dyspnea 4
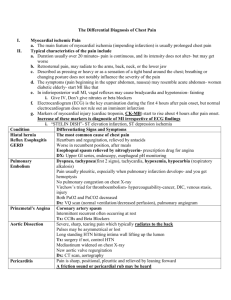
advertisement

DR.MUHAMMAD ALJOHANI ER CONSULTANT SBEM-ABEM Dyspnea: unpleasant, subjective sensation of abnormal respiration. Labored breathing - physical presentation of respiratory distress/ dyspnea Dyspnea of exertion (DOE) Orthopnea Exertion-induced SOB Recumbent-induced SOB Paroxysmal nocturnal dyspnea (PND) Sudden SOB after recumbent Eupnea - normal breathing Bradypnea - decreased breathing rate Tachypnea – breathing very fast. Pt not always aware of it. Apnea – not breathing at all Hyperpnea - faster and/or deeper breathing Hyperventilation - rapid breathing with hypocarbia Organ System Pulmonary Critical Diagnoses Airway obstruction Pulmonary embolus Noncardiogenic edema Anaphylaxis Tension pneumothorax Cardiac Pulmonary edema AMI Tamponade Associated with normal or increased respiratory effort Abdominal Emergent Diagnoses Spontaneous pneumothorax Asthma Cor pulmonale Aspiration Pneumonia pericarditis Nonemergent Diagnoses Pleural effusion Neoplasm COPD Congenital heart disease Valvular heart disease cardiomyopathy Mechanical interference Pregnancy intraabdominal sepsis Ascites Bowel obstruction Pickwikian Inflammatory/infectious process Hypotension viscerothorax Psych Hyperventilation syndrome Met/Endocrine DKA Panic attack fever Thyroid disease Infectious Trauma Epiglottitis Tension pneumothorax Cardiac tamponade Flail chest Hematologic Associated with decreased respiratory effort Neuromuscular CVA Toxicologic organophosphate poisoning CO poisoning Toxic ingestion Renal failure Electrolyte abnormality Metabolic acidosis pneumonia Simple pneumothorax hemothorax Diaphragm rupture anemia MS Guillan Barre Tick paralysis Rib fracture ALS Polymyositis porphyria TOOLS TO EVALUATE DYSPNEA Suspicion / Clinical knowledge. “If you don’t think of it, you will never find it.” History PE including Vital Signs, pulse ox, PEF Formal Studies Ability to speak Patient position Cyanosis Central vs. peripheral (acrocyanosis) Mental status Altered MS - hypoxemia/hypercapnia Pulmonary Use of accessory muscles Intercostal retractions Abdominal-thoracic discoordination Presence of stridor Cardiac Check neck for presence of JVD Inspection Use of accessory muscles Splinting Intercostal retractions Percussion Hyper-resonance vs. dullness Unilateral vs. bilateral Auscultation Air entry Stridor = upper airway obstruction Breath sounds Normal Abnormal Wheezing, rales, rhonchi, etc. Unilateral vs. bilateral ABG Vidas d-Dimer BNP Basic Metabolic Panel Cardiac Enzymes What else, and why? Asthma Pneumonia Acute Pulmonary Edema Pulmonary Embolism Emphysema Pneumo / hemothorax Carbon Monoxide (CO) Cyanide poisoning ANAPHYLAXIS 1.Age start in young age 2. Family History 3. H/O Allergic Rhinitis 4.Physical exam 5.barrel shape chest 6.X-ray chest 7. ABG Symptoms: Sudden onset; respiratory distress, Rales, ronchi. Foamy sputum. Sometimes blood tinged. Blood pressure high (vasoconstriction) usually 240/120. a) Previous H/O Heart Disease b) Hyperthyroidism c) Rheumatic Heart disease (ms) Sign of LVF a) Tachycardia b) Pulses alternan c) Basal criptation d) ECG change e) X-ray Chest ( cardiomegaly) f) Echo 1.Fever with chills 2.Pleuratic chest pain 3. purulent sputum 4. History of upper respiratory symptoms 5.signs of consolidation 6.x-ray chest 7. CBC 8. Blood culture 1.Suden chest pain 2. dyspnea,caugh 3. H/O asthma 4.COPD 5.Examination, trachea, shifted to opposite side absent breath sound 6 x-ray chest a) Previous H/O Heart Disease b) Hyperthyroidism c) Rheumatic Heart disease (ms) Sign of LVF a) Tachycardia b) Pulses alternan c) Basal criptation d) ECG change e) X-ray Chest ( cardiomegaly) f) Echo a) History of prolonged remobilization b) pelvic surgery c) contraceptive pills d) cyanosis e) ECG f) x-ray chest g) ABG h) ECHO i) PIQ study