2. Physiology of the testis 2015
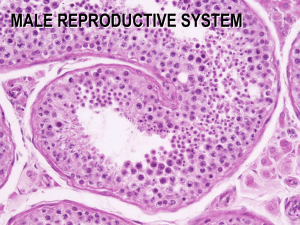
advertisement

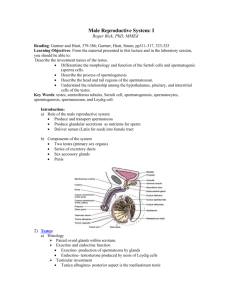
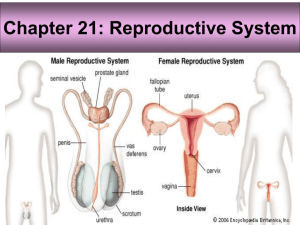
Physiology of the male reproductive system D. Gehan Shaker Badawi (2015) – (2016) Specific objectives At the end of this session, you should be able to: 1. Mention cell types of the testis 2. Mention the functions of Sertoli cells 3. List hormones involved in gametogenesis and steroidogenesis. 4. List hormones produced by the testis & describe their functions 5. Discuss biological effects of androgen (prenatal and postnatal effect). 6. Explain the mechanism of erection. Male Reproductive System Male Reproductive System 1ry sex organ Testes 2ry sex organs Tubular System Glandular System 1. Gametogenesis 2. Steriodogenesis Epididymis Seminal vesicles Secretes mucoid viscid fluid rich in Fructose, PGs, ascorbic acid & Fibrinogen A single coiled Prostate tube that essential for Secretes thin milky Motility and mucous alkaline fluid Maturation of contains the sperms plasmin, buffers, Hyaluronidase Cholesterol Bulbourethral Vas deference Essential for: Storage of sperms (in its ampulla) Transports of sperms to ejaculatory ducts. The testes: Represent 1ry sex organs in male Have 2 main functions: Spermatogenesis i.e. formation of mature sperms. Steroidogenesis i.e. synthesis and secretion of male sex hormones (testicular androgens) Histologically Spermatogenic cells Formation of mature sperm Sortoli cells 1. Supportive 2. Protective 3. Nutritive Cells Leydig Cells Androgens Secretion Cells of the Testis Spermatocytes Sortoli cell Leydig cell Cells of the testis Sertoli cell Leydig Cells Hormonal Control of testicular cells Hypothalamus -ve feedback GnRh -ve feedback Mainly inhibits FSH Specifically inhibit LH Anterior Pituitary Follicle Stimulating Hormone (FSH) Sertoli Cells Luteinizing Hormone (LH) Interstitial Cells Inhibin Androgen Binding Protein (ABP) Testosterone Spermatogenic cells Testosterone Spermatogenesis Hormonal Control of testicular cells Hypothalamus secretes gonadotropin releasing hormone (GnRH) Anterior pituitary secretes FSH and LH FSH causes Sertoli cells to secrete: Androgen Binding protein (ABP) Inhibin LH causes interstitial cells to secrete testosterone ABP binds testosterone its half-life spermatogenesis stimulate Control of testicular function: by Negative FB by 1. testosterone (on (hypothalamus & ant pituitary; against LH) 2. Inhibin (on anterior pituitary against FSH) Sortoli cells Histology Large pyramidal Non motile Non proliferating Tubular cells Site line the seminiferous tubules Function of Sertoli cells 1. Supportive 1. Provide mechanical support for the growing gametes. 2. Spermiogenesis Means: Convert spermatids to spermatozoa 3. Spermiation Means: release of sperms from Sertoli cells to lumen of seminiferous tubules 2. Provide nutrition support for growing gametes (high content of glycogen). Mechanism: by removal of excess cytoplasm. Control: under the effect of LH. Function of Sertoli cells 4. Secretory Secretion of fluid, rich in K+ , HCO3-, Essential subs for maturation of sperms. Sertoli cells synthesize and secrete the following (under the effect of FSH): 1. Inhibin Hormone ---- FSH secretion 2. Estradiol from androgenic precursors. 3. Mullerian duct-inhibiting factor preventing differentiation of the female internal sex organs in the male fetus. 4. Androgen-Binding Protein (ABP) binds testosterone its half-life 5. Blood-testis barrier: Is a memb. formed by tight junctions between the bases of Sertoli cells. It has two main functions: 1. It prevents harmful subs. in the bl. from reaching seminiferous lumen. 2. It keeps immunogenic germ cells in the seminiferous tubules from entering systemic circulation. 6. They Synthesize and secrete H-Y antigen: differentiate as testes. gonadal cells to B) Leydig Cells (interstitial cells Leydig) Site Located between seminiferous tubules (20% of testicular mass). Time of appearance Function They appear at 7-9th week of pregnancy. They secrete androgens: 1. In the fetal life under effect of human chorionic gonadotropin (HCG) secreted by the placenta. 2. At puberty under effect of pituitary gonadotropins). C) The Spermatogenic cells The spermatogonia are nonmotile stem cells that divide during the process of spermatogenesis to form mature sperms Spermatogenesis Def. Process of formation of spermatozoa from primitive germ cells. Time Starts at average of 13 year throughout whole life but ing markedly in old age (Andropause) Site Seminiferous tubules. Duration Needs 74 days (+ 12-21 days for transport of sperms into the ejaculatory ducts). Maturation of Sperms Occurs in epididymis (needs 18h to 10 days). Storage of Sperms Occurs in the vas deferens in suppressed inactive state by multiple inhibitory factors. Factors affecting 1. 2. 3. 4. Hormonal (Hypothamamic, testosterone, & others) Temperature Dietary Extrinsic 1. Hormonal Factors a) Hypothalamic-hypophysial-testicular Axis At puberty ++ hypothalamic LHRH ++ pituitary gonadotropins; FSH and LH. i) Function of FSH: 1. It maintains the gametogenic functions of the testes. 2. Stimulate Growth and secretory functions of Sertoli cells. ii) Function of LH: Stimulate Leydig cells testosterone ++ spermatogenesis. b) Testosterone: Stimulate growth & division of spermatogenic cells. Needed in high conc w is maintained by: 1. Lipid solubility of the hormone. 2. Presence of Androgen-Binding Protein (from Sertoli cells). 3. Counter current exchange: exchange of testosterone from systemic veins into spermatic arteries w runs parallel but in opposite direction to each other). Counter current exchange Note Counter current system Counter current exchanger 1. Thermoregulation (testes) 2. Testosterone (testes) 3. Thermoregulation (skin) 4. Vasa recta in kidney Multiplier system: kidney Systemic vein Spermatic artery Systemic vein c) Other Hormones: 1. Inhibin: ---FSH secretion by a direct effect on ant. pituitary. 2. Activins: are formed from precursors and ++ FSH secretion. inhibin 3. Growth h: stimulates early division of spermatogonia. 4. Thyroid h: essential for reaction of spermatogenesis. metabolic 2. Temperature The optimum temp. for spermatogenesis is 35°C (i.e.< body temp.) provided by: 1. Site of the testes: in the scrotum outside abdominal cavity. 2. Scrotal skin is thin, rich in sweat glands and with little subcutanous fat. 3. Counter current system (heat exchange between spermatic art. and veins). 4. Dartos ms buffer (contracts in cold and relaxes in hot weather). Counter current exchange Systemic vein Spermatic artery Systemic vein 3. Dietary factors 1. Starvation gonadotropin sec 2. Vit. A def. keratinization & atrophy of spermatogenic epith. 3. Vit. C deficiency testosterone synthesis 4. Extrinsic factors Mostly inhibit spermatogenesis: Irradiation, Hypoxia and toxins , Certain infections e.g. mumps destroy seminiferous tubules. We got too much…..please GOD make him finish……. Hormones secreted by the testis a) Testosterone Major hormone produced by the Leydig cells More than 98% of it is bound to plasma proteins & 2% unbound. b) Dihydrotestosterone Only 20% of dihydrotestosterone is synthesized in testis. 80% from the peripheral conversion of testosterone. Dihydrotestosterone is 2 times active than testosterone. c) Androstenedione: Important steroid precursor for blood estrogens in men. is Physiological function of testosterone During fetal life Differentiation Testicular descend After birth Sexual function Metabolic function Physiologic Effects of Testosterone A) During the Fetal Life 1- Differentiation & development of 2ry sex organs: Leydig cells of testes secrete testosterone at 79th week of gestation ++ Wolffian duct internal genitalia in male. 2- It helps descend of testes from abd. cavity into scrotum during the last 2 to 3 months of pregnancy. B) After Birth (1) Sexual functions 1- 1ry sex organ Spermatogenesis 2. 2ry sex organs Growth & enlargement. 3. Control of gonadotropin secretion (-ve FB) 4. Development of male sex characters: a) Hair: Hair especially in face, on chest, axilla and around anus. Pubic hair is triangular in appearance with apex towards umbilicus. The hair disappears from ant. part of scalp “temporal recession”. 2ry sex characters b) Voice: Deep & low pitched ( thickness of vocal cords). c) Skin: is thickened with acne formation. حب الشباب d) Body conformation Shoulders broaden and ms enlarge. e) Behavioural changes sexual desire & males become aggressive. (2) Metabolic Effects 1- Protein-anabolic effect which : Ms bulk (50% in ms mass. Bone growth with deposition of Ca2+ and finally closure of epiphysis. Thickness of the skin and vocal cords. BMR by 5-10%. 2- Increased RBCs count: 3- Effect on water and electrolytes: Moderate Na+, K+, Ca2+,& water retention. The size of the kidneys. Mechanism of Erection Mechanism of Erection The penis consists of erectile tissue made up of three columns or cords of vascular spaces spongelike Erection is accomplished by engorgement of the penis with blood (vasocongestion). In the absence of sexual excitation, the erectile tissues contain little blood, because their arterioles are constricted. the penis remains small and flaccid. During sexual arousal, these arterioles reflexly dilate and the erectile tissue fills with blood, causing the penis to enlarge. The veins that drain the erectile tissue are mechanically compressed reducing venous outflow more vasocongestion. Erection is achieved through Erection Reflex Parasymp plays the most important through its strong VD on the arterioles role The chemical mediator is nitric oxide (NO) that acts through generation of cGMP cGMP (PDE5) is inactivated by phosphodiesterase 5 Sildenafil (Viagra) inhibits PDE5 cGMP time of erection (but can’t initiate erection as it can't generate nitric oxide (NO) Mechanism of Erection Release of NO within the penile tissue Generation of c GMP Relaxation of smooth of bl vs Dilatation arterioles & arteries Expanding of sinusoids in corpora cavernosa Compression of subtunical venular plexuses Increasing of intracavernous pressure Increased resistance to outflow from penis MALE SEXUAL PERFORMANCE Erectile dysfunction or Impotence: Failure to achieve or maintain an erection suitable for sexual intercourse. Affect 50% of men between 40 and 70 years old. May be due to: 1. Psychological factors. 2. Physical factors. A. Nerve damage B. Medication that interfere with autonomic function C. Problem with blood flow to the penis. Sildenafil (Vigra): prescribed to treat erectile dysfunction. It does not produce an erection but it amplifies and prolongs an erectile response triggered by usual means of stimulation. 29 ABNORMALITIES OF TESTICULAR FUNCTION 1. Cryptorchidism: descent of testes is incomplete, testes remain in the abdomen. Occurs in neonatal life. 1. Bilateral: Impaired Testosterone secretion and spermatogenesis. 2. Unilateral :Normal Testosterone and impaired spermatogenesis. 2. Male hypogonadism: Clinical picture depends on whether testicular deficiency develops before or after puberty. causes: – Testicular disease (Hypergonadotrophic Hypogonadism) – Disorder of hypothalamus or pituitary (Hypogonadotrophic Hypogonadism) 3. Androgen secreting tumors : Leydig cell tumors (a rare condition) leads to precocious pseudopuberty in prepubertal boys. 30 REFERENCES Human physiology, Lauralee Sherwood, seventh edition. Text book physiology by Guyton &Hall,11th edition. Text book of physiology by Linda .s Costanzo, third edition. Physiology by Berne and Levy, sixth edition. 31 Thanks a lot my friend ……… Thank You