Lab 2: Tissue Processing
advertisement
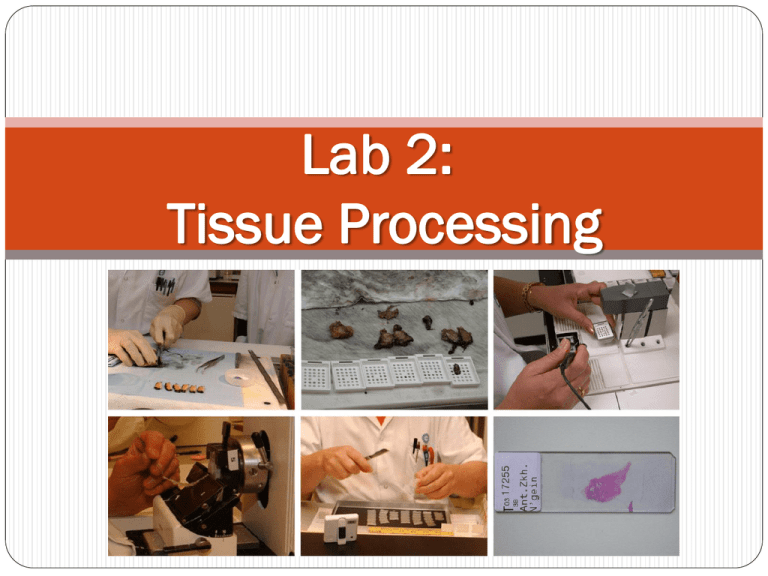
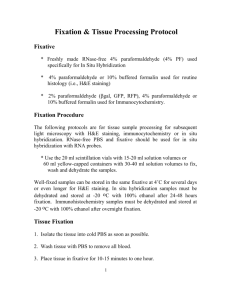
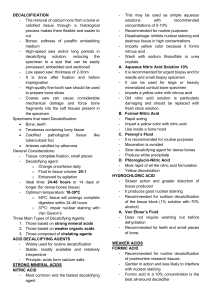
Lab 2: Tissue Processing Objectives What is tissue processing? What are the major steps in tissue processing? Identify types of fixative. The advantage of each fixative. The disadvantage of each fixative. What chemical or alterations that can be done to improve tissue processing? Overview Those who are unfamiliar with histotechnology often ask, “How does a pathologist look at a biopsy under the microscope and diagnose a disease ? ” The process is long and involved, and each sequential step is completely dependent on the previous one. The majority of surgical tissue is treated with various reagents used to preserve tissue elements (such as nuclei, cytoplasm, and tissue morphology) and prepare the specimen for paraffin embedding and microtomy. Cont. Preparing fresh tissue samples for microscopic use has many steps, such as fixation and processing, embedding and microtomy, de-paraffinization and staining, and finally cover slipping. Tissue Processing The term tissue processing refers to treatment of the tissue necessary to impregnate it into a solid medium, so that the tissue is rendered sufficiently firm yet elastic for the tissue sections of desirable thickness to be cut on microtome. Histopathological Technique Histopathological technique deals with the preparation of tissue for microscopic examination. The aim of good histological technique to preserve microscopic anatomy of tissue and make them hard, so that very thin section (4 to 5 micron) can be made. After staining, the section should represent the anatomy of the tissue as close to as possible to their structure in life. These processes are Fixative Staining Dehydration Cutting Clearing Embedding Fixation Cover slipping Staining Hydration Dehydration Tissue Processing Deparaffinized Clearing Impregnating in paraffin wax Embidding Cutting 1. Fixative This is the process by which the constituents of cells and tissue are fixed in a physical and partly also in a chemical state so that they will withstand subsequent treatment with various reagents with minimum loss of architecture. This is achieved by exposing the tissue to chemical compounds, call fixatives. Mechanism of action of fixatives Most fixatives act by denaturing or precipitating proteins which then form a sponge or meshwork, tending to hold the other constituents. Good fixative is most important factors in the production of satisfactory results in histopathology. No fixative will penetrate a piece of tissue thicker than 1 cm. Properties of an Ideal Fixative: 1. Prevents autolysis and bacterial decomposition. 2. Preserves tissue in their natural state and fix all components. 3. Make the cellular components insoluble to reagent used in tissue processing. 4. Preserves tissue volume. 5. Avoid excessive hardness of tissue. 6. Allows enhanced staining of tissue. 7. Should be non-toxic and non-allergic for user. 8. Should not be very expensive. Factor affecting fixation: 1. Size and thickness of piece of tissue. 2.Tissue covered by large amount of mucous fix slowly. 3. The same applies to tissue covered by blood or organ containing very large amount of blood. 4. Fatty and lipomatous tissue fix slowly. 5.Correct choice of fixatives. 6. Fixation is accelerated by maintaining temperature around 60Co. Formaldehyde The most commonly used fixative is formalin. It is prepared by mixing 40% formaldehyde gas in 100w/v of distilled water. Routinely, 10% formalin is used. Mechanism of action It forms cross links between amino acids of protein thereby making them insoluble. Cont. Advantages: 1. Rapid penetration. 2. Easy availability & cheap. 3. Does not over harden the tissue. 4. Fixes lipids for frozen sections Disadvantages: 1. Irritant to the nose, the eyes and mucus membranes. 2. Formation of precipitate of paraformaldehyde which can be prevented by adding 11-165 methanol. 3. Formation of black formalin pigment, Acid formaldehyde hematin. Alcohol (Ethyl Alcohol) Absolute alcohol alone has very little place in routine fixation for histopathology. It acts as a reducing agents, become oxidized to acetaldehyde and then to acetic acid. Cont. Advantages: -Alcohol penetrates rapidly in presence of other fixative hence in combination e.g. Carnoy's fixative is used to increase the speed of tissue processing. -Ethanol preserves some proteins in relatively undenatured state so that it can be used for immunofluorescence or some histochemical methods to detect certain enzymes. -Methyl alcohol is used for fixing blood and bone marrow smears. Cont. Disadvantages: -It is slow to penetrate, hardens and shrinks the tissue. Acetone Cold acetone is sometimes used as a fixative for the histochemical demonstration of some tissue enzymes like phosphatases and lipases. Its mode of action as fixative is similar to that of alcohol. Mercuric Chloride (HgCl2) Advantages: -It penetrates rapidly without destroying lipids. Disadvantages: -It causes shrinkage of the tissue if it used alone. -It brings about precipitation of the proteins. Note: Treatment of the tissue with mercuric chloride brings out more brilliant staining with most of the dyes. Picric acid Advantages: -It penetrates well and fixes rapidly. Disadvantages: -It produces marked cells shrinkage hence it is not used alone. -It precipitates proteins and combines with them to form picrate's some of the picrate's are water-soluble so must be treated with alcohol before further processing where the tissue comes into contact with water. Cont. Note: All the tissues fixed in picric acid containing fixatives should be thoroughly washed to remove the yellow discoloration to ensure proper staining of tissue sections. If the fixative is not removed by washing thoroughly with time even the embedded tissue loses its staining quality. Potassium dichromate It fixes the cytoplasm without precipitation. Valuable in mixtures for the fixation of lipids especially phospholipids. Used for fixing phosphatides and mitochondria. Note: Thorough washing of the tissue fixed in dichromate is required to avoid forming an oxide in alcohol which cannot be removed later. 2. Dehydration Tissues are dehydrated by using increasing strength of alcohol; e.g. 50%, 70%, 90% and 100%. The duration for which tissues are kept in each strength of alcohol depends upon the size of tissue, fixative used and type of tissue; e.g. after fixation in aqueous fixative delicate tissue need to be dehydrated slowly starting in 50% ethyl alcohol directly whereas most tissue specimens may be put into 70% alcohol. Delicate tissue will get high degree of shrinkage by two great concentration of alcohol. Cont. Note : If the water is one of the fixative components must be the work of dehydration step after the fixation process while the water was not a contents do not need to perform this step. 3. Clearing During dehydration water in tissue has been replaced by alcohol. The next step alcohol should be replaced by paraffin wax. As paraffin wax is not alcohol soluble, we replace alcohol with a substance in which wax is soluble. This step is call clearing. Impregnating in Paraffin Wax? Types ofWax employed for Impregnation: 1. Paraffin wax 2.Water soluble wax 3. Other material, like colloidin, gelatin, paraplast etc. Paraffin wax is used routinely. It has hard consistency, so section of 7 micron thickness can be cut. 4. Blocking Impregnated tissues are placed in a mould with their labels and then fresh melted wax is poured in it and allowed to settle and solidify. Once the block has cooled sufficiently to form a surface skin it should be immersed in cold water to cool it rapidly. After the block has completely cooled it is cut into individual blocks and each is trimmed. 5. Decalcification Loss of calcium salts from a bone or tooth OR the process of removing calcareaous matter. Methods of decalcification: Acid decalcifying agents Iron exchange resins with acid and decalcifying fluids Electrolytic decalcification Chelating agents Cont. Acid decalcifying agents The commonest method of decalcification is dissolving calcium salts in an acid solution. Some of the acid decalcifying agents are (Nitric acid, Formic acid and Trichloroacetic acid) Ion exchange with acid and decalcifying fluids The removal of calcium ions from the decalcifying fluid by the resins leads to quicker and more efficient decalcification. Cont. Electrolytic decalcification It is the speedier decalcification without damage to cytological features and staining. Chelating agents EDTA is a chelating agent, it is a white crystalline powder soluble in distilled water to about 20%. As a decalcifying agent it combines with calcium ions to form soluble, non-ionized compound. The volume of solution for decalcifying should be 150 times that of the tissue. The solution should be renewed every 5to7 days during decalcification. Cont.