Basic Human Needs Nutrition
advertisement

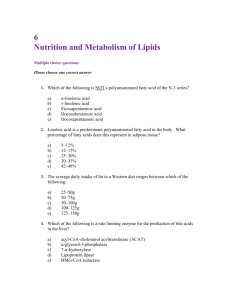
Basic Human Needs Nutrition Nutrients: The Biochemical units of nutrition Body requires fuel to provide energy for cellular metabolism and repair, organ function, growth & body movement Food is the fuel that keeps the machine that is our body running Energy requirements based on: Basal metabolic rate (BMR)-Energy needed to maintain life sustaining ( Breathing, circulation, temperature, heart rate) Resting Energy Expenditure (REE)-measurement that accounts for BMR plus energy needed to digest food & perform mild activity. Accounts for 60-70% of our daily needs Nutrients Elements necessary for body processes & function 6 Categories Carbohydrates, Proteins, Fats, Water, Vitamins, Minerals Carbohydrates Main source of energy (55-60% of calories in diet) Each gram = 4 kcal Composed of carbon, hydrogen & oxygen Main source of fuel (glucose) for brain, skeletal muscle during exercise, RBC &WBC production, cell function of renal medulla Obtained from plant foods, except for lactose (milk, sugar) Simple Carbohydrates Classified according to saccharides Monosaccharide- glucose(dextrose), fructose, galactose (building blocks of all other CHO) Glucose- blood sugar (normal fasting BS=70-100 mg/ml) Disaccharide- sucrose, lactose, maltose, Sugar alcohols-sugar replacers Artificial sweetners Complex Carbohydrates Polysaccharides are complex carbohydrates Starches, glycogen, & fiber are polysaccharides Starches are the major source of CHO in diet (grains, cereals, breads, pasta, starchy vegetables & legumes) Glycogen- animal starch (found in liver & muscle tissue, provides immediate fuel for muscle action Dietary Fiber Plant foods that cannot be broken down by body to digest Fiber eliminated by intestinal waste Adds volume, no fuel or energy Fiber in diet helps promote regularity of bowel movements, helps in regulating blood sugar, reducing cholesterol, may promote weight loss, reduce risk of colon cancer & diverticular disease Functions of CHO Provide fuel (CHO primary source) Spare body protein (body can convert protein to glucose; body will break down internal protein stores before fat stores in absence of CHO) Helps prevent ketosis (partially broken down fats accumulate in blood as ketones) Enhance learning & memory (Glucose) Proteins Provide a source of energy 4 kcal per gram Essential for synthesis of body tissue in growth, maintenance & repair Collagen, hormones, enzymes, immune cells, DNA, RNA are composed of protein Blood clotting, fluid regulation, & acidbase balance require protein Protein Composed of carbon, hydrogen, oxygen,& nitrogen There are essential and nonessential amino acids Complete and incomplete proteins Essential amino acids: isoleucine, leucine, lysine, threonine, tryptophan, methionine, histidine, valine, phenylalanine Protein Albumin & Insulin are simple proteins Lipoprotein is a complex protein (Lipid & protein) Complete & Incomplete proteins Protein Nitrogen balance- intake & output of nitrogen equal When intake of nitrogen exceeds output, body is in a positive nitrogen balance (growth, pregnancy, maintenance of lean muscle mass & vital organs, wound healing The extra nitrogen is used for building, repairing, & replacement of tissues Protein Negative Nitrogen balance- Body loses nitrogen faster than it gains it Infection, Sepsis, Fever, starvation, head injury, trauma, burns Increased nitrogen loss is the result of body tissue destruction or loss of nitrogen containing body fluids How protein functions in the body Provision of structure Growth & maintenance of tissue Regulation of body processes (hormones, enzymes, nucleoproteins) Development of immunity Circulation of blood and nutrients Backup source of energy Fats Fats(lipids) are the most calorically dense Composed of carbon, hydrogen, & oxygen (basic structural unit=glycerol) 9 kcal per gram Composed of monoglycerides, diglycerides, & triglycerides Lipogenesis- Synthesis of fatty acids Fats Fatty acids can be Saturated or Unsaturated, Monounsaturated, or polyunsaturated & Trans-fatty acids Essential Fatty Acids (Linoleic, Linolenic) must be supplied by diet Nonessential fatty acids Necessary for metabolic processes HDL vs LDL Fats Animal fats are high in saturated fatty acids Vegetable fats are high in unsaturated and polyunsaturated fatty acids Functions of Fats Fuel source Vehicle for fat soluble vitamins Satiety value Sources of essential fatty acids Organ protection Lubrication Insulation Cell membrane structure Cholesterol Not a true fat, classified as a sterol Body manufactures 1000 mg day Component of bile salts, essential component of cell membrane, necessary for production of several hormones (cortisone, estrogen adrenaline, testosterone) Elevated blood levels is a major risk factor for CAD ( < 200 mg/dL optimal) HDL vs LDL Water Critical component of body Cell function depends on a fluid environment 60-70% of body weight Muscle contains more water than fat Infants have higher total body water Fluid needs met by ingesting fluids & solid food high in water content (fruits & veggies) Vitamins Organic substances present in small amounts in food Essential for normal metabolism Body depends on dietary intake Vitamin content higher in fresh foods Classification by solubility: water or fat Vitamins Fat Soluble- Vitamins A, D, E, K Can be stored in body Provided through dietary intake except for Vitamin D Antioxidant role of vitamins Water Soluble-Vitamin C, B Complex (8 vitamins) Cannot be stored in body, provided by dietary intake Vitamins are catalysts in biochemical reactions Functions of Fat-Soluble Vitamins Vitamin A: vision, healthy epithelial tissue, proper bone growth, energy regulation Vitamin D: promotes normal bone mineralization, plays a role in calcium and phosphorus absoprtion Vitamin E: antioxidant role (protects Vitamin A & unsaturated fatty acids from oxidation Vitamin K: blood clotting, bone metabolism Functions of Water-Soluble Vitamins Vitamin C: collagen synthesis, powerful antioxidant, adrenal gland function, iron absorption, folic acid conversion B-Complex: co-enzyme in numerous metabolism mechanisms Minerals Inorganic elements essential to the body as catalysts in biochemical reactions Macrominerals-Body requires 100mg or more Trace elements-Body needs less than 100 mg Minerals Macrominerals- Calcium, Sodium, Potassium, Phosphorus, Magnesium, Sulfur, and Chloride Trace Elements- Iodine, Fluoride, Iron, Selenium, Zinc, Copper, Selenium, Manganese, Chromium A & P of Digestion Mechanical breakdown that results from chewing, churning, mixing with fluid, & chemical reaction till food reaches it’s simplest form Enzymes speed up chemical reactions A & P of Digestion Dysphagia- Difficulty swallowing Absorption occurs in small intestineprimary absorption site for nutrients Main source of water absorption via intestine, small intestine reabsorbs 9.5 L Metabolism Catabolism- Breakdown of biochemical substances into simpler substances (starvation) All body cells except RBC & neurons can oxidize fatty acids into ketones for energy in the absence of dietary CHO Metabolism Biochemical reaction with cells Anabolic or Catabolic Anabolism- Building of more complex substances, occurs when lean muscle is added through diet & exercise Amino acids are anabolized into tissue, hormones, & enzymes Dietary Guidelines Recommended dietary allowances Food Guidelines-Food Pyramid Daily values on food labels (based on 2000 kcal/day) Nutrition during Growth & Development Infant School Age Adolescents Young-Middle Adults Older Adults Alternative food patterns Cultural Aspects of Nutrition Hot Foods Hot foods: Rice, grain cereals, alcohol, beef, lamb, chili peppers, chocolate, cheese, eggs, peas, goats milk Conditions that require “hot” foods: Menstruation, cancer, pneumonia, earache, colds, headache Cultural Aspects of Nutrition Cold Foods Cold foods: Beans, citrus fruits, tropical fruits, dairy products, honey, chicken, fish and goat Conditions that require cold foods: Pregnancy, fever, infections, diarrhea, rashes, liver problems, constipation, sore throats Nursing Process & Nutrition Assessment- Anthropometry Body Mass Index Ideal Body Weight Anthropometric measurements Labs- Albumin, Transferrin, Prealbumin, Protein, Hgb, Total Lymphocyte Count Nitrogen balance Dietary & Health history Clinical Observation Nursing Diagnosis You tell me!!!!!! Conditions affecting Digestion CVA GERD Hiatal Hernia Gastric Bypass H-Pylori Ulcers Obstruction Gallbladder Malabsorption syndromes Lactose Intolerance Celiac disease IBS IBD (colitis, Crohns) Diverticulosis Diarrhea/Constipation Hemorrhoids Implementation Acute Care Oral delivery of nutrients Enteral tube feedings Nasogastric, jejunal, gastric tubes Less risk for aspiration with jejunal feedings Indicated in cancer of neck & upper GI tract, GI disorders, CVA, dementia, inadequate oral intake, respiratory failure with prolonged intubation Parenteral Nutrition: Indicated in conditions with nonfunctioning GI tract, extended bowel rest, Tube Feeding Nsg Responsibilities Document baseline weight Check Tube placement Check residual q 4 hr Check labs I&O Daily weight Aspiration Precautions Water Flush Check for complications Enteral Feeding Complications Pulmonary aspiration Diarrhea Constipation Tube occlusion Tube displacement Delayed gastric emptying (check residual) Nausea/vomiting/cramping Aspiration Precautions Elevate HOB > 30 degrees Good oral care Regular assessment of feeding tolerance Prokinetic medications (Reglan) Regular assessment of tube placement X-ray most accurate Mark tube (NGT/OGT) at exit site with indelible ink or tape. (AACN, 2005) Enteral Feeding Formulas Osmolite Perative Pulmocare Jevity Nepro Hepataid Glucerna Enteral Access Nose-nasogastric (Levine, Dobhoff, Flexiflo) Surgically placed- gastroscopy, jejunostomy Endoscopically- Percutaneous endoscopic gastroscopy (PEG) Parenteral Nutrition Specialized nutrition support in which nutrients are provided intravenously Requires nutritional assessment, placement of CV line, careful monitoring for complications Parenteral Nutrition Clients who are unable to digest or absorb enteral nutrition benefit from TPN (Total parenteral nutrition) Clients highly stressed physiologically (burns, sepsis, head injury) also benefit Parenteral Nutrition Goal is to move back to GI route Adding lipids provides supplemental kcals & provide essential fatty acids 10% - 20% Dextrose can be given peripherally (PPN) >20% Dextrose requires CV line or PICC line TPN Monitoring Daily Weight BGM every 6 hours Vitals & temp every shift I & O Labs Dedicated line for infusion Nursing Implications TPN intravenous line requires a filter Dedicated line for infusion IV tubing changed every 24 hours Requires IV pump administration Formulas prepared by pharmacist and doubled checked by RN Special physician order sheet 10% Dextrose solution used as substitute if TPN not available TPN Complications Pneumothorax from CV line insertion Infection of CV line Air embolism Lyte & mineral imbalances Concentrated glucose administration Implementation Patient Education Special diets may be necessary GI disorders-Ulcer disease, IBD, Crohns, Malabsorption Syndrome, Diverticulitis, Celiac disease Diabetes (ADA diets) CV Disease & CVA Pulmonary Disease Renal Disease Cancer HIV Usual Diet Progression NPO Clear Liquid Full Liquid Pureed Mechanical soft Soft Regular