Lecture 07 - Oxygenation
advertisement

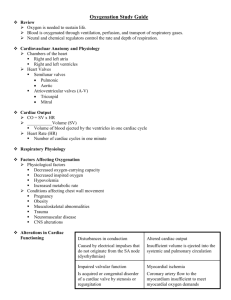
Oxygenation Chapter 39 By N.Haliyash, MD, BSN Lecture objectives Upon completing the lecture students will be able to: Define key terms related to the theme. Identify physiological processes related to oxygenation. Describe the impact of a client’s health, age, lifestyle and environment on tissue oxygenation. Identify and describe clinical outcomes of hyperventilation, hypoventilation and hypoxemia. Identify nursing care interventions that promote oxygenation. 39-2 Most cells in the body obtain their energy from chemical reactions involving oxygen and the elimination of carbon dioxide. The exchange of respiratory gases occurs between the environmental air and the blood There are 3 steps in the process of oxygenation: • Ventilation; perfusion and diffusion. 39-3 Physiology of Oxygenation Ventilation Alveolar Gas Exchange Oxygen Transport and Delivery Cellular Respiration 39-4 Physiology of Oxygenation Ventilation • Movement of air into and out of the lungs - Inhalation - Exhalation - Work of breathing Amount of muscular energy (work) required to accomplish ventilation. • Delivery of fresh air into the lung’s alveoli • Regulated by respiratory control centers • Hypoxemia is a decrease in blood oxygen concentration. 39-5 39-6 39-7 Physiology of Oxygenation Alveolar Gas Exchange • Oxygen uptake (external respiration) is the exchange of oxygen from the alveolar space into the pulmonary capillary blood. • Carbon dioxide diffuses from the blood to the alveolar space. 39-8 Physiology of Oxygenation Oxygen Transport and Delivery • Oxygen Transport in the Blood - PaO2 - SaO2 39-9 Physiology of Oxygenation Circulation/Perfusion • The heart pumps oxygenated blood into the arterial system, which carries it to the cells, and collects deoxygenated blood from the venous system. 39-10 39-11 Circulation/Perfusion Key terms: • Cardiac output Amount of blood pumped by the heart. - Norm 4 to 6 L/min • Cardiac index (CI) is the adequacy of the cardiac output for the individual - Cardiac output ÷ BSA - Norm 2.5 to 4 L/min/m³ 39-12 • Cardiac conduction system Specialized cells in the heart that generate and conduct electrical impulses; consists of the sinoatrial node, internodal pathways, atrioventricular node, bundle of His, right and left bundle branches, and Purkinje fibers. 39-13 39-14 Cardiac cycle Series of electrical and mechanical events resulting in a cycle of atrial and ventricular contractions and relaxation. • Systole Process of cardiac chamber emptying or ejecting blood. • Diastole Process of cardiac chamber filling as the right and left ventricles relax. Heart failure Inability of the heart to pump enough blood to meet the metabolic needs of the body; often accompanied by a backup of blood in the venous circuits (congestive heart failure). 39-15 Physiology of Oxygenation Cellular Respiration (internal respiration) • Oxygen diffuses from the blood to the tissues • Carbon dioxide moves from the tissues to the blood. • The blood is then reoxygenated by the heart. 39-16 Factors Affecting Oxygenation Development: Age Differences Environmental and Lifestyle Factors Disease Processes 39-17 Disease Processes Obstructive Pulmonary Disease • Asthma, emphysema, and chronic bronchitis, are collectively known as chronic obstructive pulmonary disease (COPD), or chronic airflow limitation. 39-18 Disease Processes Restrictive Pulmonary Disease • • • • Pneumonia Pulmonary fibrosis (scarring) Traumatic injury to thorax Break in pleural membrane surround lungs Atelectasis or alveolar collapse can be caused by pleural defects. 39-19 Disease Processes Diffusion Defects • Decrease in the efficiency of gas diffusion from the alveolar space into the pulmonary capillary blood 39-20 Disease Processes Ventilation-Perfusion Mismatching Atherosclerosis Heart Failure Alterations in Oxygen Uptake 39-21 Physiological Responses to Reduced Oxygenation Increased Oxygen Extraction Anaerobic Metabolism Tissue Ischemia and Cell Death Carbon Dioxide Transport and Excretion 39-22 Assessment Health History • • • • • • Events leading up to the problem Duration Methods used to alleviate symptoms Impact on activities of daily living (ADLs) Medical, psychosocial, and family history Client’s knowledge level and coping abilities 39-23 Assessment Physical Examination • Rate, rhythm, pattern of respirations • Manifestations of hypoxia - Behavior, clubbing, cyanosis, mottling • Palpation findings related to compromised ventilation include vocal fremitus, and displacement of trachea. • Percussion may reveal hyperresonance, dull percussion tone. 39-24 Assessment Physical Examination • Auscultation may reveal adventitious breath sounds. - Rales (crackles), wheezes (rhonchi), pleural friction rub, stridor • Auscultation may also reveal gallops, or extra heart sounds, and murmurs. 39-25 Diagnostic and Laboratory Data Pulse Oximetry Arterial Blood Gases (ABGs) Sputum Collection Ventilatory Function Tests Lactic Acid, Hemoglobin, Hematocrit 39-26 Diagnostic and Laboratory Data Chest X-Ray, Computerized Tomography Bronchoscopy Thoracentesis Echocardiography Electrocardiography Stress Test 39-27 Nursing Diagnosis Primary Nursing Diagnoses • • • • • Ineffective Airway Clearance Ineffective Breathing Patterns Impaired Gas Exchange Decreased Cardiac Output Altered Tissue Perfusion 39-28 Secondary Nursing Diagnoses Deficient Knowledge Activity Intolerance Disturbed Sleep Pattern Imbalanced Nutrition Acute Pain Anxiety 39-29 Outcome Identification and Planning Expected outcomes should be individualized to reflect the client’s capabilities and limitations. Identifying desired outcomes of care is best accomplished in small steps. 39-30 Outcome Identification and Planning Outcomes may be based on physiological parameters such as respiration rate or arterial blood gas values. Outcomes should be based upon the assessment findings that led to the nursing diagnoses at hand. 39-31 Implementation Interventions to Promote Airway Clearance • Teach effective coughing. • Initiate postural drainage and chest physiotherapy. • Monitor hydration. • Administer medications. 39-32 Implementation Interventions to Promote Airway Clearance • Monitor environmental and lifestyle conditions. • Manage artificial airways. • Suction the airway. 39-33 Suctioning an Endotracheal Tube 39-34 Suctioning an Endotracheal Tube 39-35 Implementation Interventions to Improve Breathing Patterns • Position client properly. • Teach controlled breathing exercises. • Manage chest drainage systems. 39-36 Implementation Interventions to Improve Oxygen Uptake and Delivery • Administer oxygen. • Administer blood components. 39-37 Implementation Interventions to Increase Cardiac Output and Tissue Perfusion • Manage fluid balance. • Encourage activity restrictions and assistance with activities of daily living. • Position client properly. • Administer medications. 39-38 Implementation Emergency Interventions • Remove airway obstruction. • Initiate cardiopulmonary resuscitation. 39-39 Implementations Interventions to Address Associated Nursing Diagnoses • Explore lifestyle and activity adaptations. • Encourage dietary and nutritional modifications. • Promote comfort measures. 39-40 Implementation Complementary Therapies • Therapies that enhance oxygenation include mediation, aroma therapy, Tai Chi, Qi Gong, and Yoga. • Herbs are often used with relaxation techniques, exercise, and diet to prevent disease. 39-41 Evaluation Based on expected outcomes that the nurse and client have established together. Success of the specific interventions may be a matter of the degree to which the client is or can be returned to a satisfactory state of respiratory functioning. 39-42 Evaluation When evaluating progress, it is important to determine if each initial expected outcome was within reasonable expectations. Revision of expected outcomes, interventions, and plan of care should be made to reflect truly reasonable expectations. 39-43