Electron Microscopy 4th lecture
advertisement

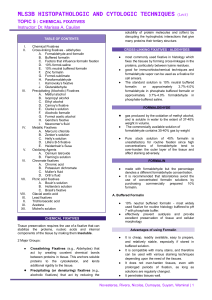
4 th lecture Five major groups of fixatives, classified according to mechanism of action: Aldehydes Mercurials Alcohols Oxidizing agents Picrates Six Factors affect fixation. Decalcification. Aldehydes include formaldehyde (formalin) and glutaraldehyde: The most widely utilized fixative in routine histopathology departments is 10% formalin (4% formaldehyde) and its derivatives. Formalin has a pungent odour, is a strong eye, skin and mucous membrane irritant and, in some workers, may cause contact dermatitis. Personnel involved with formalin usage should undergo annual respiratory sensitizer screening. Maximum recommended exposure limits are one part per million and exposure levels should be monitored on a regular basis. Formalin solutions should be carefully handled in well-ventilated rooms/fume hoods and protective clothing such as gloves, laboratory coats, goggles and respirators should be worn. The recommended time for fixation of tissues in formalin is 24–48 hours, the optimum time being 7–10 days. Modern enclosed tissue processing machines allow for the heating of reagents (40–45 oC) during processing and, thus, the process of fixation can be expedited. No fixative is ideal but 10% formalin has the advantages of preserving a wide range of tissues. Gluteraldehyde: is often the fixative of choice for tissue requiring electron microscopy, as it gives good preservation of the ultrastructure of the cell. It is a respiratory sensitizer and is strongly linked to industrial asthma. Appropriate safety measures should be observed when handling glutaraldehyde. It fixes very quickly so is good for electron microscopy. It penetrates very poorly, but gives best overall cytoplasmic and nuclear detail. The standard solution is a 2% buffered glutaraldehyde. Fix tissue by an unknown mechanism. They contain mercuric chloride and include such well-known fixatives as B-5 and Zenker's. These fixatives penetrate relatively poorly and cause some tissue hardness, but are fast and give excellent nuclear detail. Their best application is for fixation of hematopoietic and reticuloendothelial tissues. Since they contain mercury, they must be disposed of carefully. Penetrates tissue rapidly and may be used in conjunction with other fixatives to increase the speed of fixation. Absolute ethanol preserves glycogen but it causes distortion of nuclear detail and shrinkage of cytoplasm. Carnoy’s fixative is a good fixative for nucleic acids but causes shrinkage of the tissue and lysis of red blood cells. It consists of absolute ethanol, chloroform and glacial acetic acid. Methyl alcohol (methanol) and ethyl alcohol (ethanol), are protein denaturants and are not used routinely for tissues because they cause too much brittleness and hardness. However, they are very good for cytologic smears because they act quickly and give good nuclear detail. Spray cans of alcohol fixatives are marketed. They cross-link proteins, but cause extensive denaturation. Some of them have specialized applications, but are used very infrequently. Oxidizing agents including: Osmium tetroxide is used as a secondary fixative in electron microscopy, usually after primary fixation in glutaraldehyde. It fixes lipids and also preserves the fine structure of the cell. Osmium tetroxide is toxic and appropriate safety precautions should be taken when handling it. Potassium dichromate. Include fixatives with picric acid. Foremost among these is Bouin's solution. It has an unknown mechanism of action. It does almost as well as mercurials with nuclear detail but does not cause as much hardness. Picric acid is an explosion hazard in dry form. As a solution, it stains everything it touches yellow, including skin. Various additives in fixatives may be used. For example, tannic acid, phenol or heavy metal solutions may be added to formalin to increase the rate of penetration, improve preservation or enhance subsequent staining procedures. Vapour fixation. Microwave ovens can be used in fixation, either to preserve the tissue with the action of the heat itself or to speed up the process of fixation, as described earlier. Factors that will affect the fixation process: 1. Buffering 2. Penetration 3. Volume 4. Temperature 5. Concentration 6. Time interval Fixation is best carried out close to neutral pH, in the range of 6-8. Hypoxia of tissues lowers the pH, so there must be buffering capacity in the fixative to prevent excessive acidity. Common buffers include phosphate, bicarbonate HCO3- , cacodylate, and veronal. Commercial formalin is buffered with phosphate at a pH of 7. Penetration of tissues depends upon the diffusability of each individual fixative, which is a constant. Formalin and alcohol penetrate the best, and glutaraldehyde the worst. Mercurials and others are somewhere in between. One way to get around this problem is sectioning the tissues thinly (2 to 3 μm). Penetration into a thin section will occur more rapidly than for a thick section. The volume of fixative is important. There should be a 10:1 ratio of fixative to tissue. Obviously, we often get away with less than this, but may not get ideal fixation. One way to partially solve the problem is to change the fixative at intervals to avoid exhaustion of the fixative. Agitation of the specimen in the fixative will also enhance fixation. Increasing the temperature, as with all chemical reactions, will increase the speed of fixation, as long as you don't cook the tissue. Hot formalin will fix tissues faster, and this is often the first step on an automated tissue processor. Concentration of fixative should be adjusted down to the lowest level possible, because you will expend less money for the fixative. Formalin is best at 10%; glutaraldehyde is generally made up at 0.25% to 4%. Too high a concentration may adversely affect the tissues and produce artifact similar to excessive heat. Also very important is time interval from of removal of tissues to fixation. The faster you can get the tissue and fix it, the better. Artefact will be introduced by drying, so if tissue is left out, please keep it moist with saline. The longer you wait, the more cellular organelles will be lost and the more nuclear shrinkage and artefactual clumping will occur. Decalcification is the removal of calcium ions from the bone or teeth or tissue (like lung) through histological process thereby making the bone flexible and easy for pathological investigation. End-Point of Decalcification: 1. X-ray (the most accurate way) 2. Chemical testing (accurate) 3. Physical testing (less accurate and potentially damage of specimen). Other Method: Ethylenediaminetetraacetic Acid (EDTA) is a calcium absorbent that has gained popularity because of its gentleness on tissue and antigens. It is a slow decalcifies but the rate of decalcification can be increased with use of microwave energy.