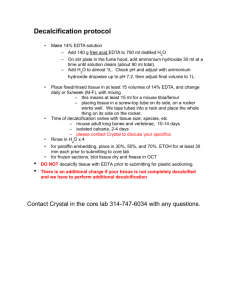
DECALCIFICATION - The removal of calcium ions from a bone or calcified tissue through a histological process makes them flexible and easier to cut - Bones: softness of paraffin embedding medium - High-speed saw and/or long periods in decalcifying solution: reducing the specimen to a size that can be easily processed, embedded and sectioned - Low speed saw: thickness of 2-3mm - It is done after fixation and before impregnation - High-quality fine-tooth saw should be used to prepare bone slices - Coarse saw can cause considerable mechanical damage and force bone fragments into the soft tissues present in the specimen Specimens that need Decalcification: Bone, teeth Teratomas containing bony tissue Calcified pathological tissue like tuberculosis foci Arteries calcified by atheroma General Considerations: - Tissue: complete fixation, small pieces - Decalcifying agent: o Change once/twice daily o Fluid to tissue volume: 20:1 o Enhanced by agitation - Ideal time: 24-48 hours or 14 days or longer (for dense bones tissue) - Optimum temperature: 18-30ºC o 55ºC: tissue will undergo complete digestion within 24-48 hours o 37ºC: impair nuclear staining with Van Gieson’s Three Main Types of Decalcifying Agents: 1. Those based on strong mineral acids 2. Those based on weaker organic acids 3. Those composed of chelating agents ACID DECALCIFYING AGENTS - Widely used for routine decalcification - Stable, readily available and relatively inexpensive - Principle: acids form calcium salts STRONG MINERAL ACIDS NITRIC ACID - Most common and the fastest decalcifying agent - This may be used as simple aqueous solutions with recommended concentrations of 5-10% - Recommended for routine purposes - Disadvantage: inhibits nuclear staining and destroys tissue in high concentrations - Imparts yellow color because it forms nitrous acid - Wash with sodium thiosulfate or urea crystals A. Aqueous Nitric Acid Solution 10% - It is recommended for urgent biopsy and for needle and small biopsy specimen - It can be used for large or heavily mineralized cortical bone specimen - Imparts a yellow color with nitrous acid - Old nitric acid solution is particularly damaging and should be replaced with fresh stock solution. B. Formol-Nitric Acid - Rapid acting - Impart a yellow color with nitric acid - Use inside a fume hood C. Perenyi’s Fluid - It is recommended for routine purposes - Maceration is avoided - Slow decalcifying agent for dense bones - Produce white precipitate D. Phloroglucin-Nitric Acid - Most rapid of all the nitric acid formulation - Yellow discoloration HYDROCHLORIC ACID - Slower action and greater distortion of tissue produced - It produces good nuclear staining - Recommended for surface decalcification of the tissue block (1% solution with 70% alcohol) A. Von Ebner’s Fluid - Does not require washing out before dehydration - Recommended for teeth and small pieces of bone. WEAKER ACIDS FORMIC ACID - Recommended for routine decalcification of postmortem research tissues - Gentler in action and less likely to interfere with nuclear staining - Formic acid in a 10% concentration is the best all-around decalcifier - Formic acid is the only weak acid used extensively as a primary decalcifying agent - Recommended for small pieces of bones and teeth - Suitable for most routine surgical specimens - Requires neutralization with 5% sodium sulfate - Decalcification Time: 2-7 days A. Formic Acid-Sodium Citrate Solution - Permits better nuclear staining - Recommended for autopsy materials, bone marrow, and cartilage and tissue studied for research purposes - Require neutralization with 5% sodium sulfate - Decalcification Time: 3-14 days TRICHOLOROACETIC ACID - Permits good nuclear staining - It does not require washing out - Weak decalcifying agent - Suitable for small spicules of bone - Decalcification Time: 4-8 days SULFUROUS ACID - It is a very weak decalcifying solution - Used for minute pieces of bones CITRIC ACID-CITRATE BUFFER SOLUTION (pH 4.5) - It permits excellent nuclear and cytoplasmic staining. - It does not produce cell or tissue distortion CHELATING AGENTS - Principle: chelating agents will combine with calcium ions and other salts to form weakly dissociated complexes and facilitate removal of calcium salts - Sequestration: removal of calcium salts - EDTA or Versene o Recommended only for detailed microscopic studies. o Binds metallic ions o Combines with calcium (insoluble nonionized complex) o Captures the calcium ions from the surface of apatite crystal, slowly reducing its size o Generally used at pH 7.0 (pH 10: works rapidly) o Optimal pH: 7-7.6 ; pH 5: works slowly (insolubility) pH >8: tissue maceration starts due to alkaline sensitive protein bonds o 1-3 weeks for small specimens; 6-8 weeks or longer to totally decalcify dense cortical bone o Change every 3 days, and in the final stage, every day, to facilitate decalcification A. Neutral EDTA - Forms minimal histological artifacts, usually caused by production of CO2 bubbles - For enzyme or immunohistochemical staining and for electron microscopy - EDTA inactivates alkaline phosphatase activity Other Techniques for Increasing the Efficiency of Decalcification: Sonication with EDTA: accelerate decalcification of trephine specimens Microwave with Hydrochloric Acid: high temperature may damage the morphology and cause staining artefacts Ion-Exchange Resin: take up the ionized calcium, thereby maintaining the effectiveness of acid Electrolytic Decalcification: in which bone is placed in acid decalcifier and attached to an electrode through which current is applied. ION-EXCHANGE RESIN - Principle: removes calcium ions from formic acid-containing decalcifying solutions, thereby increasing solubility from the tissue - Process: o Spread about ½ inch thick over the bottom of the container o Place the specimen on top of it o Add decalcifying agent o Allow to stay in solution for 1-14 days o Extents of decalcification may then be measured by physical or x-ray method o Resin Reactivation: immerse it in N/10 HCl twice and wash it with distilled water three times. Advantages: - Cellular detail is well-preserved - It permits excellent staining results. - Decalcification is hastened - It forms minimal histological artifacts Disadvantages: - It is very slow and causes slight tissue hardening ELECTROPHORESIS (ELECTRICAL IONIZATION) - Principle: positively charged calcium ions are attached to a negative electrode and subsequently removed from the decalcifying solution - Solution used for Electrolytic Decalcification: o Fornic Acid 88% o Concentrated hydrochloric acid o Distilled water MICROWAVE OVEN DECALCIFICATION - Microwave oven decalcification is faster than routine decalcification irrespective of the decalcifying agents used - Process: o Hard tissues are placed in the decalcifying agent o Then place in a microwave oven for intermittent periods with regular changes of the solution till the end point is reached Determining the end-point of decalcification A. Physical Tests - Require manipulation, bending, probing or trimming of the specimen to “feel” for remaining calcified areas - Disadvantages: o Causes mechanical damage. Small deposits of calcium can easily be missed o Probing: produce needle tract artifacts and destroy important cellular details o Pricking, slicing, bending or squeezing: disrupts soft tumor from the bone or cause false positive microfractures of fine trabeculae o Small calcified foci may not even be detected. B. Chemical Test - Can be applied when some acid decalcifiers are used - Process: o A pieces of blue litmus paper is added to a test tube containing 5mL of the discarded decalcifying agent o Add strong ammonia drop by drop until the fluid is neutralized o Cloudiness indicates calcium is still present in the solution o If the solution remains clear: add 0.5mL of saturated solution of ammonium oxalate o Stand for 30 minutes o Cloudiness will signify incomplete calcium removal o Solution remains clear after 30 minutes (decalcification is complete) C. X-ray or Radiological Method - Best method - Very expensive although the most ideal - Most sensitive and most reliable method of determining extent of decalcification - Most recommended for mercuric chloridefixed tissues due to its characteristic radioopacity which will interfere with the correct interpretation of the plate POST DECALCIFICATION TREATMENT - Removal or neutralization of acids from tissues a. Neutralization o By saturated lithium carbonate solution or 5-10% aqueous solution for several hours b. Rinsing o Tap water: most common decalcification treatment o 30 minutes for small sample o 1-4 hours for large sample o Small needle biopsies, can be blotted or quickly rinsed with water to remove acid from the surface, before transferring the specimen to a dehydrating fluid - ACID DECALCIFIED TISSUE FOR FROZEN SECTION o Thoroughly washed in water or o Stored in formol-saline containing 15% sucrose or phosphatebuffered saline (PBS) with 15-20% sucrose at 4ºC before freezing - EDTA DECALCIFIED TISSUE o Should not be placed directly into 70% alcohol o Rinsing the decalcified tissue with water or storing overnight in formolsaline or phosphate-buffered solution (PBS) will prevent the formation of crystalline precipitate. SURFACE DECALCIFICATION - Method of dealing with small unexpected deposits of calcium that may be encountered in paraffin blocks - Placed the block face down on a pad of cotton gauze saturated with 10% hydrochloric acid for approximately one hour. Allowing the decalcifier penetrate and decalcify by a small distance - Rinsed with water to remove residual acid, chilled, and sectioned. TISSUE SOFTENERS Perenyi’s Fluid: softens unduly hard tissues - Tissues are left in the fluid for 12-24 hours and dehydrated in the usual manner or - Submerged the cut surface of the block for 1-2 hours before sectioning to facilitate easier cutting of tissues. 4% aqueous phenol solution (Lendrum’s): washing out and immersion for 1-3 days Molliflex: tissue may appear swollen and soapy. This does not affect staining of tissue sections 2% hydrochloric acid 1% hydrochloric acid in 70% alcohol