7-Recovery-and-Social-inclusion Theo comments
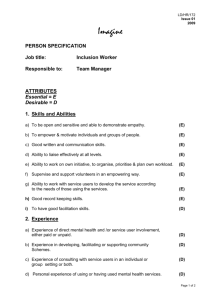
advertisement

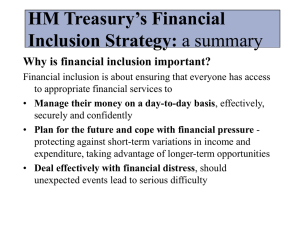
Domain Recovery and Social Inclusion General points How to read: The first part, General points, is analyzed briefly according to all interviews. Note that we have kept the different terms on the patients and the stakeholders so far. These are going to be changed in the next analyze. We have kept all suggestions (without valuing) according to eventually foundation for educational interventions in brackets (Such as: xxxxxxxx) so we get all the details with us in the further analysis. Also some citations are included, these can eventually be used in the coming paper. All input according to Children and Older people are below, still not analyzed, just copy and pasted! We think we will need the discussion in Dublin and get a picture of the framework of the analysis, before we include children/older people in the work. In the table: 6 Table X. Domains, themes and subthemes eMenthe 140502, you get an overview of the domains, themes and subthemes of the general points. Please, use track changes for all input. Theme: Knowledge Suggested title of subtheme: “Understanding the causes of mental health problems” or understanding cause of mental distress : More evidence-based knowledge of mental illnesses/distress, in depth knowledge of consequences of decreased function and how to treat in the best way and be able to inform about it. From this understand and transfer knowledge about how does recovery fit in with different models/concepts, such as biological, pharmacological, psychological, psychological distress. Models of recovery (clinical versus personal) Be aware that recovery is more than just recovery from illness but is also recovery from stigma and from the actual treatment itself. Being able to provide information connected with early recognition, such as factors promoting wellbeing, risk factors affecting to social exclusion. Also significance of the contribution of narratives to recovery theory (such as: recovery theory, i.e. Anthony, Deegan, Slade). A need to embrace the philosophy of recovery, not just knowledge (Such as: medication, knowledge of diagnoses and symptoms and how they affect the individual , the significance of activity on mental health, communication techniques, also knowledge on psychiatric disorders, prognosis and treatment models, Need to be able to learn from examples of recovery orientated practices. Need to examine what is being done already; Knowledge about relapse intervention). Knowledge of services and approaches outside mainstream mental health services (Citation: Knowledge of how medications work, I also think that patients already at an early stage are able to learn about their medications. I hear about them hiding Fass (explanation?) for their patients and that is wrong. To sit alone and read about the side effects you Googled up online is not OK.) Suggested title of subtheme: “Understanding psychosocial influences” Knowledge of how people are influenced by psychosocial factors, social participation and psychological normal factors, the importance of the social context preventive approach to social participation, such as psychological knowledge and development. Also the additional factors that affect, work, social contacts, relationships what can affect recovery, interaction between illness and the social environment; to have knowledge of various elements in the community and what they have to offer. Understanding of patient's situation from a social perspective and see the person in context. Once the crisis is over, nurse need to help people reintegrate into society. Interaction and relation of partnership of couples as well sex-counselling. One example of this was related to understanding the significance of employment to people’s recovery. It’s one thing knowing that, and another thing helping someone back into work. Provide information about environmental factors that support recovery and social inclusion, that invite patient and caregivers. Counselling skill to active adults to participate social life: 1 culture, hobbies, motion, social interaction and health promotion. Increased Knowledge of regulations within the own framework as well as outside the business. Exercising a helicopter view in organising care or support arrangements. (Such as: legislation, laws, recommendations and different activities from society, social systems to find partners to realize social inclusion). Information connected with service provision; are they working in a clientcentered manner and how this ideology is seen in practice. Also information about what kind of services are available. Knowledge and understanding on recovery and social inclusion also from families’ viewpoint; whole family is in danger of social exclusion when someone in the family has mental health problems. They might start to avoid social interaction with other people. The importance of employment. (Such as support, social issues, grants, housing, personal representative, what forums are available in social media. technical competence, society and health (mental) services, service user and carers organizations, Services of alcohol and other addictions service possibilities , such as a-clinic, folk high schools) (Citation: Prio 1 - Let organisations (as in five years only on the internet) to send a representative to introduce their network services. Perhaps therapy pages with psychologist contact?) Suggested title of subtheme: “Supporting people towards recovery” : knowledge of the various connections that exist and are available in society to organize around the person (Such as: economics, daily employment, exercise knowledge of the actions that take focus on alleviating psychological distress, eg activities, sense of coherence, knowledge about the importance of networking, knowledge about peer-support and service user’s Understand the complexity of what service users are recovering from. Understanding service users personal accounts of mental distress and recovery. Strengths based model as opposed to problem focused models, or diagnosis focused modules. Have knowledge of the recovery concept and what resources there are in society to relapse prevention. Need to understand the theory and concept of recovery and social inclusion and how service users become socially included as well as excluded. Be aware of that family or named significant others are the most important partner. (Such viewpoint.) as: Resilience and coping theory, Coproduction and narratives, Rights and responsibilities, psychological theory, psychoanalysis. Anderson’s 4 different version of recovery. Empowerment, philosophy, narratives) In-depth knowledge about managing and coordinate efforts that contribute to recovery: A variety of models / approaches can be considered to promote recovery based on person-centred care, overall and relevant health knowledge. Coordination of advanced care and social interventions. Be aware of diversity including cultural diversity. Work for anti-stigma and respect for different needs and nonjudgmental from personal references. Providing service users with the tools to understand what is happening to them. Be able to reorganize a chain of care related to recovery and social inclusion in a comprehensive recovery facilitating programme. The emphasised the importance of knowing the provenance of recovery and its relationship to the consumer-survivor movement and association with the era of civil rights movements. Skills Using past resources and strengthen self-management: See the resources of everyone and their own ability to cope with things, the importance of learning from the service users experiences and as experts. Involvement of mental health service users in the development and delivery of mental health services and in research. Move away from patient-centred services to patient directed services. The importance of first-hand accounts of people in ‘recovery’ about their experiences. (Such as: use narratives as teaching materials, user involvement in the education of nurses). An important paradigm shift professionals on master level should be aware of and know how to handle is the change from thinking in limitations to thinking in strengths and potentialities, to support the patient develop strategies to deal with life situations, and enabling choice in healthcare decisions. 2 To work person-centered and family-centred: Being responsive and find individual solutions; Stand for personcentered care and to listen to the patient , be interested, show understanding and see the possibilities, Use partnership in care, and collaborative decision making, a core message is that people are individuals and that one approach can’t work for everyone. The requirement to see the whole person and not just the physical. In this negotiating process it is important to look for the best quality options (from scientific evidence and good practices). The master level is found in how the professional combines these sometimes conflicting values. The person is first a person not person with problems. Patent narrative is the most important and care must base on patient narrative. Deepen/broaden pedagogical/educational knowledge: developing knowledge of teaching tools to work with both patients and families from a multiprofessional perspective. Bring in Narrative – we live in a world of stories and all these stories have been constructed over time. Transferring knowledge: teaching patients, relatives and colleagues individually and in groups, learn to design instructional materials, make posters and handouts. They acknowledged the contribution of experts to an online resource would be excellent to accompany the narratives of people who have experienced mental health problems (e.g. like TED talks). The students appreciate the variety of resources to aid learning. Skills and interviewing techniques : to know more about HOW I'm going to talk to the patient, more on structured conversations and communication techniques, (Such as: Motivational interviewing, Solution focused interventions, dialectical behaviour therapy, cognitive behaviour therapy). (Citation: what is a good conversation where I work, that I would need, what is the purpose of the call? One enters as a human, but perhaps lacks a proper strategy for what is it that is good for this patient, respond to pat and families so they feel seen and understood “student”) Skills that enhance Nursing Skills: engage in things that stimulate - not just medication, that nurses are good at technology and could have their own advice web sites. (Such as: online facilities, that´s why it is important, that care met up with apps where care plans, individual plans of cooperation could be recorded). Need to be able to translate the philosophy of recovery into practice – practical application. (Such as: brief solution working, how people frame distress, psychological therapy skills, basic building of CBT, Family work, positive risk taking as opposed to containing risk, opportunity to try new things i.e.reduce medication, go on leave, working on joint crisis plans, have an Signalling where there is a discrepancy between praxis and a potential better quality of care. Be able to improvise and find solutions to complex problems or coach colleagues in solution probing tracks. Being capable to think creative in an-out-of-the box way. Being able to formulate organizational formats for ‘good care’, and know how to discern between domains of medical, personal recovery and recovery in terms of participation in society and social inclusion. They must be able to switch from one domain to another and at the same time stay in line with the service user, involving also family, because recovery is a dynamic interaction with many parties. Information for public about mental health and – problems (illnesses) is crucial. Value based methods leading to high ethical quality when supporting service users in recovery, (Such as: therapeutical skills, creative therapies, touch to everyday life skills, leadership and management skills, research skills, coping and counselling skills). Service user viewpoint and how they are part of caring process (assessment, planning, evaluation etc). Slå ihop? Caring skills: be empathetic and able to listen, Providing a safe environment when people are having a crisis. Negotiating, presencing (tuning and being empathetic): Presencing is also to listen and recognize what the needs of a person are and ultimately to get somewhere (aim formulation). To address all kinds of caring needs (physical, as well as psychic and social). To develop a more coaching, supportive attitude instead of caring open dialogue). 3 (Citation: It is super most important that patients feel involved, not least during his compulsory treatment. I also want to see health care that go out and meet up with such blogs, present their business and it inspires respect and trust. Trust in daring to seek care and believe the treatment you suggested. Nurses should be a bit 'on', do not give in.) To focus/enhance/? Personal skills in nurses (not the same as Nursing Skills) : ability to be in situations and emotional states which may be difficult, ability to inspire hope and confidence and that the words and actions match, except the equal value there should be one's own inner compass available during life, at work and outside that direct action and not just by words, showing what it stands for. (Such as: have courage and curiosity, being humorous, compassion, use your own knowledge, thoughts / solutions, take initiative and not just follow directions, importance of honesty and truth in relationships, manage the negative attitudes of mental health professionals, be more self-aware of their practices and how they impact on service users, students etc.) Communication skills and a positive attitude towards people with a mental health problems and be able to demonstrate this to them. Assertive communication skills (Such as: conflict resolution, problem solving skills, engagement skills, assessment skills, power relationships, provide hope, opportunity Nurses need to be kind, they have to be warm and this needs to come through in their body language because people know when nurses are not being genuine. They can sense it when they are being treated as though they are valuable. It’s a skill to start learning how to low people – to gaze into the eyes of the person to know them. Offer a meaningful future to someone, to learn to share the nurses own life story and show that they are a person too. Be able to tune in to the specific needs that makes some values more important than others across the different patient groups. Masters level students should feel equipped to influence the culture of the organisation where they work. Therefore they need change-management skills. and control how you would work with these concepts in practice). Values Holistic approach: See the whole person and how it is affected by the approach you have. Be aware that all elements affecting patient recovery, the patient's autonomy and that one should not violate or take away the responsibility. Believe in human being´s own ability to show empathy and trust in patients, have a salutogenic approach. Knowledge of holistic and human needs and human behavior. Let patient participate in decision, The nurse must stand for continuity and have a positive view of humanity - it is possible to resolve trust in the ability of people and to be yourself. Values like understanding the human as a whole with different backgrounds (age, culture, living area) and different challenges in life, Nonjudgemental approach, dignity, respect , empathy and be approached as a human being. Patients’s actions may Conflict with our respect for autonomy, it makes you responsible for the wellbeing of the patient and obliges you sometimes to question the patient’s autonomy. It is not only this or that: it is a composition of values: (Such as: professionality, feeling responsible, equivalence, philosophical, moral (ethics) values and principles behind recovery, Humanism, Hopefulness, Respectful attitude towards clients and careers, the ability to promote autonomy ) Students need to be open about their own values. They thought that these could be encouraged and exposed through a web-based discussion forum. They emphasised the need for a skilled facilitator when dealing with sensitive issues such as values and beliefs. Ethical standpoints: Dare to stand up for a person’s rights and values; make sure that every person has an opportunity to be participated in right conditions, which involves social skills, Being guided by an inner ethical value system.Show compassion and empathy, what is considered normal today may be different tomorrow. Valuing person respect, belief in peoples potential and strengths, respect for the autonomy of the patient and the choices and decisions that they make in favour of more 4 participation Humanism, awareness of the basic values and beliefs of your own when working in mental health sector (Citat: Integrity comes in many different forms, beware of your body integrity and more, This is to avoid degrading treatment. Lay over the blanket, hide the body, give the patient choices where the injection should be added, do not pull down panties more than necessary and so on. This is obvious to some but far from all. Let the patients on compulsory treatment take their own medicine, teach patients to get into routines that hold even at home. It is not good to come home with a medicine bag and not having a clue what it is, combination between how RNs are and how RN behave. (Citation: … about stigma, it is also for us students, that one must multiply counter. That you can say no to your colleagues in the department, we've pat coming in again and again and there may be some jargon and it is important to remind each other about it, otherwise there is something wrong. Be able to stand up for the patient, sometimes against the doctors, you need to be the patients lawyer, one has to remind colleagues sometimes the patient is sick that is why they are with; thought out how the nurse see the role as staff in relation to patients, that people are of equal worth and let it permeate care) Humanistic approach: To have an advanced clinical gaze and analytical skills, no preconceptions, non judgmental. Be supportive, stand for hope, equal right to equal treatment. Human value, responsive approach and possess a personal and reflective of values, see the patient's right to care to ensure the patient's best, convey hope. The importance of hope and how mental health nurses can develop hope inspiring relationships. Respect the person and express understanding. Stimulating someone’s own responsibility and resilience, trust and hope. e committed and avoid too much professional distance. Holistic view on human beings, bio/psycho/social. Hope and its meaning during the recovery process. Empathy in dialogue process. 5 Recovery and Social Inclusion Child and Adolescence Perspective Below only descriptions from all (copy and paste) Not analysed! Knowledge Family-centred and person-centred according to the age of the child. Knowledge about normal development of children and youth health development, mental health and growth in adolescence. Knowledge when caring child and adolescent family is the most important partner. Evidence based recovery orientated interventions for working with children and adolescents. To know the child and adolescents mental health service system Knowledge about children and adolescents social exclusion process and early intervention with those who are in danger of social exclusion. Neuropsychiatric knowledge and knowledge about the importance of family in adolescence’s life. Knowledge about children’s risk of social exclusion if their parent have mental health problems, they are in danger to isolate from their friends and take an adult’s responsibilities in family. Understanding how parent’s mental health problems are affecting to child, how the problems can proceed from one generation to other. Seeing the importance of low level interventions in different problems, like in school-bullying. They highlighted the impact of cultural norms and expectations on social and personal development. There are enormous social pressures on children to conform to both peers’ values and behaviours and to state systems such as education. It was questioned about the validity of diagnosing children with mental illness and it was acknowledged that pharmaceutical companies had a vested interest in ensuring mental illness does exist amongst children. The notion therefore of recovery for young people is spurious. Furthermore, it was observed how damaging it might be to label young people with mental illness. It was observed that in the UK, some young people are unfortunate enough to find themselves on adult acute admission wards, which are scary places for such young people. He asserted that it is very important not to impose adult models on children and young people. Furthermore he thinks it is imperative to take a multi-agency approach to working with this group. He spoke about a liaison diversion service that the Centre for Mental Health funded. This project comprised of a major national programme of six pilot Youth Justice liaison and diversion schemes for young people with mental health, learning, communication difficulties or other vulnerabilities affecting their physical and emotional wellbeing. The pilot schemes were designed to ensure that children and young people with mental health and other problems get the help they need as soon as they enter the youth justice system. It is essential that students and workers have knowledge and training for child-protection issues. 6 Skills Knowledge to work in natural environments of child and adolescents like schools Skills to evaluate adolescent’s wellbeing and recognizing the neuropsychiatric disorders. Skills to use interventions to support children whose parent has mental health problems (like Family talk-intervention). Medication use in children and adolescence. Working with parents and helping them resolve issues and concerns with their children. Preventing, recognising, reporting, and managing abuse. Communication skills for working with children and adolescents. There is a need for evidence-based skills to assist professionals in a multi-dimensional, multi-party context (school, parents, care professionals, the child) to have children, diagnosed with depression, to participate in school life again. System thinking is assumed to be absolutely necessary and having a cultural sensitivity to expectations and ideas that parties involved with a problematic child express (felt as pressure sometimes by the professional) about what should be done and what should not be done. Multi-partiality is necessary to do justice to the diverse and sometimes conflicting opinions of the school or one parent from another parent (when divorced). Negotiating is another skill demanded from professionals to get parties in line and work out a workable solution for the child. Sometimes this must be combined with taking your time in order not to force one of the parties. This skill is labelled as ‘ moving with (not against) the resistance’ (just as in judo). Children and adolescent need a special approach, in which parents and other members of the family, but also class mates at school play an important role in the process of recovery. Caretakers must be aware of eyeopeners and pittfalls in this respect and know where they can find expertise for differentiated interventions for anxiety, depression etc. in children and adolescents. For instance, nowadays a lot of so called ‘blended treatment modules’ have been developed, combining face-toface contact with e-health. Recognising the early signs of mental health problems Methods of early interventions in schools and kindergartens Support for whole family not only children “Normal development of Children and youth “Computernism “ the influence of games e.g e.g Values The ethics of child psychiatry. Hope in important aspect in recovery process Stigma is damaging to all age groups but can be particularly damaging in adolescence when young people may not be sure of who they are. Therefore helping young people (and their peers) overcome stigma is important. Forgotten children, child poverty Recovery methods need to develop adolescent initiative, if young people like to study as a teacher or diplomat he is not interested in cleaning or knitting. 7 Recovery and Social Inclusion Older Persons Below only descriptions from all (copy and paste) Not analysed! Knowledge When someone in the family is having mental health problems, also grandparents and other older people are in danger to wear themselves out and they need information. It is felt to be important to have broad knowledge of the social map to be able to see how patient needs can be best matched with services of care providers. Professionals on master level must know about comorbidity from different angles and perspectives (psychosocial, medical). They must be able to switch and prioritize certain knowledge domains and approaches. The connection of psychical health and mental health problems, Knowledge about neurological diseases such as Alzheimer’s e.g. Mechanism cause social inclusion especially among older people. Older people are fist as a holistic person with some phycila or mental health problem, but they need physical caring also family or named significant others are the most important partner. There was acknowledgement of the potentially unique views of older people whose life experiences have been very different to those younger than them. For example social attitudes have changed with regards to how older people are viewed and treated. Mental illness amongst older people was questioned, for example growing old is perfectly natural, but there is a strong trend to medicalise human experience, therefore so many older people are deemed mentally ill when they begin to lose their faculties. Skills Elderly persons usually requires a bit more basic nursing, showering, brushing teeth, poor hearing, it may was harder to grab young people's basic nursing, you forget about it for you are focusing so much on psychiatry. Though sometimes you can tell, but it does not take hold of it the same way. Sometimes older people may feel as though they are too old to experience a good recovery. Mental health nurses need to know how to work therapeutically with older people and their families to instil hope about the future and to seek a meaningful recovery. Presencing is seen as an important skill to connect with the life world of the older person. Take grandparents into consideration when helping their children and grandchildren, grandparents can be a resource in recovery process. Older people need activities, comfort and companionship from the peers. Prevent ageism and abuse of elderly people. Supporting the participation of social life and prevent loneliness 8 Need therapeutic approaches: reminiscence, cognition, validation, as well as with families Understand the impact of loneliness Double stigma of being old and having mental health problems Value Respecting the autonomy of the older person is attributed as an important value in elderly care. To recognize stigma and shame behind if old person does not use mental health services 9