Chapter 1: FRESH TISSUE EXAMINATION
advertisement
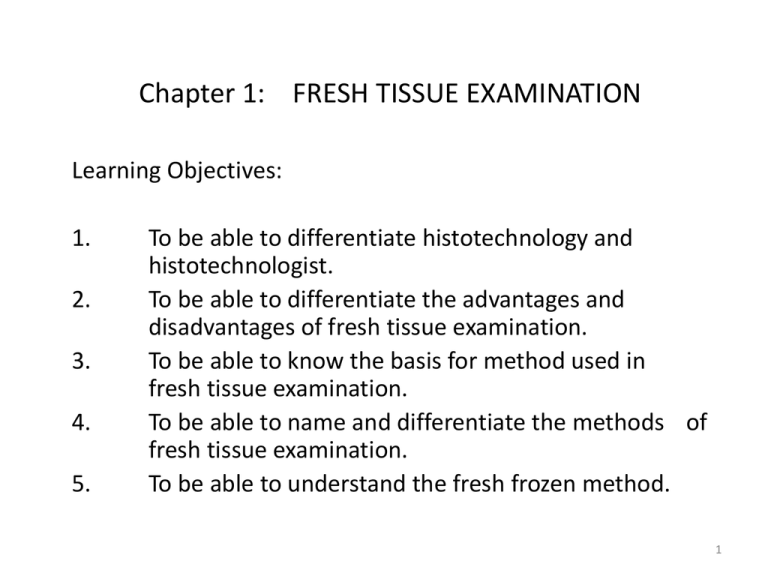
Chapter 1: FRESH TISSUE EXAMINATION Learning Objectives: 1. 2. 3. 4. 5. To be able to differentiate histotechnology and histotechnologist. To be able to differentiate the advantages and disadvantages of fresh tissue examination. To be able to know the basis for method used in fresh tissue examination. To be able to name and differentiate the methods of fresh tissue examination. To be able to understand the fresh frozen method. 1 Chapter 1: FRESH TISSUE EXAMINATION Histotechnology - is the art and science performed by the histotechnologist to produce a tissue section of good quality that will enable the pathologist to diagnose the presence of disease. The tissue may be done fresh or preserved. Advantage of fresh tissue examination: The specimen may be in living state, therefore may observe protoplasmic activities (motility, mitosis, phagocytosis, pinocytosis). Disadvantage: not permanent, and therefore liable to changes 2 Chapter 1: FRESH TISSUE EXAMINATION The choice of tissue examination method would depend on the following conditions; 1. Cell Structure and chemical components 2. Amount and nature of tissue 3. Urgency of result 3 Chapter 1: FRESH TISSUE EXAMINATION The methods of fresh tissue examination: 1. Teasing or dissociation – selected tissue is in isotonic solution, dissected and examined under the microscope. 2. Squash Preparation (Crushing) – less than 1 mm tissue pieces are compressed (stained when necessary), and examined under the microscope. 3. Smear preparation – spread cellular materials (secretions, sediments) are examined. useful for cytologic examinations a) b) c) d) 4. Streaking – using an applicator stick by direct or zigzag spread Spreading – teasing (sputum, bronchial aspirates, thick mucoid secretions) by applicator stick and spread in circular spread. Pull-Apart – thick secretions (gastric lavage, serous fluids, blood) are dispersed evenly on two slide surfaces. Touch Preparation (Impression) - freshly cut tissue surface is brought into contact to slide. Cells are examined in their actual intercellular relationship. Frozen Section – for rapid diagnosis during surgery, and demonstration of lipids and nervous tissue elements. 4 Frozen tissue – 10 -15 u in thickness cut from frozen tissue on a microtome with CO2 or on cryostat. A cryostat is cold chamber kept at an atmospheric temperature of -10 to -20 deg. C. The frozen sections are then transferred to a slide, and examined under light microscopy. Sequence of fresh frozen tissue examination by cryostat a b c d e The tissue should be fresh and processed quickly. Slow freezing can cause tissue distortion due to ice artifacts. The more commonly used methods of freezing include; 1. 2. 3. 4. Liquid nitrogen Isopentane cooled by liquid nitrogen Carbon dioxide gas Aerosol sprays 5 Chapter 2: Fixation and Fixatives Learning objectives: 1. To understand the process of autolysis 2. To determine the contributing factors in autolysis. 3. To discuss why certain tissues are affected severely by autolysis. 4. To know the objectives of fixation and qualities to serve its objective. 5. To understand the factors involve in fixation. 6. To know the types of fixative. 7. To understand the properties of formaldehyde. 6 Chapter 2: Fixation and Fixatives Once tissues are removed from the body, they undergo a process of self-destruction or autolysis. Soon after tissue death, the intracellular enzymes break down the protein and then the cell eventually undergo liquefaction. – Autolysis. 1. 2. 3. 4. Properties of Autolysis: independent of a bacterial action retarded by cold accelerated at 30 degree C temperature, inhibited at 50 degrees Celsius more severe in tissue which are rich in enzymes (e.g. liver, brain, and kidney) and less rapid in elastic and collagen tissues. 7 Chapter 2: Fixation and Fixatives Autolysed tissue presentations: 1. 2. 3. “washed-out” appearance with swelling of cytoplasm, eventually to a granular, homogenous mass which fails to take up stains. The nuclei of autolytic cells may show some of the changes including condensation (pyknosis), fragmentation (karyorrhexis) and lysis (karyolysis). There may be diffusion of intracellular importance like glycogen. The epithelium may desquamate from its basement membranes. Dead tissue may allow bacteria to proliferate. When these bacteria decompose, it can mimic those of autolyzed tissue. 8 Chapter 2: a) b) Fixation and Fixatives The objective of fixation; To preserve cells and tissue constituents in as close to life-like state. To ready for further processing without or minimal tissue change. Fixative should have the following qualifications to serve its objective; a) Arrest autolysis and bacterial decomposition b) Stabilizes cellular and tissue constituents. c) Preservation of tissue substances and proteins (for Immunohistochemisatry techniques to augment diagnosis) Fixation is therefore the first step and the foundation in a sequence of events that culminate in the final examination of ta tissue section. Each fixative has specific properties and disadvantages. Their varied effects to tissues would require careful selection of fixative when specific cellular substances is to be studied. 9 Chapter 2: Fixation and Fixatives Factors involve in Fixation: 1. Temperature – standardized fixation is carried out at room temperature. However, for electron microscopy and some histochemical procedure, fixation is usually at 0 – 4 degrees Celsius. Lower temperatures autolysis is slowed down allowing a more life-like appearance of tissues. 2. Size of specimen – the penetration of fixative is inversely directly relative to size. In which, larger tissue size will be fixed slowly. Thus, large specimens are opened and washed of contaminant or sliced thinly. . The fixative should be at least 20 times the volume of the specimen. 3. Change in volume – the volume changes in tissue with fixation, as the tissue shrinks by 33%. This is evident as the tissue show larger nuclei and cells in frozen sections (unfixed). 4. pH and Buffers – The hydrogen ion concentration varies between fixatives, but in general maintained between 6 – 8. The buffer systems maintain this physiological range of pH level (e.g.; phosphate, acetate, bicarbonate). The buffer should have the following properties; a. do not interfere with fixative b. do not inhibit enzymes 5. Osmolality – the fixative solutions; osmotic pressure may be affected by the addition of buffer. The best result is obtained by using slightly hypertonic solutions (isotonic solutions adjusted by using sucrose). 6. Concentration of fixative 7. Duration of fixation 10 Chapter 2: Fixation and Fixatives Types of fixative according to action: A. Microanatomical fixatives – are those the permit the general microscopic study of tissues structures without altering the structural pattern and normal intercellular relationship of the tissues in question. 10% formol saline 10% neutral buffered formalin Zenkers solution Bouin’s solution B. Cytological fixatives – are those that preserve specific parts and particular microscopic elements of the cell itself. 1. Nuclear fixative – are those that reserve nuclear structure (e.g. chromosome) in particular. They usually contain glacial acetic acid as their primary component due to its affinity for nuclear chromatin. Usually have pH of 4.6 or less Flemmings Carnoys Newcomers Heidenhain’s susan 2. Cytoplasmic – are those that preserve cytoplasmic structures in particular. They never contain glacial acetic acid which destroys mitochondria and Golgi bodies of the cytoplasm. Ph of more than 4.6. Kelly flemmings Regauds’s fluid Orth’s fluid C. Histochemical fixative - preserve chemical constituents of cells and tissues. Formol saline 10% Absolute ethyl alcohol Acetone Newcomer’s fluid 11 Chapter 2: Fixation and Fixatives Formaldehyde (Formalin) Properties: 1. The most widely used and routine fixative particularly for paraffin embedded sections. 2. It is a gas with a very pungent odor. 3. The commercially available solution of formaldehyde (formalin) contains 35 – 40% gas by weight. However, pure stock solution of 40% formalin is unsatisfactory. 4. Formaldehyde is commonly used as 4% solution, giving 10% formalin for fixation. Therefore, it should be diluted 1:10. 5. Formaldehyde is usually buffered to pH 7 with phosphate buffer. 6. It is thought that formaldehydes form cross-links between proteins, creating a gel, thus retaining cellular constituent. 7. It is a forgiving fixative – requires a relatively short fixation time (24 hours) but can be used for long term usage with no deleterious effects on tissue. 8. Prepared by adding 100 ml of 40% formaldehyde to 900 ml distilled water with 4 g sodium phosphatase (monobasic) and 6.5 g sodium phosphate (dibasic anhydrous). 12