physiology10
advertisement

Name: Rakan Khtoum
Lec. Date: 22/2/2011
Lec #10
Dr.Saleem Khrysha
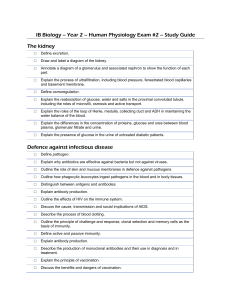
The Male Reproductive System
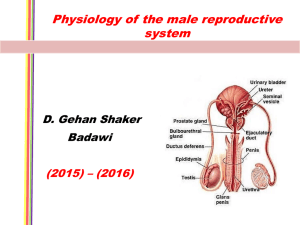
This is a figure (figure 37.1) about the regulation of reproduction in the male (the regulation is like a pyramid).
We start from the Brain (in the brain there are many centers) then Hypothalamus (hypothalamus releases many
hormones affecting not only anterior pituitary but also some other centers) releases GnRH (gonadotropin releasing
hormone) affecting cells in the anterior pituitary [gonadotroph cells] these cells they secrete 2 hormones:
FSH & LH [follicle stimulating hormone & luteinizing hormone] from the names you understand that:
FSH
function on follicles, LH
function on mature (growth) of cells.
They affect the Testis, testis secretes
Testosterone (testosterone exhibits feedback mechanism on all steps)
from the testis there are 2 other hormones or factors:
1- Activin: activates anterior pituitary to secrete more and more LH & FSH.
2- Inhibin+follistatin: inhibits anterior pituitary cells.
Brain centers affected by:
1- age: at certain age puberty occurs.
2- environment: involves many factors; hot, cold or some other factors; social factors.
3- drugs: some stimulates early puberty or delay it.
Figure 37.6 about the interactions between the leydig & sertoli cells:
There are 2 important cells in the testis:
1- Leydig cells.
2- sertoli cells.
Leydig cells: under the effect of LH they produce testosterone hormone (the potent androgen in the male). Then it is
transfer into the blood or to the sertoli cells, in the sertoli cell to function it must bind with ABP (androgen-binding
protein) and is converted into Estradiol under the effect of FSH [even the male reproductive system produces
estrogens (estrogens actually more than one hormone), estradiol is the most potent one]. Estradiol again transferred
into the blood or into leydig cells again to produce proteins or in the sertoli cells also testosterone is converted into
proteins, these proteins are important for production of sperms (spermatogenesis).
Figure 52-14:
TSH 2 subunits α & β
α: non-specific because it bound other structures of other hormones such as; LH, FSH & HCG (Human chorionic
gonadotropin).
β: specific.
Figure 12.2 about the differentiation of the genital ducts:
Chromosomes in human:
Chromosome
Somatic
type
chromosomes
sex chromosomes
sex
Male (46)
44
XY
Female (46)
44
XX
The sexual differentiation (XY): testis, sertoli cells, leydig cells, testosterone, anti-mullerian hormone, male genital
tract = male reproductive system.
If we block the testosterone
NO male reproductive system, even if it is produced very primitive.
(in embryology sometimes even female reproductive system are produced or both).
Ovaries
NO anti-mullerian hormone / NO testosterone
female reproductive system.
The different between male & female JUST:
2 glands (ovary or testis) & 2 chromosomes (X & Y), no different in the brain, thinking or anything.
Male reproductive system:
The function of reproductive system in both sexes:
1- Production of hormones (androgens or estrogens).
2- Production of cells (sperms or ovum).
We call it "dual function".
Testis are called "Primary Male Sex Organs"
they produce hormones first (not second) -because even during
fetal life the hormones are produced- then Sperms, they are produced when the boy reaches the stage of puberty.
At puberty
the testosterone responsible for the development of secondary sex organs & the appearance of
secondary sex characteristics.
-Male secondary sex organs: epididymis, vas deference, seminal vesicle, prostate gland & penis.
-Male secondary sex characteristics: laryngeal changes
deep voice, pubic, axillary & facial hair, male shape
of body.
Male secondary sex organs:
Testis (outside the body) is in the scrotum, epididymis (one of the secondary sex organs), vas deference (and it's
ampulla), seminal vesicle, prostate & bulbo-urethral glands.
-Note the location of the prostate:
Any *enlargement of the prostate gland it will affect urination (urethra).
*The enlargement
benign (mild, harmless & non-invasive) or malignant (cancer).
In both there is enlargement, in malignant: more hyperplasia than hypertrophy, in benign: more hypertrophy than
hyperplasia.
[Hyperplasia: increase in cell's proliferation (number of cells, abnormal), hypertrophy: increase in cell size]
In embryology the prostate comes from 2 sources:
1- From the center around the urethra.
2- Peripheral away from the urethra.
Usually (not always) the peripheral hypertrophy or hyperplasia is malignant and in the center is benign.
Till now they say the cause of hyperplasia
high concentration of "Dihydrotestosterone" DHT, a new theory says
that there is high accumulation of calcitonin; they found a lot of calmodulin (calmodulin
concentrates
calcium).
But the first cause is preferred: because when they remove the testis or reducing the production of DHT
the
patient cured & and it's variant. And there is another problem –maybe coincidence- even without testis they may
have prostate enlargement, and no one can gives an explanation.
Testis:
Spermatogenesis: (occurs in all seminiferous tubules of the testis)
Start with the production (initiation) of primordial cells called "spermatogonia" at puberty (they have 46
chromosomes) then they form primary spermatocytes (also they have 46 chromosomes) then they form
secondary spermatocytes by meiosis, each premature sperm contain half of the chromosomes (22+X or 22+Y) then
The sperms mature in the epididymis.
-period of spermatogenesis about 70 days.
-new cycle every 16 days (means at about the same time of primary spermatocyte of the first cycle
cycle begins).
-the maturation we call it "spermiation" (spermatid to become mature sperm).
the second
Figure 55.6:
All steps of spermatogenesis occur between the sertoli cells, they form pathway for spermatogenesis
(Spermatogonia till the sperm released into the lumen)
Table 19.2:
Sertoli cell play an important role in spermatogenesis:
-functions of sertoli cells:
1- Blood-testis barrier to chemicals.
2- To nurture the developing sperm.
3- Secrete luminal fluid, including: androgen binding protein.
4- Secrete the protein hormone "Inhibin" which inhibits FSH secretion.
5- Phagocytosis: for defective sperms.
6- Secrete during embryonic life -mullerian inhibiting factor-.
Note: {anti-mullerian = mullerian inhibiting = mullerian regression - hormone or factor}.
Male secondary sex organs:
-Sperms when they are produced (in the seminiferous tubule)
they are non-motile, they need sometimes to
mature. Maturation occurs in the epididymis
maybe this is a matter of time spending, some substances
(chemicals), hormones, enzymes affecting the sperms there so as to mature.
*This time for maturation varies from person to person (from 1 day to 10 days).
-After maturation they have to be stored –little remains in the epididymis- in the vase deference and it's ampulla,
they are stored for many months (the can be not utilized for about 6 months).
If we remove the mature sperm from the storage
this sperm can't fertilize the ovum, because the capability of a
sperm to fertilize the ovum is gained when the sperms spend sometime in the female reproductive system, this
called "Capacitation".
We say that sperms can survive for many weeks in the male reproductive system
but in the female genital tract
they live only {1 to 2} days = (after sexual intercourse between couples the sperm can remain capable of fertilizing
the ovum for about 2 days).
*Factors that affect the spermatogenesis:
1- Testosterone.
2- LH.
3- FSH.
4- Estrogens.
*Spermiation factors:
1- Estrogens.
2- Growth hormones.
3- Thyroid hormones.
In thyroid cancer
- In complete starvation
sterility occurs.
NO spermatogenesis.
Figure 6.6, the role of spermatogenesis:
If there is no testosterone
meiosis doesn't occur.
(Primary is not converted into secondary spermatocyte).
Male Accessory sex organs:
During fetal life the testis are in the abdominal cavity, in the last 3 months of pregnancy
the testis descend into
the scrotum under the effect of testosterone.
[No or deficiency in the testosterone
the testis remains in the abdominal cavity] this is called
"cryptorchidism".
(Non-descending testis = cryptorchidism)
Cryptorchidism in: 1) pre-mature babies are 30%, because testosterone still not that high, 2) in normal babies
(babies born in full term) 2% : when they born the testis is in the abdominal cavity, the doctor "physician" waits for
about 1 year, but family doesn't wait. Usually the testis descends in maximally 6 months (of course because of
testosterone).
After that by surgery they descend the testis into the scrotum to function normally Why?? Low degree (<2 °C)
below the body temperature (that means at 37 °C they don't function) they need about 34-35 °C to function.
Done By:
Rakan Khtoum Alabady