Case 2
advertisement
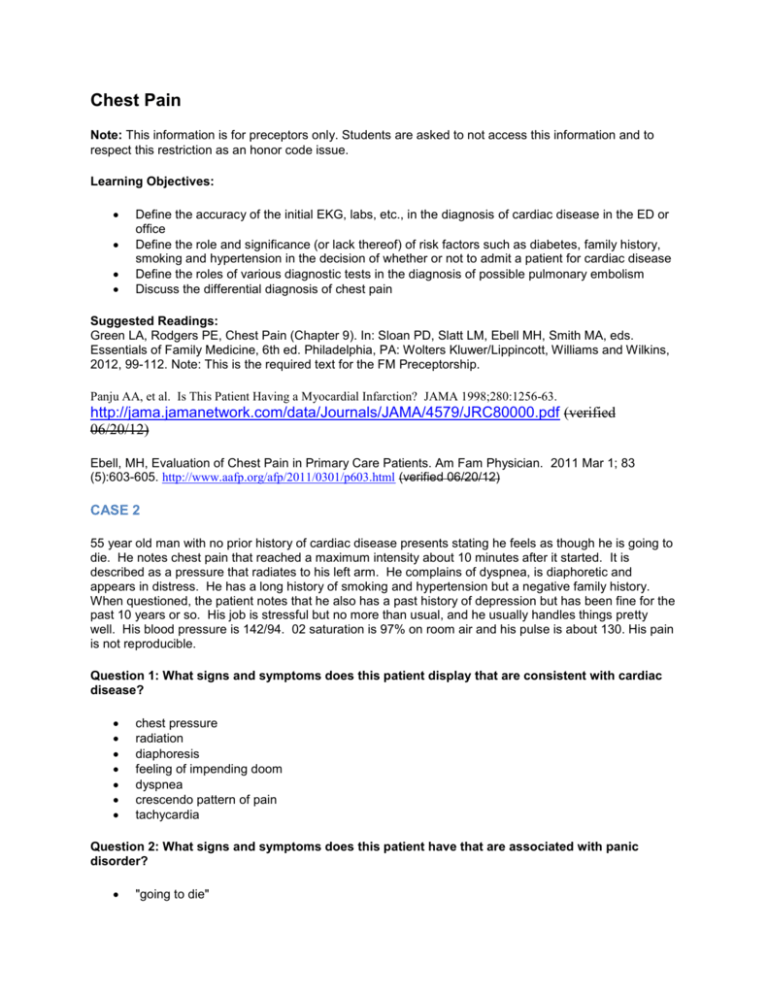
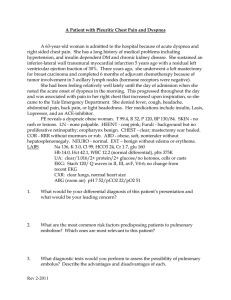
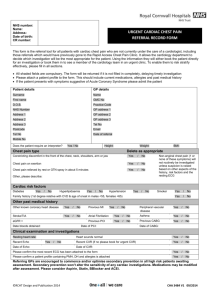
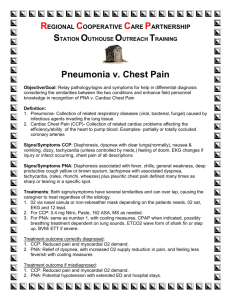
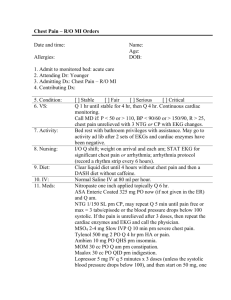
Chest Pain Note: This information is for preceptors only. Students are asked to not access this information and to respect this restriction as an honor code issue. Learning Objectives: Define the accuracy of the initial EKG, labs, etc., in the diagnosis of cardiac disease in the ED or office Define the role and significance (or lack thereof) of risk factors such as diabetes, family history, smoking and hypertension in the decision of whether or not to admit a patient for cardiac disease Define the roles of various diagnostic tests in the diagnosis of possible pulmonary embolism Discuss the differential diagnosis of chest pain Suggested Readings: Green LA, Rodgers PE, Chest Pain (Chapter 9). In: Sloan PD, Slatt LM, Ebell MH, Smith MA, eds. Essentials of Family Medicine, 6th ed. Philadelphia, PA: Wolters Kluwer/Lippincott, Williams and Wilkins, 2012, 99-112. Note: This is the required text for the FM Preceptorship. Panju AA, et al. Is This Patient Having a Myocardial Infarction? JAMA 1998;280:1256-63. http://jama.jamanetwork.com/data/Journals/JAMA/4579/JRC80000.pdf (verified 06/20/12) Ebell, MH, Evaluation of Chest Pain in Primary Care Patients. Am Fam Physician. 2011 Mar 1; 83 (5):603-605. http://www.aafp.org/afp/2011/0301/p603.html (verified 06/20/12) CASE 2 55 year old man with no prior history of cardiac disease presents stating he feels as though he is going to die. He notes chest pain that reached a maximum intensity about 10 minutes after it started. It is described as a pressure that radiates to his left arm. He complains of dyspnea, is diaphoretic and appears in distress. He has a long history of smoking and hypertension but a negative family history. When questioned, the patient notes that he also has a past history of depression but has been fine for the past 10 years or so. His job is stressful but no more than usual, and he usually handles things pretty well. His blood pressure is 142/94. 02 saturation is 97% on room air and his pulse is about 130. His pain is not reproducible. Question 1: What signs and symptoms does this patient display that are consistent with cardiac disease? chest pressure radiation diaphoresis feeling of impending doom dyspnea crescendo pattern of pain tachycardia Question 2: What signs and symptoms does this patient have that are associated with panic disorder? "going to die" dyspnea tachycardia Question 3: What would you do for this patient? Subjective discussion about whether he should be admitted to rule out MI or not. According to the referenced clinical decision rule, he would be a moderate risk patient, necessitating an EKG evaluation and either stress testing or serial troponin levels. If he does have ischemia/infarction, Aspirin has proven strong benefit in reducing mortality. IV beta blockers are contraindicated in unstable patients due to increased risk for cardiogenic shock, but they may have a net benefit for stable patients. Oral beta blockers can reduce death and reinfarction rates and should be initiated within 24 hours if there is no sign of CHF. Metoprolol is preferred over atenolol. ACE inhibitors are indicated within 24 hours and may reduce mortality in patients who have an MI. Heparin adds little benefit. Nitroglycerin reduces preload and afterload and provides good pain relief. Morphine reduces pain and anxiety. Oxygen and bed rest are often used but are not proven to be beneficial. Reperfusion therapy (thrombolytic or emergent PCI) is essential in patients with ST elevation, new LBBB, or ST depression in anterior precordial leads. Thrombolytic therapy must be initiated within 6 hours of symptom onset (perhaps 12 hours) if there are no contraindications. PCI should occur within 90 minutes of patient presentation. Treatment for chronic CAD would include continued aspirin and beta blocker therapy, smoking cessation, lipid management, long-acting CCBs, avoidance of NSAIDs. Revascularization may be indicated based on angiogram results.