Control of Testicular Function Leydig Cells
advertisement
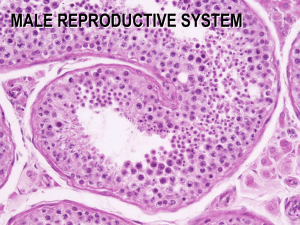
Hormonal Control of Reproduction in the Male Spermatogenesis • Spermatogenesis goes on continuously from puberty to senescence along the entire length of the seminiferous tubules • Though a continuous process, spermatogenesis can be divided into three discrete phases: – Mitotic divisions, which maintain a stem cell population of spermatogonia and provide the cells destined to become mature sperm – Meiotic divisions, which reduce the chromosome number and produce a cluster of haploid spermatids – Transformation of spermatids into mature spermatozoa, a process involving the loss of most of the cytoplasm and the development of flagella Dr. M. Alzaharna (2014) Control of Testicular Function • Physiological activity of the testis is governed by two pituitary gonadotropic hormones – follicle stimulating hormone (FSH) – and luteinizing hormone (LH) • The same gonadotropic hormones are produced in pituitary glands of men and women • FSH and LH are closely related glycoprotein hormones that consist of a common α subunit and unique β subunits that confer FSH or LH specificity Dr. M. Alzaharna (2014) Control of Testicular Function • Both gonadotropins are synthesized and secreted by a single class of pituitary cells, the gonadotropes • Their sites of stimulation of testicular function, however, are discrete: – LH acts on the Leydig cells and – FSH acts on the Sertoli cells in the germinal epithelium Dr. M. Alzaharna (2014) Control of Testicular Function Leydig Cells • The principal role of Leydig cells is synthesis and secretion of testosterone in response to stimulation by LH • In addition to stimulating steroidogenesis, LH controls: – the availability of its own receptors (downregulation) – and governs growth and differentiation of Leydig cells • In male embryos androgen secretion by the Leydig cells is initiated by human chorionic gonadotropin (hCG) Dr. M. Alzaharna (2014) Control of Testicular Function Leydig Cells • As with the adrenal cortex, the initial step in the synthesis of testosterone is the conversion of cholesterol to pregnenolone • In maintaining the functional integrity of the Leydig cells, LH maintains the levels of all steroid transforming enzymes • Testosterone released from Leydig cells may diffuse into: – nearby capillaries for transport in the general circulation – or it may diffuse into nearby seminiferous tubules where it performs its essential role in spermatogenesis Dr. M. Alzaharna (2014) Control of Testicular Function Leydig Cells • The testes also secrete small amounts of estradiol and some androstenedione, which serves as a precursor for extratesticular synthesis of estrogens • Leydig cells are the main source of testicular estrogens Control of Testicular Function Leydig Cells • Estradiol is present in seminal fluid and is essential for fluid reabsorption in the rete testis • The presence of estrogen receptors in the epididymis and several testicular cells, including Leydig cells, suggests that estradiol may have other important actions in normal sperm formation and maturation Dr. M. Alzaharna (2014) Control of Testicular Function Germinal Epithelium • The function of the germinal epithelium is to produce large numbers of sperm that are capable of fertilization • The Sertoli cells harbor and nurture sperm as they mature • Sertoli cells are the only cells known to express FSH receptors in human males and therefore are the only targets of FSH • FSH increases Sertoli cell proliferation and differentiation in the immature testis and maintains the functional state of the stable population of Sertoli cells in the mature testis • In its absence testicular size is severely reduced and sperm production, which is limited by Sertoli cell availability, is severely restricted Dr. M. Alzaharna (2014) Control of Testicular Function Germinal Epithelium • Sertoli cells lack receptors for LH but are richly endowed with androgen receptors, indicating that the actions of LH on Sertoli cell function are indirect, and are mediated by testosterone • FSH and testosterone have overlapping actions on Sertoli cells and act synergistically – Testosterone is indispensable for spermatogenesis – FSH is required for production of normal quantity and quality of sperm Dr. M. Alzaharna (2014) Testosterone: Secretion and Metabolism • Testosterone is the principal androgen secreted by the mature testis • Normal young men produce about 7 mg each day, of which less than 5% is derived from adrenal secretions • Testosterone in blood is largely bound to plasma protein, with only about 2 to 3% present as free hormone – About half is bound to albumin, – and slightly less to sex hormone-binding globulin (SHBG), which is also called testosterone-estradiolbinding globulin (TeBG) Dr. M. Alzaharna (2014) Testosterone: Mechanism of Action • Like other steroid hormones, testosterone penetrates the target cells whose growth and function it stimulates • Androgen target cells generally convert testosterone to 5 αdihydrotestosterone before it binds to the androgen receptor • The androgen receptor is a ligand-dependent transcription factor that belongs to the nuclear receptor superfamily Dr. M. Alzaharna (2014) • • • • Testosterone (T) Androgen receptor (AR) 5 α-dihydrotestosterone (DHT) The thickness of the arrows reflects the quantitative importance of each reaction Testosterone: Effects on the Male Genital Tract • Testosterone promotes growth, differentiation, and function of accessory organs of reproduction • Maintenance of normal reproductive function in the adult also depends on continued testosterone secretion • It also affects organs directly related to transport and delivery of sperm Dr. M. Alzaharna (2014) Testosterone: Effects on secondary sexual characteristics • Contributes to the morphological and psychological components of masculinity • Stimulate growth of pubic, chest, axillary, and facial hair • Adequate amounts of Dihydrotestosterone allow expression of genes for baldness • Growth and secretion of sebaceous glands in the skin are also stimulated, a phenomenon undoubtedly related to the acne of adolescence Dr. M. Alzaharna (2014) Testosterone: Effects on secondary sexual characteristics • Stimulates growth of the larynx and thickening of the vocal chords • Adolescent growth spurt results from the interplay of testosterone and growth hormone • Promote growth of muscle • Testosterone also stimulates red blood cell production • In both men and women androgens increase sexual drive ( libido ) Dr. M. Alzaharna (2014) Sexual Differentiation • The early embryo has the potential to form either testes or ovaries and develop either the male or female phenotype • Differentiation of the testes depends upon the transient expression of a single gene on the Y chromosome (SRY, sex-determining region of the Y chromosome) • It encodes a transcription factor that stimulates expression of some genes and repress expression of others Dr. M. Alzaharna (2014) SOX 9: transcription factors FGF9: autocrine factor (fibroblast growth factor 9) DHH: desert hedgehog PDGF: platelet-derived growth factor AMH: antimüllerian hormone Development of internal reproductive ducts and their derivatives • Wolffian ducts are progenitors of the upper male genital tract • The müllerian ducts are the progenitors of the upper female genital tract • Thus, regardless of its genetic sex, the embryo has the potential to develop supposedly either as male or female • The Sertoli cells begin to secrete the antimüllerian hormone (AMH), which, causes epithelial cells of the müllerian ducts to undergo apoptosis • A similar fate awaits the wolffian ducts unless they are rescued by testosterone produced by the developing Leydig cells Dr. M. Alzaharna (2014) Regulation of Testicular Function • Testicular function depends on stimulation by two pituitary hormones, FSH and LH • Without them, the testes lose spermatogenic and steroidogenic capacities • Secretion of these hormones by the pituitary gland is driven by the central nervous system through its secretion of the gonadotropin releasing hormone (GnRH) • Signals from the testis are inhibitory – Castration results in a prompt increase in secretion of both FSH and LH • FSH stimulates the Sertoli cells to synthesize and secrete a glycoprotein called inhibin, which acts as a feedback inhibitor of FSH Dr. M. Alzaharna (2014)