Ch. 28 – Reproductive System
advertisement
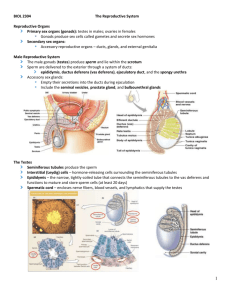
1 Ch. 28 – Reproductive System *human reproductive system produces, stores, nourishes, and transports functional male & female reproductive cells, or gametes *fertilization: also known as conception; where male & female gamete unite *all cells in human body are mitotic descendants of single zygote, cell create by fusion of sperm & ovum Overview of Reproductive System *system includes following: *gonads: reproductive organs that produce gametes & hormones *ducts that receive & transport gametes *accessory glands & organs that secrete fluids into these or other excretory ducts *perineal structures associated with reproductive system, which are collectively known as external genitalia *in adult male, testes, or male gonads, secrete sex hormones called androgens & produce about one-half billion sperm each day *during emission, mature sperm travel along lengthy duct system, where they are mixed with secretions of accessory glands mixture is known as semen *during ejaculation, semen is expelled from body *in adult female, ovaries, or female gonads, typically release only one immature gamete, or oocyte, per month *gamete travels along short uterine tubes that end in muscular uterus *vagina: short passageway that connects uterus to exterior *during sex, ejaculation introduces semen into vagina, & sperm ascend female reproductive tract *if fertilization occurs, uterus will enclose & support developing embryo as it grows into fetus & prepares for eventual delivery Reproductive System of Male *The Testes *hang within scrotum, fleshy pouch suspended inferior to perineum, anterior to anus, & posterior to base of penis *The Spermatic Cords *consist of fascia layers, tough connective tissue, & muscle enclosing blood vessels, nerves, & lymphatics that supply testes *each cord contains ductus deferens & its deferential artery, a testicular artery, the pampiniform plexus of testicular vein, & branches of genitofemoral nerve from lumbar plexus *inguinal canals form during development as testes descend into scrotum; at that time, these canals link scrotal cavities with peritoneal cavity *Descent of Testes *during development, testes form inside body cavity adjacent to kidneys *bundle of connective tissue fibers extends from each testis to posterior wall of small, anterior & inferior pocket of peritoneum constitute gubernaculum testis *as growth proceeds, gubernacula do not get any longer, & they lock testes into position *during seventh developmental month, fetal growth continues as rapid pace, & circulating hormones stimulate contraction of gubernaculum testis *during this period, each testis moves through abdominal musculature, accompanied by small pockets of peritoneal cavity process known as descent of testes 2 *body of spermatic cord formed by ductus deferens, & testicular blood vessels, nerves, & lymphatics *The Scrotum & Position of Testes *scrotum is divided internally into 2 chambers *partition between 2 is marked by raised thickening in scrotal surface known as perineal raphe *each testis lies in separate compartment, or scrotal cavity *narrow space separates inner surface of scrotum from outer surface of testis *tunica vaginalis: serous membrane lining scrotal cavity that reduces friction between opposing parietal (scrotum) & visceral (testicular) surfaces *isolated portion of peritoneum that lost its connection with peritoneal cavity after testes descended, when inguinal canal closed *scrotum consists of thin layer of skin & underlying superficial fascia *dermis contains layer of smooth muscle, dartos – resting muscle tone of dartos causes characteristic wrinkling of scrotal surface *layer of skeletal muscle, cremaster muscle, lies deep to dermis – contraction of cremaster muscle during sexual arousal, or in response to temperature changes, tenses scrotum & pulls testes closer to body *scrotum is richly supplied with sensory motor nerves from hypogastric plexus & branches of ilioinguinal nerves, genitofemoral nerves, & pudenal nerves *vascular supply to scrotum includes internal pudenal arteries, external pudenal arteries, & cremasteric branch of inferior epigastric arteries *Structure of Testes *deep to tunica vaginalis covering testis lies tunica albuginea dense layer of connective tissue rich in collagen fibers *fibers of this network are continuous with those surrounding adjacent epididymis *collagen fibers of tunica albuginea also extend into substance of testis, forming fibrous partitions, or septa *these septa converge toward area closest to entrance of epididymis – this region, located at superior end of testis is called mediastinum of testis *Histology of Testes *septa divide testis into series of lobules *roughly 800 slender tightly coiled seminiferous tubules are distributed among lobules – where sperm production occurs *each seminiferous tubule forms loop that is attached to straight tubule at mediastinum of testis *straight tubule is connected to maze of passageways known as rete testis – connected to epididymis via 15-20 large efferent ducts *each tubule is surrounded by delicate capsule, & loose connective tissue fills spaces between tubules *within these spaces are numerous blood vessels & large interstitial cells, which are responsible for production of androgens, the dominant sex hormones in male (testosterone is most important) *sperm cells, or spermatozoa, are produced by process of spermatogenesis, which begins at outermost layer of cells in seminiferous tubules & proceeds toward tubular lumen *stem cells called spermatogonia divide by mitosis to produce generations of daughter cells, some of which differentiate into spermatocytes *through meiosis, specialized form of cell division involved only in production of gametes, spermatocytes give rise to spermatids *at each step in this process, daughter cells move closer to tubular lumen *spermatids subsequently differentiate into spermatozoa – process called spermiogenesis (last step of spermatogenesis) *sustentacular cells – within seminiferous tubule; attached to tubular capsule & extend toward 3 lumen between other cell types *Spermatogenesis *involves three integrated processes: 1. Mitosis – spermatogonia undergo cell divisions throughout adult life *cell divisions produce daughter cells that are pushed toward lumen of tubule *these cells differentiate into spermatocytes that prepare to begin meiosis *product – primary spermatocyte 2. Meiosis – special form of cell division involved in gamete production *gametes contain half normal chromosome complement *as result, fusion of nuclei of sperm & ovum produces cell that has normal number of chromosomes (46) rather than twice that number *in seminiferous tubules, meiotic divisions of spermatocytes produce spermatids, or undifferentiated male gametes *product meiosis I – secondary spermatocyte *product meiosis II - spermatid 3. Spermiogenesis – spermatids are small, relatively unspecialized cells *spermatids differentiate into physically mature spermatozoa – among most highly specialized cells in body *involves major changes in spermatid’s internal & external structure *Mitosis & Meiosis *mitosis is part of process of somatic cell division, which produces two daughter cells, each containing 23 pairs of chromosomes *because daughter cells contain both members of each chromosome pair, they are called diploid cells *meiosis involves 2 cycles of cell division & produces four cells, each of which contains 23 individual chromosomes *because these cells contain only one member of each pair of chromosomes, they are called haploid cells *as cell prepares to being meiosis, DNA replication occurs within nucleus as if cell were about to undergo mitosis *as prophase if first meiotic division, meiosis I, arrives, chromosomes condense & become visible *as in mitosis, each chromosome consists of two duplicate chromatids *corresponding maternal & paternal chromosomes now come together, an event known as synapsis – involves 23 pairs of chromosomes; each member of each pair consists of 2 chromatids *matched set of four chromatids is called tetrad *some exchange of genetic material can occur between chromatids of chromosome pair at this stage of meiosis – exchange is called crossing-over *nuclear envelope disappears at end of prophase I – as metaphase I begins, tetrads line up along metaphase plate *as anaphase I begins, tetrads break up, & maternal & paternal chromosomes separate *this is major difference between mitosis & meiosis – in mitosis, each daughter cell receives one of two copies of every chromosome, maternal & paternal, but in meiosis each daughter cell receives both copies of either maternal chromosome or paternal chromosome from each tetrad *as anaphase proceeds, maternal & paternal components are randomly distributed – as result, telophase I ends with formation of two daughter cells containing unique combinations of maternal & paternal chromosomes - both cells contain 23 chromosomes 4 *because first meiotic division reduces number if chromosomes from 46 to 23, it is called reductional division – each of these chromosomes still consists of two duplicate chromatids, which will separate during meiosis II *interphase separating meiosis I & meiosis II is very brief & there is no DNA replication over this period *cell will then proceed through prophase II, metaphase II, & anaphase II *during anaphase II, duplicate chromatids separate – telophase II thus yields 4 cells, each containing 23 chromosomes *because number of chromosomes has not changed, meiosis II represents an equational division *mitotic divisions of spermatogonia produce primary spermatocytes *as meiosis begins, each primary spermatocyte contains 46 individual chromosomes *at end of meiosis I, daughter cells are called secondary spermatocytes & contain 23 chromosomes, each of which consists of pair of duplicate chromatids *for each primary spermatocyte that enters meiosis, four spermatids are produced *connection of 4 spermatids assist in transfer of nutrients & hormonal messages between cells, this helping to ensure that cells develop in synchrony *interconnections are not broken until last stages of physical maturation *Spermiogenesis *each spermatid matures into single spermatozoon, or sperm cell – process known as spermiogenesis *developing spermatocytes undergoing meiosis & spermatids undergoing spermiogenesis are surrounded by cytoplasm of sustentacular cells *as spermiogenesis proceeds, spermatids gradually develop appearance of mature spermatozoa *at spermiation, spermatozoon loses its attachment to sustentacular cell & enters lumen of seminiferous tubule *Spermatogenesis & Sustentacular Cells *Leydig cells produce testosterone, which is taken by Sertoli cell & turned into estrogen *sustentacular cells have 6 important functions that directly or indirectly affect mitosis, meiosis, & spermiogenesis within seminiferous tubules: 1. Maintenance of blood-testis barrier *seminiferous tubules are isolated from general circulation by blood-testis barrier *sustentacular cells are joined by tight junctions, forming layer that divides seminiferous tubule into outer basal compartment that contains spermatogonia & inner lumenal compartment where meiosis & spermiogenesis occurs *transport across sustentacular cells is tightly regulated so that conditions in lumenal compartment remain very stable *fluid within lumen of seminiferous tubule is produced by sustentacular cells, which also regulate fluid’s composition, blood-testis barrier is essential to preserving difference between tubular fluid & interstitial fluid 2. Support of mitosis & meiosis *spermatogenesis depends on stimulation of sustentacular cells by circulating FSH & testosterone *stimulated sustentacular cells then in some way promote division of spermatogonia & meiotic divisions of spermatocytes 3. Support of spermiogenesis *spermiogenesis requires presence of sustentacular cells *these cells surround & enfold spermatids, providing nutrients & chemical stimuli that promote development 4. Secretion of inhibin *sustentacular cells secrete inhibin, peptide hormone, in response to factors released by 5 developing sperm *faster rate of sperm production, greater amount of inhibin secreted *by regulating FSH & GnRH (gonadotropin-releasing hormone) secretion, sustentacular cells provide feedback control of spermatogenesis 5. Secretion of androgen-binding protein (ABP) *ABP binds androgens in fluid contents of seminiferous tubules *protein is thought to be important in elevating concentration of androgens within tubules & stimulating spermiogenesis 6. Secretion of Müllerian-inhibiting factor (MIF) *MIF is secreted by sustentacular cells in developing testes *hormone causes regression of fetal Müllerian ducts, passageways that, in females, participate formation of uterine tubes & uterus *Anatomy of Speratozoon *each spermatozoon has three distinct regions: *head: flattened ellipse containing nucleus with densely packed chromosomes *at tip is acrosomal cap: membranous compartment containing enzymes essential to process of fertilization *neck: short; attaches head to middle piece *neck contains both centrioles of original spermatid *mitochondria of middle piece are arranged in spiral around microtubules *mitochondrial activity provides ATP needed to move tail *tail: only flagellum in human body *unlike other, less specialized cells, mature spermatozoon lacks endoplasmic reticulum, Golgi apparatus, & many other intracellular structures *because cell does not contain glycogen or other energy reserves, it must absorb nutrients from surrounding fluid *Male Reproductive Tract *Epididymis *lies along posterior border of testis *head: portion of epididymis proximal to mediastinum of testis *receives spermatozoa from efferent ducts that connect rete testis to epididymis *body: begins distal to last efferent duct & extends inferiorly along posterior margin of testis *near inferior border of testis, number of convolutions decreases, marking start of tail *tail recurves & ascends to its connection with ductus deferens *sperm stored primarily in tail *three major functions 1. monitors & adjusts composition of tubular fluid *pseudostratified columnar epithelial lining of epididymis bears distinctive stereocilia that increase surface area available for absorption & secretion into fluid in tubule 2. acts as recycling center for damaged spermatozoa *cellular debris & damaged spermatozoa are absorbed in epididymis, & products of enzymatic breakdown are released into surrounding interstitial fluids for pickup by epididymal circulation 3. stores spermatozoa & facilitates their functional maturation *takes about 2 weeks for spermatozoa to pass through epididymis – during this period, spermatozoon completes its functional maturation *although spermatozoa leaving epididymis are mature, they are immobile 6 *to become active, motile, & fully functional, spermatozoa must undergo capacitation: activation of acrosomal cap; normally occurs in two steps: (1)spermatozoa become motile when mixed with secretions of seminal vesicles, & (2) they become capable of successful fertilization when exposed to conditions inside female reproductive tract *transport along epididymis involves some combination of fluid movement & peristaltic contractions of smooth muscle *after passing along tail of epididymis, spermatozoa enter ductus deferens *Ductus Deferens *also called vans deferens *begins at tail of epididymis & as part of spermatic cord, ascends through inguinal canal *just before it reaches prostate gland & seminal vesicles, its lumen enlarges – expanded portion known as ampulla *wall of deferens contains thick layer of smooth muscle *peristaltic contractions in this layer propel spermatozoa & fluid along duct, which is lined by pseudostratified ciliated columnar epithelium *in addition to transporting sperm, ductus deferens can store spermatozoa for several months – during this time, spermatozoa remain in state if suspended animation & have low metabolic rates *junction of ampulla with duct of seminal vesicle marks start of ejaculatory duct *this short passageway penetrates muscular wall of prostate gland & empties into urethra *Urethra *extends from urinary bladder to tip of penis *used by both urinary & reproductive systems *Accessory Glands *fluid component of semen is mixture of secretions of many different glands, each with distinctive biochemical characteristics *major functions of following glandular organs, which occur only in males, include: *activating spermatozoa *providing nutrients spermatozoa need for motility *propelling spermatozoa & fluids along reproductive tract, mainly by peristaltic contractions *producing buffers that counteract acidity of urethral & vaginal contents *Seminal Vesicles *ductus deferens on each side ends at junction between ampulla & duct that drains seminal vesicle *seminal vesicles are embedded in connective tissue on either side of midline, sandwiched between posterior wall of bladder & rectum *body of gland has many short branches *entire assemblage is coiled & folded into compact, tapered mass *extremely active secretory glands with epithelial lining that contains extensive folds *contribute about 60% of volume of fluid *secretion of seminal vesicles contains: *relatively high concentrations of fructose, which is easily metabolized by spermatozoa *prostaglandins, which may stimulate smooth muscle contractions along male & female reproductive tracts *fibrinogen, which after ejaculation will form temporary clot with vagina; clot will alow for capacitation *secretions are slightly alkaline helps neutralize acids in prostatic secretions & within vagina *when mixed with secretions from seminal vesicles, previously inactive but functional spermatozoa begin beating their flagella, becoming highly mobile *secretions are discharged into ejaculatory duct at emission, when peristaltic contractions are under way in ductus deferens, seminal vesicles, & prostate gland 7 *Prostate Gland *small, muscular, rounded organ that encircles proximal portion of urethra as it leaves urinary bladder *glandular tissue of prostate consists of cluster of 30-50 compound tubuloalveolar glands, which are surrounded by & wrapped in thick blanket of smooth muscle fibers *prostatic glands produce prostatic fluid, slightly acidic solution that contributes 20-30% of volume of semen *secretions contain seminalplasmin, an antibiotic that may help prevent urinary tract infections in males ejected into prostatic urethra by peristaltic contractions of muscular wall *Bulbourethral Glands *Cowper’s glands; paired glands situated at base of penis, covered by fascia of urogenital diaphragm *duct of each gland travels alongside penile urethra for 3-4cm before emptying into urethral lumen *these are compound, tubuloalveolar mucous glands that secrete thick, alkaline mucus *secretion helps neutralize any urinary acids that may remain in urethra & provides lubrication for glans, tip of penis *Semen *typical ejaculation releases 2-5ml of semen *volume of fluid, called ejaculate, contains: *spermatozoa *normal sperm count ranges from 20-100 million spermatozoa per milliliter *seminal fluid *fluid component of semen – mixture of glandular secretions with distinct ionic & nutrient composition *typical sample of seminal fluid contains secretions of seminal vesicles (60%), prostate (30%), sustentacular cells & epididymis (5%), & bulbourethral glands (less than 5%) *enzymes *several important enzymes are present in seminal fluid including: (1) protease that may help dissolve mucous secretions in vagina, (2) seminalplasmin, an antibiotic enzyme from prostate gland that kills variety of bacteria, including Escherichia coli, (3) prostaic enzyme that converts fibrinogen to fibrin after ejaculation, & (4) fibrinolysin, which subsequently liquefies clotted semen *Penis *tubular organ through which distal portion of urethra passes *conducts urine to exterior & introduces semen into female vagina during sexual intercourse *divided into three regions: *root: fixed portion that attaches penis to body wall *connection occurs within urogenital triangle immediately inferior to pubic symphysis *body (shaft):tubular, movable portion *masses of erectile tissue are found within body *glans: expanded distal end that surrounds external urethral meatus *neck – narrow portion of penis between shaft & glans *skin overlying penis resembles that of scrotum *dermis contains layer of smooth muscle, & underlying loose connective tissue allows thin skin to move without distorting underlying structures *fold of skin called prepuce or foreskin surrounds tip of penis *attaches to relatively narrow neck & continues over glans *no hair follicles on opposing surfaces, but preputial glands of skin of neck & inner surface of prepuce secrete waxy material known as smegma, which is an excellent nutrient source for bacteria *circumcision: surgical removal of prepuce 8 *beneath loose connective tissue, dense network of elastic fibers encircles internal structures of penis *most of body of penis consists of three cylindrical columns of erectile tissue: consists of 3D maze of vascular channels incompletely separated by partitions of elastic connective tissue & smooth muscle fibers *in resting state, arterial branches are constricted, & muscular partitions are tense, restricting blood flow into erectile tissue *smooth muscles in arterial walls relax when NO is released at which time (1) vessels dilate, (2) blood flow increases, (3) vascular channels become engorged with blood, & (4) erection of penis occurs *on anterior surface of flaccid penis, 2 cylindrical corpus cavernosa are separated by thin septum & encircled by dense collagenous sheath *diverge at their bases, forming crura of penis – each is bound to ramus of ischium & pubis by tough connective tissue ligaments *extend along length of penis as far as neck *surrounds central artery *relatively slender corpus spongiosum surrounds penile urethra *this erectile body extends from superficial fascia of urogenital diaphragm to tip of penis, where it expands to form glans *sheath surrounding spongiosum contains more elastic fibers than does that of cavernosa, & erectile tissue contains pair of small arteries *Hormones & Male Reproductive Function *anterior pituitary release FSH & LH *pituitary release of these hormones occurs in presence in gonadotropin-releasing hormone (GnRH), a peptide synthesized in hypothalamus & carried to anterior pituitary by hypophyseal portal system *GnRH secretion occurs in pulses rather than continuously *as levels of GnRH change, so do rates of secretion of FSH & LH *FSH & Spermatogenesis *in males, FSH mainly targets sustentacular cells of seminiferous tubules *under FSH stimulation, & in presence of testosterone from interstitial cells, sustentacular cells (1) promote spermatogenesis & spermiogenesis, & (2) secrete androgen-binding protein *rate of spermatogenesis is regulated by negative feedback mechanism involving GnRH, FSH, & inhibin *when FSH levels become elevated, inhibin production increases until FSH levels return to normal *LH & Androgen Production *in males, LH causes secretion of testosterone & other androgens by interstitial (Leyidg) cells of testes *testosterone, most important androgen, has numerous functions including: *stimulating spermatogenesis & promoting functional maturation of spermatozoa, through its effects on sustentacular cells *affecting CNS function, including influence of libido & related behaviors *stimulating metabolism throughout body, especially pathways concerned with protein synthesis & muscular growth *establishing & maintaining secondary sex characteristics, such as distribution of facial hair, increased muscle mass & body size, & quantity & location of characteristic adipose tissue deposits *maintaining accessory glands & organs of male reproductive tract *testosterone circulates which bound to transport proteins; gonadal steroid-binding globulin (GBG) carries roughly 2/3 of circulating testosterone, & rest binds to albumins *diffuses across cell membrane & binds to intracellular receptor *in many target tissues, some of arriving testosterone is converted to dihyrotestosterone (DHT) 9 *early surge of testosterone levels stimulates differentiation of male duct system & accessory organs & affects CNS development Reproductive System of Female *woman’s reproductive system must produce sex hormones & functional gametes & must be able to protect & support developing embryo & nourish newborn infant *ovaries, uterine tubes, & uterus are enclosed within extensive mesentery known as broad ligament *uterine tubes run along superior border of broad ligament & open into pelvic cavity lateral to ovaries *mesovarium: thickened fold of mesentery that supports & stabilizes position of each ovary *broad ligament attaches to sides & floor of pelvic cavity, where it becomes continuous with parietal peritoneum *pocket formed between posterior wall of uterus & anterior surface of colon is rectouterine pouch; that formed between uterus & posterior wall of bladder is vesicouterine pouch *Ovaries *small, paired, almond-shaped organs located near lateral walls of pelvic cavity *functions include: *producing immature female gametes, or oocytes *secreting female sex hormones, including estrogens & progestins *secrete inhibin, involved in feedback control of pituitary FSH production *position of each ovary is stabilized by mesovarium & by pair of supporting ligaments: *ovarian ligament: extends from uterus, near attachment of uterine tube, to medial surface of ovary *suspensory ligament: extends from lateral surface of ovary past open end of uterine tube to pelvic wall *contains major blood vessels of ovary, ovarian artery, & ovarian vein *these vessels are connected to ovary at ovarian hilus where ovary attaches to mesovarium *pink or yellowish & has nodular consistency *visceral peritoneum, or germinal epithelium, covering surface of each ovary consists of layer of columnar epithelial cells that overlies dense connective tissue layer called tunica albuginea *interior tissues, or stroma, can be divided into superficial cortex (where gametes are produced) & deeper medulla *Oogenesis *ovum production, or oogenesis begins before woman’s birth *oogonia, or stem cells of females, complete their maturation before birth *between third & seventh months of fetal development, daughter cells, or primary oocytes, prepare to undergo mitosis *they proceed as far as prophase of meiosis I, but at that time process comes to halt *primary oocytes then remain in state of suspended development until individual reaches puberty *at that time, rising levels of FSH trigger start of ovarian cycle *not all primary oocytes produced in development survive until puberty (only about 400,000 of the 2 million produced initially) *those that don’t survive degenerate in process called atresia *meiosis in ovaries is same as in testes with exception of 2 important details: 1. cytoplasm of primary oocyte is unevenly distributed during 2 meiotic divisions *oogenesis produces one functional ovum, which contains most of original cytoplasm, & 2 or 3 nonfunctional polar bodies that later disintegrate 2. ovary releases secondary oocyte rather than mature ovum *secondary oocyte is suspended in metaphase of meiosis II; meiosis will not be completed unless & until fertilization *Ovarian Cycle 10 *ovarian follicles: specialized structures in which oocyte growth & meiosis I occur *located in cortex of ovaries *primary oocytes are located in outer portion of ovarian cortex near tunica albuginea, in clusters called egg nests *each primary oocyte in egg nest is surrounded by single squamous layer of follicular cells *primary oocyte & its follicular cells form primordial follicle *after sexual maturation, different group of primordial follicles is activated each month process called ovarian cycle *cycle can be divided into follicular phase, or preovulatory phase, & luteal phase, or postovulatory phase *STEP 1: Formation of primary follicles *follicle formation is stimulated by FSH *cycle begins as activated primordial follicles develop into primary follicles *in primary follicle, follicular cells enlarge & undergo repeated cell division *these divisions create several layers of follicular cells around oocyte cells now called granulosa cells *as layers of granulosa cells develop around primary oocyte, microvilli from surrounding granulosa cells intermingle with those of primary oocyte *microvilli are surrounded by layer of glycoproteins, & entire region is called zona pellucida *microvilli increase surface area available for transfer of materials from granulosa cells to rapidly enlarging oocyte *as granulosa cells enlarge & multiply , adjacent cells in ovarian stroma form layer of thecal cells around follicle *thecal cells & granulosa cells work together to produce sex hormones called estrogen *STEP 2: Formation of secondary follicles *transformation begins as wall of follicle thickens & granulosa cells begin secreting small amounts of fluid called follicular fluid, or liquor fluid, that accumulates in small pockets & gradually expands & separates inner & outer layers of follicle *at this stage, complex is called secondary follicle *although primary oocyte continues to grow at steady pace, follicle as whole now enlarges rapidly because follicular fluid accumulates *STEP 3: Formation of tertiary follicle *8 to 10 days after start of ovarian cycle, ovaries generally contain only single secondary follicle destined for further development *by 10 to 14 day of cycle, follicle has formed tertiary follicle, or mature Graafian follicle *this complex spans entire width of ovarian cortex & distorts ovarian capsule, creating prominent bulge in surface of ovary *oocyte projects into expanded central chamber, antrum of follicle surrounded by mass of granulosa cells *as tertiary follicle completes its development, LH levels begin to rise, & primary oocyte completes meiosis I *secondary oocyte then enters meiosis II but stops once again on reaching metaphase; meiosis II will not be completed unless fertilization occurs *as time of ovulation approaches, secondary oocyte & surrounding granulosa cells lose their connections with follicular wall & drift free within antrum – generally occurs on day 14 of 28-day cycle *granulosa cells immediately surrounding secondary oocyte are now known as corona radiata *STEP 4: Ovulation *ovulation: when tertiary follicle releases secondary oocyte *distended follicular wall ruptures, releasing follicular contents, including secondary oocyte & 11 corona radiata, into pelvic cavity *sticky follicular fluid keeps corona radiata attached to surface of ovary, where direct contact with projections of uterine tube or with fluid currents established by their ciliated epithelium can transfer secondary oocyte to uterine tube *STEP 5: Formation & degeneration of corpus luteum *empty tertiary follicle initially collapses, & ruptured vessels bleed into antrum *remaining granulosa cells then invade area, proliferating to create endocrine structure known as corpus luteum, named for its yellow color process occurs under LH stimulation *lipids contained in corpus luteum are used to manufacture steroid hormones known as progestins, principally steroid progesterone *progesterone’s principal function is to prepare uterus for pregnancy by stimulating maturation of uterine lining & secretions of uterine glands *STEP 6: Unless pregnancy occurs, corpus luteum begins to degenerate roughly 12 days after ovulation *progesterone & estrogen levels then fall markedly *fibroblasts invade nonfunctional corpus luteum, producing knot of pale scar tissue called corpus albicans *disintegration, or involution, or corpus luteum marks end of ovarian cycle *Uterine Tubes *each is hollow, muscular tube, divided into three regions: *infundibulum: expanded funnel end closest to ovary; has numerous fingerlike projections that extend into pelvic cavity *projections are called fimbriae *inner surfaces of infundibulum are lined with cilia that beat toward middle segment of uterine tube, ampulla *ampulla: middle segments whose thickness of smooth muscle layer in wall gradually increases as it approaches uterus *isthmus: short segment connected to uterine wall; where ampulla leads *Histology of Uterine Tube *epithelium lining uterine tube is composed of ciliated columnar epithelial cells with scattered mucin-secreting cells *mucosa is surrounded by concentric layers of smooth muscle *oocyte transport involves combination of ciliary movement & peristaltic contractions in walls of uterine tube *uterine tube transports secondary oocyte for final maturation & fertilization – normally takes 3-4 days for oocyte to travel from infundibulum to uterine cavity *tube also provides nutrient-rich environment that contains lipids & glycogen *this mixture provides nutrients to both spermatozoa & developing pre-embryo *The Uterus *provides mechanical protection, nutritional support, & waste removal for developing embryo & fetus *contractions in muscular wall of uterus are important in ejecting fetus at time of birth *small, pear-shaped organ that bends anteriorly near its base, a condition known as anteflexion *body of uterus lies across superior & posterior surfaces of bladder *Suspensory Ligaments of Uterus *in addition to broad ligament, three pairs of suspensory ligaments stabilize position of uterus & limit its range of movement *uterosacral ligaments: extend from lateral surfaces of uterus to anterior face of sacrum, keeping body from moving inferiorly & anteriorly *round ligaments: arise on lateral margins of uterus just posterior & inferior to attachments of uterine tubes; restrict primarily posterior movement of uterus 12 *lateral ligaments: extend from base of uterus & vagina to lateral walls of pelvis; tend to prevent inferior movement of uterus *additional mechanical support is provided by skeletal muscles & fascia on pelvic floor *Internal Anatomy of Uterus *body, or corpus, is largest region of uterus *fundus: rounded portion of body superior to attachment of uterine tubes *body ends at constriction known as uterine isthmus *cervix: inferior portion of uterus that extends from isthmus to vagina *within vagina, distal end of cervix forms curving surface that surrounds cervical os, or external orifice of uterus *cervical os leads into cervical canal, a constricted passageway that opens into uterine canal of body at internal os, or internal orifice *uterus receives blood from branches of uterine arteries, which arise from branches of internal iliac arteries & ovarian arteries, which arise from abdominal aorta inferior to renal arteries *there are extensive interconnections among arteries to uterus – arrangement helps to ensure reliable flow of blood to organ despite changes in position & changes in uterine shape that accompany pregnancy *Uterine Wall *wall has thick, outer, muscular myometrium & thin, inner, glandular endometrium (10% of uterine mass), or mucosa *fundus & posterior surface of uterine body & isthmus are covered by serous membrane continuous with peritoneal lining this incomplete serosa is called perimetrium *glandular & vascular tissues of endometrium support physiological demands of growing fetus *myometrium, thickest portion of uterine wall, forms almost 90 % of mass of uterus *smooth muscle in myometrium is arranged into longitudinal, circular, & oblique layers *smooth muscle tissue provides much of force needed to move large fetus out of uterus & into vagina *Histology of uterus *endometrium can be divided into: *functional zone: layer closest to uterine cavity *contains most of uterine glands & contribute most to endometrial thickness *basilar zone: outer layer adjacent to myometrium *attaches endometrium to myometrium & contains terminal branches of tubular glands *within myometrium, branches of uterine arteries form arcuate arteries that encircle endometrium *radial arteries supply straight arteries that deliver blood to basilar zone of endometrium & spiral arteries that supply functional zone *structure of basilar zone remains relatively constant over time, but that of functional zone undergoes cyclical changes in response to sex hormone levels *Uterine Cycle *menstrual cycle, repeating series of changes in structure of endometrium *entire cycle averages about 28 days *cycle can be divided into 3 phases: (1) menses, (2) proliferative phase, & (3) secretory phase *phases occur in response to hormones associated with regulation of ovarian cycle *menses & proliferative phase occur during follicular phase of cycle *secretory phase corresponds to luteal phase of cycle *Menses *cycle begins with onset on menses, interval marked by degeneration of functional zone of endometrium *deterioration occurs in patches & is caused by constriction of spiral arteries, which reduces blood flow to certain parts of endometrium 13 *deprived of oxygen & nutrients, secretory glands & other tissues of functional zone begin to deteriorate *blood cells & degenerating tissues break away & enter uterine lumen, to be lost by passage through cervical os & into vagina *sloughing of tissue is glandular, & at each site, repairs begin almost at once *before menses has ended, entire functional zone has been lost process called menstruation *menstruation generally lasts 1-7 days, & over this period roughly 35-50 mL of blood is lost *Proliferative Phase *after menses, epithelial cells of glands multiply & spread across endothelial surface, restoring integrity of uterine epithelium *further growth & vascularization result in complete restoration of functional zone *as this reorganization proceeds, endometrium is said to be in proliferative phase *stimulated & sustained by estrogens secreted by developing ovarian follicles *by time ovulation occurs, functional zone is several mm thick & prominent mucous glands extend to border with basilar zone *at this time, endometrial glands are manufacturing mucus rich in glycogen *entire functional zone is highly vascularized, with small arteries spiraling toward inner surface from larger arteries in myometrium *under control of high levels of estrogen, which causes contractions in uterus to help sperm travel through uterus to fallopian tubes *Secretory Phase *during this phase, endometrial glands enlarge, accelerating their rates of secretion, & arteries elongate & spiral through tissues of functional zone *this activity occurs under compound stimulatory effects of progestins & estrogens from corpus luteum *this phase begins at time of ovulation & persists as long as corpus luteum remains intact *secretory activities peak about 12 days after ovulation *over next day or two, glandular activity declines, & uterine cycle comes to close as corpus luteum stops producing stimulatory hormones *estrogen levels decrease, progesterone levels increase, stopping uterine contractions & preparing for implantation *Menarche & Menopause *cycle begins with menarche, or first menstrual period at puberty, typically at age 11-12 *cycle continues until age 45-55, when menopause, last uterine cycle, occurs *The Vagina *elastic, muscular tube extending between cervix of uterus & vestibule, space bounded by female external genitalia *at proximal end of vagina, cervix projects into vaginal canal *shallow recess surrounding cervical protrusion is known as fornix *vagina lies parallel to rectum, & 2 are in close contact posteriorly *primary blood supply to vagina is via vaginal branches of internal iliac arteries & veins *three major functions include: *serves as passageway for elimination of menstrual fluids *receives penis during sexual intercourse & holds spermatozoa prior to their passage into uterus *forms lower portion of birth canal, through which fetus passes during delivery *Histology of Vagina *vaginal walls contain network of blood vessels & layers of smooth muscle *lining is moistened by secretions of cervical glands & by movement of water across permeable epithelium 14 *vagina & vestibule are separated by hymen, an elastic epithelial fold that partially or completely blocks entrance to vagina before onset of sexual intercourse *two bulbospongiosus muscles extend along either side of vaginal entrance, & their contractions constrict entrance *these muscles cover vestibular bulbs, masses of erectile tissue on either side of vaginal entrance *vaginal lumen is lined by nonkeratinized stratified squamous epithelium that in relaxed state is thrown into folds called rugae *underlying lamina propia is thick & elastic, & it contains small blood vessels, nerves, & lymph nodes *vaginal mucosa is surrounded by elastic muscularis layer, with layers of smooth muscle fibers arranged in circular & longitudinal bundles continuous with uterine myometrium *portion of vagina adjacent to uterus has serosal covering continuous with pelvic peritoneum *vagina contains population of resident bacteria, usually harmless, supported by nutrients in cervical mucus *metabolic activity of these bacteria creates acidic environment, which restricts growth of many pathogens *hormonal changes associated with ovarian cycle also have effect on vaginal epithelium *External Genitalia *vulva: region containing female external genitalia; also called pudendum *vagina opens into vestibule, a central space bounded by small folds known as labia minora, which are covered by smooth hairless skin *urethra opens into vestibule just anterior to vaginal entrance *paraurethral glands: Skene’s glands; discharge into urethra near external urethral opening *clitoris: projects into vestibule, anterior to urethral opening *small, rounded tissue projection; female equivalent to male penis *internally it contains erectile tissue comparable to corpura cavernosa of penis *engorges with blood during sexual intercourse *small erectile glans sits atop organ; extensions of labia minora encircle body of clitoris forming prepuce, or hood of clitoris *variable number of small lesser vestibular glands discharge their secretions onto exposed surface of vestibule, keeping it moistened *during arousal, pair of ducts discharges secretions of greater vestibular glands into vestibule near posterolateral margins of vaginal entrance *outer limits of vulva are established by mons pubis & labia majora *bulge of mons pubis is created by adipose tissue beneath skin anterior to pubis symphysis *adipose tissue also accumulates in labia majora, prominent folds of skin that encircle & partially conceal labia minora & adjacent structures *outer margins of labia majora & mon pubis are covered with coarse hair, but inner surfaces of labia majora are relatively hairless *sebaceous glands & scattered apocrine sweat glands secrete onto inner surface of labia majora, moistening them & providing lubrication *Mammary Glands *mammary glands: secrete milk for nourishment of newborn baby *lactation: milk production; occurs in mammary glands *glands are specialized organs of integumentary system that are controlled primarily by hormones of reproductive system & placenta, temporary structure that provides embryo or fetus with nutrients *on each side, mammary gland lies in subcutaneous tissue of pectoral fat pad beneath skin of chest *reddish brown region around skin of each nipple is areola: grainy texture due to large sebaceous glands beneath it *glandular tissue of gland consists of separate lobes, each containing several secretory lobules 15 *ducts leaving lobules converge, giving rise to single lactiferous duct in each lobe *near nipple, lactiferous duct enlarges, forming expanded chamber called lactiferous sinus *dense connective tissue surrounds duct system & forms partitions that extend between lobes & lobules bands of connective tissue are known as suspensory ligaments of breast *layer of loose connective tissue separates mammary complex from underlying pectoralis muscles *branches from internal thoracic artery supply blood to each gland *Development of mammary glands during pregnancy *size of mammary gland in non-pregnant woman reflects primarily amount of adipose tissue present, not amount of glandular tissue *secretory apparatus does not complete its development until pregnancy occurs *active mammary gland is tubuloalveolar gland, consisting of multiple glandular tubes that end in secretory alveoli *Hormones & Female Reproductive System *activity of female reproductive tract is under hormonal control that involves interplay between pituitary & gonadal secretions *circulating hormones control female reproductive cycle, coordinating ovarian & uterine cycles to ensure proper reproductive function *GnRH from hypothalamus regulates reproductive function in females *unlike in males, GnRH pulse frequency and amplitude change throughout course of ovarian cycle *changes in GnRH pulse frequency are essential to normal FSH & LH production & thus to normal ovulation; frequencies are controlled primarily by circulating levels of estrogens (increase) & progestins (decrease) *cells responsible for FSH & LH production are called gonadotropes *Hormones & Follicular Phase *follicular development begins under FSH stimulation *as follicles enlarge, thecal cells start producing androstenedione, steroid hormone that is key intermediate in synthesis of most sex hormones; absorbed by granulosa cells & converted to estrogens *3 estrogens are in circulation: estradiol, estrone, & estriol – all have similar effects of target tissues *estradiol: most abundant estrogen whose effects of targets tissues are most pronounced *dominant hormone prior to ovulation *estrogens have multiple functions, affecting activities of many different tissues & organs throughout body: 1. stimulating bone & muscle growth 2. maintaining female secondary sex characteristics such as body hair distribution and location of adipose tissue deposits 3. affecting CNS activity (especially in hypothalamus, where it increases sexual drive) 4. maintaining functional accessory reproductive glands & organs 5. initiating repair & growth of endometrium *early in follicular phase, estrogen levels are low & GnRH pulse frequency is 16-24 per day *at this frequency, FSH is dominant hormone released by anterior pituitary gland *estrogen released by developing follicles inhibits LH secretion *as secondary follicles develop, FSH levels decline due to negative feedback effects of inhibin *follicular development & maturation continues, however, supported by combination of estrogens, FSH, & LH *as one or more tertiary follicles begin forming, concentration of circulating estrogens rises steeply *as result, GnRH pulse frequency increases to about 36 per day increase stimulates LH secretion *in addition, effect of estrogen on LH secretion changes from inhibition to stimulation 16 *high estrogen levels also increase gonadotrope sensitivity to GnRH *at about day 14 of cycle, estrogen levels have peaked causing massive release LH from anterior pituitary *sudden surge in LH concentration triggers: (1) completion of meiosis I by primary oocyte, (2) rupture of follicular wall, & (3) ovulation *Hormones & Luteal Phase *high LH levels that trigger ovulation also promote progesterone (main hormone of luteal phase) secretion & formation of corpus luteum *as progesterone levels rise & estrogen levels fall, GnRH pulse frequency declines sharply which stimulates LH secretion more than it does FSH secretion, & LH maintains structure & secretory function of corpus luteum *progesterone’s primary function is to continue preparation of uterus for pregnancy by promoting degeneration of corpus luteum & elaboration of blood supply to functional zone & stimulating secretion of endometrial glands *drop in progesterone causes sloughing of functional zone *when pregnant – embryo secretes HCG, which stops regression of corpus luteum & maintains progesterone levels *rising levels of estrogen & progesterone during 36 weeks makes everything get big *Hormones & Uterine Cycle *declines in progesterone & estrogen levels that accompany degeneration of corpus luteum result in menses *sloughing of endometrial tissue continues for several days, until rising estrogen levels stimulate repair & regeneration of functional zone of endometrium *proliferative phase continues until rising progesterone levels mark arrival of secretory phase *combination of estrogen & progesterone then causes enlargement of endometrial glands & increase in their secretory activities *Hormones & Body Temperature *monthly hormonal fluctuations cause physiological changes that affect core body temperature *during follicular phase, when estrogen is dominant hormone, basal body temperature, or resting body temperature measured on awakening in morning is about .3°C lower than it sis during luteal phase when progesterone is dominant phase *at time of ovulation, basal body temperature declines noticeably, making rise in temperature over following day even more noticeable Physiology of Sexual Intercourse *sexual intercourse: also called coitus or copulation, introduces semen into female reproductive tract *Male Sexual Function *coordinated by complex neural reflexes that utilize sympathetic & parasympathetic division of ANS *during arousal, erotic thoughts, stimulation of sensory nerves in genital region, or both lead to increase in parasympathetic outflow over pelvic nerves which leads to erection of penis *during intercourse, sensory receptors of penis are rhythmically stimulated stimulation eventually results in coordinated processes of emission & ejaculation *emission: occurs under sympathetic stimulation *process begins when peristaltic contractions of ampulla push fluid & spermatozoa into prostatic urethra *seminal vesicles then begin contracting, & contractions increase in force & duration over next few seconds *peristaltic contractions also occur within walls of prostate gland *combination moves seminal mixture into membranous & penile portions of urethra 17 *combination of elevated pressure inside bladder & contraction of internal urethral sphincter effectively prevents passage of semen into bladder *ejaculation: occurs as powerful, rhythmic contractions appear in ischiocavernosus & bulbospongiosus muscles, 2 superficial skeletal muscles of pelvis floor *ischiocavernosus muscle contractions serve primarily to stiffen organ *bulbospongiosus muscle contraction pushes semen toward external urethral opening *these contractions are controlled by somatic motor neurons in lower lumbar & upper sacral segments of spinal cord *associated with intensely pleasurable sensations, known as orgasm *temporary increases in heart rate & blood pressure *Female Sexual Function *during sexual arousal, parasympathetic activation leads to engorgement of erectile tissues of clitoris & increase secretion of cervical mucous glands & greater vestibular glands *clitoral erection increases receptors’ sensitivity to stimulation, & cervical & vestibular glands provide lubrication for vaginal walls *during sexual intercourse, rhythmic contact of penis with clitoris & vaginal walls, reinforced by touch sensations from breasts & other stimuli, provides stimulation that eventually lead to orgasm *female orgasm is accompanied by peristaltic contractions of uterus & vaginal walls, & by means of impulses traveling over pudendal nerves, rhythmic contractions of bulbospongiosus & ischiocavernosus muscles (latter contractions give rise to sensations of orgasm) Aging & Reproductive System *Menopause *usually defined as time ovulation & menstruation cease *typically occurs at age 45-55, but in years preceding it ovarian & uterine cycles become irregular – interval known as perimenopause *shortage of primordial follicles is underlying cause of cycle irregularities *as number of available follicles decreases, levels of estrogen decline & may fail to rise enough to trigger ovulation *accompanied by decline in circulating concentrations of estrogen & progesterone & sharp & sustained rise in production of GnRH, FSH, & LH *decline in estrogen levels leads to reductions in size of uterus & breasts, accompanied by thinning of urethral & vaginal epithelia *reduced estrogen concentrations have also been linked to development of osteoporosis, presumably because bone deposition proceeds at slower rate *Male Climacteric *changes in male reproductive system occur more gradually than do those in female reproductive system *period of change is known as male climacteric *levels of testosterone begin to decline at age 50 & 60, & levels of circulating FSH & LH increase