Oxygenation - Lake-Sumter State College
advertisement

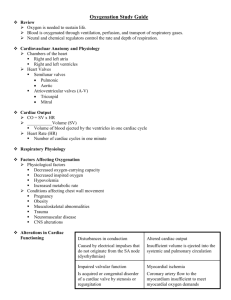
Janna Wickham RN MSN Lake Sumter Community College Nursing Foundation January 2013 Learning Objectives Safe, Effective Care Environment Describe physiological processes affecting the client's ventilation, perfusion, and exchange of respiratory gases Assess the client’s oxygenation status Health Promotion and Maintenance Develop nursing interventions that promote oxygenation Describe the impact of a client's level of health, age, lifestyle, and environment on tissue oxygenation Physiological Integrity Interpret diagnostic testing related to oxygenation, breathing, circulation, and gas exchange Systems Involved in Oxygenation Pulmonary Respiration Circulatory Perfusion Musculoskeletal Ventilation Neurological Ventilation Lungs-Lower- considered sterile Right- 3 lobes Left- 2 lobes Mediastinum- separates right from left Alveoli Alveoli-capillary membrane Gas Exchange Surfactant Pleura Pleural Space Gas Exchange Functions of Pulmonary System Ventilation Respiration Oxygenation Hypoxemia (blood) Perfusion Hypoxia Pulmonary Ventilation Inhalation Diaphragm contracts Exhalation Diaphragm Hyperventilation Hypoventilation Lung Compliance Conditions that reduce lung compliance Edema Scar tissue Loss of surfactant Lung elasticity Loss of elasticity results in lungs that inflate but air is trapped Airway resistance Small changes can cause increased airway resistance Respiration External Respiration Alveolar-Capillary Membrane Diffusion Conditions that slow or reduce gas exchange Internal Respiration How is Breathing Controlled Respiratory Center Brainstem Feedback system Chemoreceptors in the medulla, aorta, and carotid arteries Blood pH, O2 levels, and CO2 levels Lung receptors provide feedback Cardiovascular Deoxygenated blood flows into the right atrium Pulmonary circulation Alveolar-capillary membrane external gas exchange occurs Oxygenated blood flows from the lungs to the left side of the heart of out into the arterial circulation Blood Flow Song Heart Sinoatrial Node 60-100 Atrio-ventricular Node 40-60 Ventricular <40 Vascular System Arteries Arterioles Capillaries- one cell thick Veins Venules Oxygen Transport Requires adequate Cardiac output Circulation Effective regulation of cardiovascular system Hemoglobin-reservoir for oxygen 97% of blood oxygen is bound to hemoglobin 3% of oxygen is dissolved Carbon Dioxide Dissolves into plasma for diffusion into the alveoli Autonomic Nervous System Regulates Cardiovascular Function Sympathetic Parasympathetic Brain Stem Center Baroreceptors Heart Aortic arch Blood vessels Carotid artery Chemoreceptors Blood pH Oxygen Carbon dioxide levels Factors Affecting Oxygenation Developmental factors Lifestyle factors Environment Stress Medications Stop Developmental Preterm infants surfactant system is not fully developed putting them at risk for respiratory distress syndrome- atelectasis Infant airways are small and this puts them at risk for obstruction from mucous, edema, foreign objects Toddlers are at risk for URI because of tonsils and adenoids are relatively large. Preschool introduces infectious agents. Still at risk for choking. Age/Older Adults Reduces lung expansion Less alveolar inflation Less effective cough Declining immune system Diminished ability to increase ventilation Lifestyle Smoking Sedentary lifestyle Nutrition Fat Sugar Pregnancy Occupational Hazards Obesity Substance Abuse Environment Stress Catecholamine - SNS Suppressed immune system Release of cortisol Allergic Reactions Asthma –allergic reaction in the bronchioles of the lungs Air Quality Altitude Low oxygen levels can cause hypoxemia and hypoxemia Heat and Cold Nursing history fatigue dyspnea cough wheezing pain environmental exposures respiratory infections risk factors medications Examination Lung Heart Circulatory Function Ventilation and oxygenation studies Pulmonary Function Tests Arterial Blood Gas Tests pO2 Arterial blood range 80-100mmHg Venous 40 mmHg pCO2 35-45 mm Hg Pulse Oximetry Capnography Peak Flow Monitoring Lung Volume and Capacity Diagnostics Visualizing Respiratory system Chest x-ray Bronchoscopy Lung scan Basic cardiac monitoring lead placement cardiac cycle/wave form Alterations in Oxygenation Hypoxemia Hypoxia Hypercarbarbia Hypocarbia Pulmonary Causes Structural Abnormalities Airway Inflammation/Obstruction Alveolar-capillary membrane disorders Atelectasis Pulmonary Embolism Pulmonary Hypertension Cardiovascular Causes Heart Failure Cardiomyopathy Cardiac Ischemia Dysrhythmias Valve Abnormalities Anemia CO poisoning Peripheral Vascular Disease Promote Optimum Respiratory Function Immunization/ Screening Influenza, pneumonia, tuberculosis Prevent URI Position for maximum ventilation Teach/Assist with Incentive Spirometer Implement Aspiration Precautions Mobilization of pulmonary secretions Hydration Humidification Nebulization Chest physiotherapy chest percussion vibration postural drainage CPR Pharmacotherapy Artificial Airway Management Oropharyngeal Nasopharnygeal Endotracheal Tracheostomy Care Maintaining placement Suctioning Mechanical Ventilation Acute Long term Chest Tubes Purpose to remove air or fluid from the pleural space to reestablish negative pressure Flow of air or fluid is in one direction Water sealed Promotion of oxygenation Oxygen therapy safety precautions Methods of oxygen delivery nasal cannula nasal catheter transtracheal masks Home Oxygen Therapy compressed gas cylinders liquid oxygen systems concentrators Breathing exercises pursed-lip breathing diaphragmatic breathing Promote Optimum Circulation Promote Venous Return Ambulation Positioning ROM Compression devices Prevent Clot Formation CPR Pharmacotherapy Nursing Diagnosis Pulmonary Ineffective Airway Clearance Ineffective Breathing Pattern Impaired Gas Exchange Impaired Spontaneous Ventilation Dysfunctional Ventilatory Weaning Response Risk for Aspiration Nursing Diagnosis Cardiac Decreased Cardiac Output Ineffective Tissue Perfusion Risk for Shock Ineffective coping Anxiety Pain Risk for Activity Intolerance