Ch 23: The Respiratory System
advertisement

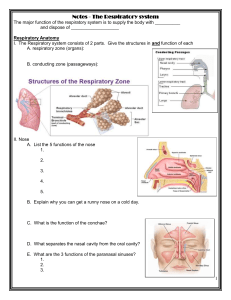
Ch 22: The Respiratory System The respiratory system • The respiratory system: – supplies the body with oxygen & disposes of carbon dioxide • Respiration – 4 steps: – 1. Pulmonary ventilation – • Movement of air into and out of the lungs • Air movement = ventilation – 2. External respiration – • Between the blood & alveoli – 3. Transport of respiratory gases – • Between the lungs and tissue cells of the body – 4. Internal respiration – • Between the systemic blood & tissue cells Functional anatomy • Organs include: – Nose, nasal cavity, pharynx, larynx, trachea, and bronchi • Respiratory zone – – Actual site of gas exchange – Composed of: respiratory bronchioles, alveolar ducts, and alveoli • Conducting zone – – All other respiratory passageways – The organs cleanse, humidify, and warm the incoming air Respiratory organs Nose & Paranasal Sinuses • Function of the nose – – – – – Provides an airway for respiration Moistens, warms, filters, & cleans incoming air Resonance chambers for speech Houses olfactory receptors • 2 divisions of the nose – – External: • External nares • Formed by hyaline cartilage • Includes bones from the skull – nasal, frontal, and maxillary bones Nose cont. – Nasal cavity: • Air enters this cavity through the external nares • Divided by the nasal septum • Contain internal nares (posterior nasal apertures a.k.a. choanae “funnels”) – continuous w/ the pharynx • Roof formed by ethmoid & sphenoid bones • Floor of cavity – palate (separates the nasal & oral cavities) – supported by maxillary processes & palatine bones = hard palate Nasal Cavity Lining of Nasal Cavity • Nasal vestibule lined with sebaceous and sweat glands and hair follicles (vibrissae = hairs, filter coarse particles) • Olfactory mucosa – receptors for the sense of smell • Respiratory mucosa – pseudostratified ciliated columnar epithelium & goblet cells • Mucous glands secrete mucus to trap dust and bacteria, serous glands secrete watery fluid with lysozyme • Epithelial cells secrete defensins (natural antibiotics that help get rid of invading microbes) • Cilia creates a gentle current that moves the mucus towards the throat – mucus builds up in the cold because the cilia move more slowly Nasal Cavity cont. • Nasal mucosa richly supplied with sensory nerve endings – Sneeze reflex • Plexuses of capillaries and thin-walled veins warm incoming air • Mucosa-covered projections (conchae) increase mucosal surface area – Groove below = meatus • Rhinitis = inflamation of nasal mucosa Paranasal Sinuses • Nasal cavity is surrounded by: – paranasal sinuses found w/in the frontal, maxillary, sphenoid, & ethmoid bones • Sinuses – – lighten the skull, – warm & moisten air, & – produce mucus The Pharynx • The pharynx connects the nasal cavity and mouth superiorly to the larynx and esophagus inferiorly. • The throat • 3 regions (superior to inferior) – Nasopharynx – Oropharynx – Laryngeopharynx • Muscular wall = skeletal muscle Phayrnx • Nasopharynx – – Posterior to the nasal cavity & inferior to sphenoid bone & superior to the soft palate – Serves only as an air passageway – Uvula closes off during swallowing to prevent food from entering nasal cavity – Continuous w/ nasal cavity through the internal nares – Pseudostratified ciliated columnar epithelium – Contains adenoids (pharyngeal tonsil) – • Trap & destroy airborne pathogens entering Nasopharynx Pharynx • Oropharynx – – Posterior to oral cavity – inferior to the soft palate to the epiglottis – Passageway for food & air – Stratified squamous epithelium – accommodates the trauma caused by food and digestive enzymes • Larygopharynx – – – – – – Air & food passageway Posterior to epiglottis Extends to the larynx Continues inferiorly w/ the esophagus Stratified squamous epithelium Oropharynx & Laryngopharynx Larynx • Voice box • Attaches superiorly to the hyoid bone, opening into the laryngopharynx, and attaches inferiorly to the trachea. • Provides/functions: – Open (patent) airway – Routes food and air into proper passageways – Produces sound through the vocal cords • Composition – – nine hyaline cartilages connected w/ membranes & ligaments Larynx • Hyaline cartilages – – Thyroid: • Shield shaped • Midline laryngeal prominence forms the Adam’s apple • Larger in males than females (male sex hormones during puberty) – Cricoid: • Ring shaped • Attaches & anchored to the trachea inferiorly – Three pairs • Arytenoid – Anchors the vocal folds (cords) • Corniculate: – Helps reinforce vocal folds • Cuneiform: – Reinforces epiglottis & vocal folds • Epiglottis Larynx – Elastic cartilage – Flexible, spoon shaped – Posterior aspect of tongue to the anterior rim of the thyroid cartilage where it anchors – Breathing – • epiglottis is free and projecting upward allowing air to flow freely into the larynx – Swallowing – • larynx pulled superiorly causing the epiglottis to tip and cover the laryngeal inlet – Coughing reflex – • when anything other than air entering the larynx Larynx • Vocal ligaments – – Attach to the thyroid cartilage – Elastic fibers – Form the core of the mucosal folds (true vocal cords) • pearly white in color because they lack blood vessels • Vibrate as air passes over them to produce sound – Glottis = • medial opening through which air passes between the vocal folds • Opening & closing along with expired air = voice production – Laryngitis = • Inflammation of the vocal folds interfering w/ their vibrations • Below vocal folds, epithelium is pseudostratified ciliated columnar type that directs power stroke of cilia upward Trachea • The trachea (windpipe) descends from the larynx through the neck into the mediastinum, where it terminates at the primary bronchi. • Very flexible • Thick lamina propria w/ pseudostratified ciliated epithelium • Smoking – – Kills cilia preventing them from propelling mucus & dust towards the pharynx – Coughing is the only way to prevent mucus from accumulating in the lungs Trachea Tracheal Wall • Mucosa – Propels debris-laden mucus toward pharynx • Submucosa – Connective tissue layer – Contains seromucous glands that help produce the mucus sheets • Adventitia – Connective tissue reinforced by C-shaped rings of hyaline cartilage – Trachealis muscle can contract to cause expired air to rush upward with greater force – Carina = last tracheal cartilage, marks point of bronchi branching • Muscosa highly sensitive – trigger coughing Bronchial tree • Conducting zone – – R & L bronchi – run obliquely in the mediastinum before plunging into the hilum (depression on the lung for blood vessel & bronchial attachment) of the lung on its respective side – Secondary bronchi branch into several orders of the tertiary bronchi, which ultimately branch into bronchioles – Bronchi segments – • Primary, secondary (lobar), tertiary (segmental), bronchioles (>1 mm), and terminal bronchioles (>0.5 mm) Conducting vs. Respiratory 1. Support structures change – As conducting airways become smaller – supportive cartilage changes in character until it is no longer present in the bronchioles 2. Epithelium type changes – Columnar -> cuboidal 3. Amount of smooth muscle increases – Complete layer of circular smooth muscle in bronchioles provides substantial resistance under certain conditions Bronchial tree • Respiratory zone – – Defined by the presence of alveoli – Begins at the terminal bronchioles which feed into the respiratory bronchioles & terminate in the alveolar ducts w/in clusters of alveolar sacs (made up of a cluster of alveoli ~300 million) Respiratory Membrane • Respiratory membrane = – Type I Cells - Single cell layer of squamous epithelium surrounded by basal lamina – Gas on one side blood flowing past on the other – Simple diffusion allows for gas exchange – alveolar wall + capillary walls + fused basal laminas – Type II Cells – secrete fluid containing surfactant that coats the alveolar surfaces and reduces surface tension • Alveoli surrounded by elastic fibers, contain open alveolar pores (air pressure equalization), & have alveolar macrophages Lungs • Occupy the thoracic cavity except the mediastinum • Each lung is suspended w/in its own pleural cavity & connected to the mediastinum by vascular & bronchial attachments = lung roots • Apex – narrow superior tip of the lung • Base – concave inferior surface of the lung that rests on the diaphragm • All conducting & respiratory passageways distal to the primary bronchi are w/in the lungs • Left lung – – Cardiac notch – impression for the heart – 2 lobes – upper & lower • Right lung – – 3 lobes- upper, middle, & lower Lungs • Each lobe contains a number of bronchopulmonary segments, each served by its own artery, vein, and tertiary bronchus • Lobule – smallest division of the lungs that can be seen w/ the naked eye – Smokers – connective tissue between lobules becomes blackened w/ carbon • Lung tissue consists largely of air spaces, with a balance of lung tissue (stroma) composed of elastic connective tissue Lung blood supply & Innervation • 2 circulations that serve the lungs (enter through the hilum) – – Pulmonary network – • Carries systemic blood to the lungs for oxygenation • Picks up O2 and unloads CO2 for blood returning to the body – Bronchial arteries – • Provide systemic blood to the lung tissue • Oxygenates the lung tissue • Lungs innervated by parasympathetic (constrict) and sympathetic (dilate) motor fibers, and visceral sensory fibers – Enter through the pulmonary plexus on the lung root Pleura • Pleura – – Thin, double-layered serosa (moist membrane found in closed cavities) • Parietal pleura – – Covers the thoracic wall, superior surface of the diaphragm, & continues around the heart between the lungs • Visceral pleura – – Covers the external surface of the lungs – Follows the lungs contours • Pleural fluid – – Allows the lungs to slide easily over the thoracic wall during breathing • Pleurisy – – Inflammation of the pleurae – Results from pneumonia – Prevents pleura from producing fluid causing friction & stabbing pain w/ each breath Mechanics of Breathing • Pulmonary ventilation is a mechanical process causing gas flow into (inspiration) and out of (expiration) the lungs according to volume changes in the thoracic cavity. • Atmospheric pressure (Patm) = 760 mm Hg – A negative respiratory pressure indicates that the pressure is lower than 1 ATM • Intrapulmonary pressure (Ppul) = pressure in the alveoli – Eventually equalizes with Patm • Intrapleural pressure (Pip) = pressure in the pleural cavity – About -4 mm Hg • Transpulmonary pressure keeps air spaces of lungs open Pulmonary Ventilation: Inspiration and Expiration • Pulmonary ventilation is a mechanical process that depends on volume changes • Volume changes lead to pressure changes, pressure changes lead to the flow of gases to equalize the pressure. – Gases always fill their container. Breathing • Quiet inspiration – – Diaphragm & intercostals muscles contract – Thoracic volume increases – Intrapulmonary pressure drops below atmospheric pressure – Air flows into the lungs – Any time intrapulmonary pressure is less than atmospheric pressure air will rush into the lungs • Forced inspiration – – Accessory muscles of the neck & thorax contract raise the ribs even more – Thoracic volume increases beyond the increase in volume during quiet inspiration Breathing • Quiet expiration – – Passive process – Relies on elastic recoil of the lungs as the thoracic muscles relax – Ribcage descends & the lungs recoil • Forced expiration – – Active process – Relies on the contraction of the abdominal muscles (oblique & transverse) – Increases intra-abdominal pressure & depresses the ribcage Inspiration •Figure 22.13.1 Expiration •Figure 22.13.2 Physical Factors Influencing Pulmonary Ventilation • Airway Resistance – Diameters of conducting tubes • Alveolar Surface Tension – Liquid molecules are more strongly attracted to each other than gas molecules – Water molecules are highly polar • Lung Compliance – Distensibility of lungs (the higher the lung compliance, the easier to expand the lungs) Respiratory volume & pulmonary ventilation • Respiratory volumes include… – Tidal, inspiratory reserve, expiratory reserve, & residual volumes • Tidal volume – – Amount of air that moves in & out of the lungs with each breath during quiet breathing – About 500 ml • Inspiratory reserve volume – – Amount of air that can be forcibly inspired beyond the tidal volume – About 2100-3200 ml • Expiratory reserve volume – – Amount of air that can be evacuated from the lungs after tidal expiration – About 1000-1200 ml • Residual volume – – Amount of air that remains in the lungs after maximal forced expiration – About 1200 ml – Helps to keep the alveoli open & prevent lung collapse R.V & P. V cont • Inspiratory capacity (IC) – – Total amount of air that can be inspired after a tidal expiration – Sum of the tidal volume & inspiratory reserve volume • Vital Capacity (VC) – – Total amount of exchangeable air • Total lung capacity – – Sum of all lung volumes – About 6000 ml in males – Less in women – smaller in size Pulmonary Function • Anatomical dead space: volume of air within the conducting zone that do not contribute to gas exchange in alveoli • Alveolar Ventilation Rate – Index of effective ventilation – Includes dead space and measures flow of fresh gases in and out – 12 breathes per min. Nonrespiratory Air Movements • Most result from reflex activity, some produced voluntarily – – – – – – Cough Sneeze Crying Laughing Hiccups *spasms of diaphragm Yawn *not believed to be triggered by levels of O2 or CO2 Gas Exchanges Between the Blood, Lungs, and Tissues • Partial Pressure = pressure exerted by each gas (proportional to percentage of that gas in the mixture. – Henry’s Law – when a mixture of gases is in contract with a liquid, each gas will dissolve in the liquid in proportion to its partial pressure. – Also depends on solubility of the gas in the liquid (temp. can affect this) • I.e. Warm vs. Cold Pop Alveolar Gas • Atmosphere is almost entirely O2 and N2; the alveoli contain more CO2 and water vapor • The relative proportions of gases in the alveoli reflect; – gas exchange occurring in the lungs, – humidification of air by conducting passages, – and mixing of alveolar gas that occurs with each breath External Respiration: Pulmonary Gas Exchange • Three factors influence the movement of O2 and CO2 across the respiratory membrane (from alveoli to blood): 1. Partial Pressure gradients and gas solubilities 2. Matching of alveolar ventilation and pulmonary blood perfusion 3. Structural characteristics of respiratory membrane Partial Pressure gradients and gas solubilities • Oxygen moves from alveoli to blood stream due to high partial pressure gradient • Carbon dioxide moves in the opposite direction with a lesser gradient, but it has a much higher solubility Matching of alveolar ventilation and pulmonary blood perfusion • Ventilation = the amount of gas reaching the alveoli • Perfusion = the blood flow in pulmonary cappilaies Structural characteristics of respiratory membrane • Healthy lungs – respiratory membrane is only 0.5 to 1 micrometer thick • Greater surface area, the more gas can diffuse across it in a given time period – Spread flat, tiny sacs have surface area 40 times greater than the skin Internal Respiration • Capillary gas exchange in body tissues driven by simple diffusion • Partial pressure and diffusion gradients are switched • Tissue cells use oxygen for metabolic activities and produce carbon dioxide Transport of Respiratory Gases by Blood • Oxygen – Bound to hemoglobin (98.5%) – Dissolved in plasma (1.5%) • Carbon dioxide – Dissolved in plasma (7-10%) – Bound to hemoglobin (~20%) – Bicarbonate ion in plasma (~70%) • Quickly enters the RBCs Transport and Exchange •Figure 22.22a Transport and Exchange •Figure 22.22b Respiratory adjustments • Adjustments during exercise – – Ventilation can increase 10-20 fold – During vigorous exercise, deeper and more vigorous respirations, called hyperpnea, ensure that tissue demands for oxygen are met • 3 neural factors – – Psychic stimulation: • Anticipation of exercise – Cortical stimulation: • Stimulation of skeletal muscles and respiratory centers – Excitatory impulses: • Signals being sent from active muscles, tendons, & joints to the respiratory area Respiratory adjustments cont. • Adjustments at high altitude: – High altitude = lower density & lower partial pressure of oxygen (pO2) • Acute mountain sickness – – Rapid transition from sea level to altitudes above 8000 ft. – Headache, dizziness, shortness of breath, nausea • Adjustments/acclimatization – – Increased ventilation rate – Lower hemoglobin saturation (less O2 available) – Increased production in erythropoietin (stimulate bone marrow to produce more RBC’s) Homeostatic imbalances • Chronic Obstructive Pulmonary Disease (COPD) – Chronic bronchitis and emphysema • Asthma – – Coughing, wheezing, chest tightness, & dyspnea (labored breathing – “air hunger”) – Caused by – active inflammation of the airways • Tuberculosis – – Fever, night sweats, weight loss, cough, & spitting up blood – Infectious disease caused by the bacterium Mycobacterium tuberculosis – Spread by coughing & inhalation • Lung Cancer – – – – – Leading cause of cancer death for both men and women in N.A. Squamous cell carcinoma (25-30%) Adenocarcinoma (40%) Small cell carcinoma (20%) Developmental Aspects • During fetal life, the lungs are filled with fluid and exchanges are made by the placenta • By 28 weeks, the respiratory system has developed sufficiently to allow a baby to breathe on its own • Cystic fibrosis – – Lethal genetic disease – most common in young children – 2 children die every day – Over secretion of mucus that clogs respiratory passageways – breeding ground for bacteria – Can impair food digestion by clogging pores that deliver bile to the intestines • Respiratory Rate – – – – – Newborn infants: 40-80 resp./min. 5 years: 25 resp./min. Adults: 12-18 resp./min. Old Age: increases again Alveoli develop and mature until young adulthood