Basic Human Needs Oxygenation Ventilation/Perfusion
advertisement

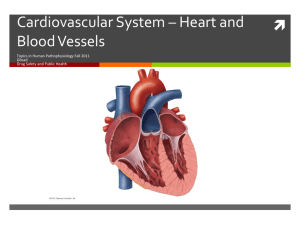
Basic Human Needs Oxygenation Ventilation/Perfusion Basic Needs: Oxygenation Oxygenation Oxygen is required to sustain life, primary basic human need The cardiac & respiratory systems function to supply the body’s oxygen demands Cardiopulmonary physiology involves delivery of deoxygenated blood to the right side of the heart & to the pulmonary system What are the 2 mechanisms that drive the function of the heart? Electrical/conduction Mechanical/pump Myocardial Pump Pumping action of heart is essential to maintenance of oxygen delivery Decreased effectiveness of pumping action is a result of disease ( MI, CHF, Cardiomyopathy) Results in diminished pumping action (stroke volume) Myocardial Pump Chambers of the heart fill during diastole & empty during systole Myocardial fibers have contractile properties that enable them to stretch during filling In healthy heart the stretch is proportionally related to the strength of contraction Frank-Starling Law of the Heart Myocardial Blood Flow Unidirectional 4 Heart valves ensure forward flow Atrioventricular (mitral & tricuspid) Open during ventricular filling (diastole), blood flows from atria into ventricles Myocardial Blood Flow Review Semilunar valves (aortic & pulmonic) Open during systolic phase Closure of atrioventricular valves & closure of semilunar valves constitute normal heart sounds “Lub” or S1=Closing of atrioventricular valves just before the contraction of the ventricles (systole) “Dub” or S2=Closing of Semilunar valves after the ventricles have emptied and heart enters the filling phase (diastole) Coronary Artery Circulation Right Coronary Artery Left Coronary Artery Circumflex Systemic Circulation LV to aorta to arteries to arterioles to capillaries Oxygen exchange occurs at the capillary level Waste product exchange occurs here also and exits via venous system back to lungs Blood Flow Regulation Cardiac Output Cardiac Index Stroke Volume Stroke Volume Preload Myocardial Contractility Afterload Conduction System Rhythmic relaxation & contraction of atria & ventricles Dependent on continuous transmission of electrical impulses Influenced by ANS (Sympathetic & parasympathetic) Conduction System Originates in the sinoatrial node (SA node) Intrinsic rate of 60-100 beats per minute Electrical impulses transmitted through atria along intra-nodal pathways to AV node Conduction System AV node mediates impulses between atria & ventricles Intrinsic rate 40-60 beats per minute AV node assists atrial emptying by delaying the impulses before transmitting it through to the Bundle of His & Perkinje fibers Conduction System Intrinsic rate of Purkinje fibers 20-40 beats per minute EKG reflects the electrical activity of conduction system Normal Sinus Rhythm Physiology of NSR Electrical Cycle NSR Respiratory Physiology Structure & Function Respiratory Gas Exchange Structure & Function Ventilation-Process of moving gases into and out of the lung Requires coordination of the muscular & elastic properties of lungs & thorax as well as intact innervation Diaphragm-Major muscle of inspiration, innervated by phrenic nerve (3rd cervical vertebrae) Structure & Function Work of Breathing Degree of compliance of lungs Airway resistance Presence of active expiration Use of accessory muscles of respiration Lung Compliance Ability of lungs to distend or expand in response to increased intra-alveolar pressure, the ease in which lungs are inflated Compliance is decreased in pulmonary fibrosis, emphysema Lung compliance is affected by surface tension of alveoli, surfactant lowers surface tension. Airway Resistance Pressure difference between the mouth & the alveoli in relation to the rate of flow of inspired gas Airway resistance increased in airway obstruction, asthma, tracheal edema Structure & Function Accessory Muscles Assist in increasing lung volume during inspiration Scalene & sternocleidomastoid (inspiration) COPD patients use these frequently Abdominal muscles Trapezius muscle and pectoralis play minor role Pulmonary Circulation Move blood to and from the alveolocapillary membrane for gas exchange Begins at pulmonary artery which receives deoxygenated blood from RV Flow continues to PA to pulmonary arterioles to pulmonary capillaries where blood comes in contact with alveolocapillary membrane Respiratory Gas Exchange Diffusion-movement of molecules from an area of higher concentration to areas of lower concentration (oxygen & CO2) Occurs at the alveolocapillary level Rate of diffusion affected by thickness of membrane Increased thickness: COPD, pulmonary edema, pulmonary infiltrates, effusions Oxygen Transport Consists of lung & cardiovascular system Delivery depends on O2 entering lungs (ventilation) And blood flow to lungs & tissues (perfusion) Rate of diffusion V/Q ratio O2- carrying capacity Oxygen Transport O2 transport capacity affected by hemoglobin Oxyhemoglobin CO2 Transport-diffuses into RBC’s & is rapidly hydrated into carbonic acid Regulation Of Respiration CNS control rate, depth, & rhythm Change in chemical content of O2, CO2 can stimulate chemorecptors which regulate neural regulators to adjust rate & depth of ventilation to maintain normal Arterial Blood Gases. Factors Affecting Cardiopulmonary Functioning Physiological Age Medications Stress Developmental Lifestyle Environmental Factors Affecting Oxygenation: Physiologic Any factor that affects cardiopulmonary functioning directly affects the body’s ability to meet O2 demands Physiologic factors include: decreased O2 carrying capacity, hypovolemia, increased metabolic rate, & decreased inspired O2 concentration Conditions Affecting Chest Wall Movement Pregnancy Obesity Trauma Musculoskeletal Abnormalities Neuromuscular Disease CNS Alterations Influences of Chronic Disease Alterations in Cardiac Functioning Disturbances in Conduction Altered Cardiac Output Impaired Valvular Function Impaired Tissue Perfusion (Myocardial) Disturbances of Conduction Dysrhythmias-deviation from NSR Junctional Classified by cardiac response origin of impulse dysrhythmias Tachycardia Bradycardia Supraventricular dysrhythmias Ventricular dysrhythmias Altered Cardiac Output Left-sided heart failure Right-sided heart Failure Impaired Valvular Function Stenosis -Stenosis of valves can cause ventricles to hypertrophy (enlarge) Obstruction of Flow Valve Degeneration Lead to Regurgitation of Blood Valves Impaired Tissue Perfusion: Myocardial Insufficient blood flow from coronary arteries to meet heart O2 demand Manifested as angina, MI Angina-transient imbalance between O2 supply & demand’ resulting in chest pain Atherosclerosis: most common cause of impaired blood flow to organs Myocardial Ischemia Myocardial Infarction-sudden decrease in coronary blood flow or an increase in myocardial oxygen demand without adequate perfusion Infarction occurs because of ischemia (reversible) or necrosis (irreversible) of heart tissue Impaired Tissue Perfusion Cardiac perfusion Cerebral perfusion (TIA, CVA) Peripheral vascular perfusion Incompetent valves Thrombus formation Blood alterations (anemia) Electrical Picture of an MI Alterations in Respiratory Function Goal of ventilation is to produce a normal arterial CO2 tension (PaCO2) between 35-45mmHg and maintain normal arterial O2 tension (PaO2) between 95-100 Alterations affect ventilation or O2 transport Hyperventilation, Hypoventilation, Hypoxia Alterations in Respiratory Function Hyperventilation- state of ventilation in excess of that required to eliminate the normal venous CO2 produced by cell metabolism Anxiety, infection, drugs or acid-base imbalance can produce hyperventilation Hyperventilation Lightheadedness Disorientation Dizziness Tachycardia Chest pain SOB Blurred vision Extremity numbness Hypoventilation Alveolar ventilation is inadequate to meet body’s O2 demand PaCO2 elevates, PaO2 drops Severe atelectasis can cause hypoventilation Hypoventilation and COPD Hypoventilation Disorientation Lethargy Dizziness Headache Decreased ability to follow instructions Convulsions Coma Dysrhythmias, cardiac death Hypoxia Inadequate tissue oxygenation at the cellular level Deficiency of O2 delivery or O2 utilization at cell level Causes: Decreased Hgb, diminished concentration of inspired O2, decreased diffusion poor tissue perfusion, impaired ventilation Hypoxia Restlessness Inability to concentrate Decreased LOC Dizziness Behavioral changes Agitation Change in vital signs Cyanosis: Peripheral vs Central Other Factors Affecting Oxygenation Age Environmental Lifestyle Medications Stress Infection Nursing Process Assessment History Physical Exam Diagnostic Tests Blood Studies Assessment: Nursing History Client’s ability to meet oxygen needs Pain Fatigue Smoking Dyspnea Orthopnea Environmental Exposure Respiratory Infections Allergies Health Risks Medications Cough Wheezing Altered breathing patterns Physical Exam Inspection Palpation Percussion Auscultation Inspection of Cardiopulmonary Status Cyanotic mucous membranes Pursed lip breathing Jugular neck vein distention Nasal faring Use of accessory muscles Peripheral or central cyanosis Edema Clubbing of fingertips Altered breathing patterns Pale conjunctivae Marked clubbing of the nails. 25Clubbing Clubbing nails Palpation Palpate for thoracic excursion PMI Palpation of peripheral pulses Palpation for skin temperature, capillary refill Palpation of lower extremities for peripheral edema Auscultation Identification of normal and abnormal breath sounds Heart sounds S1, S2 Abnormal heart sounds Murmurs Bruits Diagnostic Tests EKG Holter Monitor Stress tests Echocardiogram Cardiac cath TEE Pulmonary functions Chest x-ray Arterial blood gases Pulse ox Bronchoscopy Thoracentesis CT Scan/MRI Ventilation/Perfusion Scan Lab Studies Electrolytes Cardiac enzymes BNP Lipid Profile Coagulation Studies CBC Troponin D Dimer C reactive protein Sputum culture Throat culture AFB Cytology Interventional Cardiology PTCA Balloon Angioplasty Nursing Diagnosis Activity Intolerance Ineffective Tissue Perfusion Decreased Cardiac Output Impaired Gas Exchange Ineffective Airway Clearance Ineffective Breathing Pattern Fatigue Anxiety Planning for Care Develop goals and outcomes Set Priorities Select appropriate interventions Collaborate Involve patient and family in care Implementation: Health Promotion/Prevention Vaccinations Healthy Lifestyle Environmental pollutants Implementation: Acute Care Dyspnea Management Airway Management Mobilization of Airway Secretions Maintenance and Promotion of Lung Expansion Maintenance and Promotion of Oxygenation Breathing Exercises Hydration Dyspnea Management Treat underlying disease process and add additional therapies as needed: Pharmacological agents Oxygen therapy Physical techniques Psychosocial techniques Airway Maintenance Mobilization of Secretions Hydration Humidification Nebulization Coughing techniques Chest PT Postural drainage Suctioning Artificial airways Suctioning Oropharyngeal Nasopharyngeal Orotracheal Nasotracheal Tracheal Promotion or Maintenance of Lung Expansion Positioning of patient Incentive Spirometer Chest tubes Oxygen Therapy Goal is to prevent or relieve hypoxia Not a substitute for other treatment Treated as a drug Safety precautions Methods of O2 Delivery Nasal cannula-1-4 liters/min Oxygen Mask-Simple face mask, Venturi mask, Non-rebreather face mask, Rebreather mask Home Oxygen Therapy Medications Affecting Cardiopulmonary Functioning Cardiovascular agents: Nitrates, Calcium Channel Blockers, Beta Blockers, ACE Inhibitors/Blockers Positive Inotropic Agents (Digoxin) Antiarrhythmic Agents Antilipemic Agents Bronchodilators Cough suppressants/expectorants Benzodiazepines/Narcotics Diuretics Anticoagulants/Antiplatelet Agents Acute MI Core Measures www.the jointcommission.org Aspirin at arrival Aspirin prescribed at discharge ACE Inhibitor/ARB prescribed at discharge for left ventricular systolic dysfunction Adult smoking cessation counseling Beta Blocker prescribed at discharge Beta Blocker at arrival Thrombolysis within 30 minutes Percutaneous coronary intervention within 90 minutes Promoting Cardiovascular Circulation Positioning Medications Preventing venous stasis Cardiopulmonary Resusitation Clicker Question During the first heart sound, S1 or “Lub”, what valves are closing? A. Aortic and pulmonic B. Tricuspid and mitral C. Aortic and mitral D. Mitral and pulmonic Clicker Question Nursing care prior to cardiac catheterization includes all of the following except: A. Assess for allergy to iodine B. Evaluation of peripheral pulses C. Informed consent D. Clear liquids prior to the test Clicker Question Treatment of suspected myocardial infarction (MI) includes: A. Oxygen, aspirin, morphine, nitroglycerin B. Acetaminophen, bedrest, EEG C. Oxygen, cardiac catheterization D. Mechanical ventilation, CEA levels, acetaminophen Clicker Question Which of the following is an early sign of hypoxia? A. Pallor B. Restlessness C. Difficulty breathing D. Decreased heart rate Clicker Question 3. When evaluating a postthoracotomy client with a chest tube, the best method to properly maintain the chest tube would be to: A. Strip the chest tube every hour to maintain drainage. B. Place the device below the client’s chest. C. Double clamp the tube except during assessment. D. Remove the tubing from the drainage device to check for proper suctioning. 40 - 120 Clicker Question 2. A client with a tracheostomy has thick tenacious secretions. To maintain the airway, the most appropriate action for the nurse includes: A. Tracheal suctioning B. Oropharyngeal suctioning C. Nasotracheal suctioning D. Orotracheal suctioning 40 - 121 To have a persons Heart in Your Hands!!!!