Lifecycle histology - U
advertisement

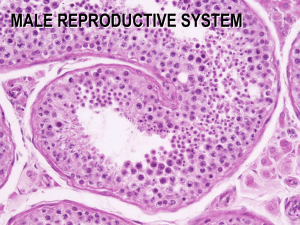
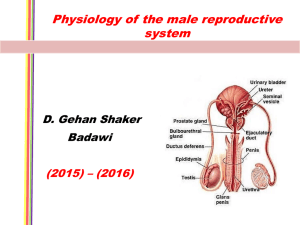
Lifecycle histology and miscellaneous topics Mike Ori Disclaimer • Faculty has not reviewed or vetted the information contained herein. • If you think this material is any way accurate, you are mistaken. • Celebrity voices are impersonated • Describe the structure of the ovary • Outer epithelial layer referred to as the germinal epithelium overlies a connective tissue capsule called the tunica albuginea. Underlying this is the parenchyma and stroma organized into a cortex and medulla. • Embryologically, where do the primordial germ cells originate? • In the yolk sac. • Whats the difference between an oogonia and an oocyte • Oogonia are the result of mitotic expansion of the primordial germ cells. When they enter meiosis, they become oocytes • How many oocytes does a female have in early fetal life, birth, puberty. How many are ovulated? • Fetal – 6 million • Neonatal – 2.5 million • Puberty – 400K • Ovulation – 450 • Distinguish a primordial follicle and a primary follicle. • Primordial follicles are more or less the resting state of the female gamete. They contain a primary oocyte arrested at prophase I surrounded by a thin layer of squamous granulosa cells. • Primary follicles are entering the active state. The granulosa cells have plumped up to cuboidal/columnar and the zona pelucida has begun to form. As the primary follicle matures, the theca forms from adjacent stromal cells. • Distinguish antral from graafian follicles • Antral follicles have a multi-layer theca, multilayer granulosa, and small fluid filled cavities called antral cavities. • Graafian follicles are larger than antral follicles and the fluid filled spaces have coalesced to form a lagoon in which the oocyte floats surrounded by a cloud of granulosa cells (cumulus oophorus). The cloud is a attached to the wall of the follicle by a stalk of granulosa cells • Name the regions of the uterine tube • (Fimbriae) – infundibulm – ampula – isthmus intramural • What are the two epithelial cells of the uterine tubes • Ciliated cells – move the ovum toward the uterus • Peg cells – produce nutritive medium and enzymes necessary for capacitation • When and at what stages is the oocyte halted during meiosis and when does each continue. • Meiosis I – Entered in fetal life – Halted at prophase I – Completes at ovulation • Meiosis II – Entered at ovulation – Halted at metaphase II – Completes on fertilization • What is the second messenger system for FSH and LH • They are both Gs linked to cAMP. • Describe the the two cell theory of hormone synthesis in the ovary. • Two cells are required to synthesize estrogen. • Theca cells overlying the follicle respond to LH to synthesize androgen (androstenedione). The androgens diffuse across the basement membrane of the follicle and enter the adjacent granulosa cells. • Granulosa cells respond to FSH to convert androgen to estrogen. • What does LH do in both males and females • It induces the production of androgens – Androstenedione in females – Testosterone in males • Why is [FSH] generally lower than [LH] • Both FSH and LH are controlled by GnRH and both are inhibited by estrogen and progesterone but FSH is also inhibited by inhibin thus there are more inhibitory inputs in the FSH pathway. • Why does LH and FSH decrease in the luteal phase and pregnancy even though estrogen levels are high in pregnancy? • Progesterone is always inhibitory to GnRH thus the high levels of progesterone in the luteal phase and during pregnancy prevent FSH and LH release and subsequently ovulation. • NOTE: its not completely clear to me if the estrogen levels are such that inhibition or induction of GnRH/LH/FSH would occur without progesterone. I think they are inhibitory levels. • When does the menstrual cycle begin • By convention with the first day of menses. • What are the phases of the menstrual cycle • Menses (1-~5) • Follicular/proliferative (1-14) • Luteal/secretory (14-1) • What is the purpose of the cervical mucous glands • They secrete mucous of varying quality depending on the hormone milieu. Normally the mucous is thick and retards entry of both sperm and micro-organisms into the upper reproductive tract. When estrogen levels peak at mid-cycle, the mucous secretions thin and allow access. • Describe the epithelium of the cervix. What is the squamocolumnar junction and why is it important • In the endocervical canal, the cervical epithelium consists of simple columnar epithelium, whereas in the vagina the cervix is covered with a nonkeratinized squamous epithelium. The squamocolumnar junction is the point where the transition is made from columnar to squamous epithelium. The area surrounding this junction is called the transformation zone. It is the site of squamous metaplasia caused by HPV infection and thus is the site of genesis for most cervical squamous cell carcinomas • Describe the glandular structure of the vagina • The vagina is non-glandular. Secretions from arousal are due to increased hydrostatic pressure from congestion of the venous plexus lining the organ. • Why do vaginal squamous epithelia synthesize glycogen? What controls glycogen synthesis and how would this impact the vaginal tract with age? • The glycogen synthesized in the vaginal mucosa is released into the lumen when the cells are sloughed. The glycogen is fermented to lactic acid by symbiotic bacterium, creating an low pH environment that is hostile to many pathogenic species. Synthesis is controlled by estrogen. • Thus as women age, the pH of the vagina should increase, leading to an increase in candida infections however, in reality (or up to date at least) this increase in candida infection does not occur…go figure • Mammary glands are glorified versions of what? • Apocrine sweat glands…put that way, what’s all the fuss about? • If sperm were vegetarian, what kind would they be? • Frutitarians as they consume fructose for fuel • Describe the structure of a seminiferous tubule • The seminiferous tubule is divided into a basal and adlumenal compartment. Spermatogonia lie within the basal comparment and give rise to the spermatocytes of the adlumenal compartment. Sertoli cells rest against the basement membrane of the tubule and extend through to the adlumenal compartment. Leydig cells lie outside the tubule in the testicular stroma. • What is the function of leydig and sertoli cells • Leydig cells respond to LH to produce testosterone. • Sertoli cells secrete androgen binding protein which effectively traps testosterone within the seminiferous tubule thus ensuring that high the levels of testosterone required to support spermatogenesis are maintained. • Describe the regulation of GnRH, FSH, and LH in males • Testosterone feeds back to inhibit GnRH, FSH, LH. Inhibin secreted by sertoli cells feeds back on FSH only. • Differentiate spermatocytogenesis from spermiogenesis • Spermatocytogenesis refers to the production of spermatocytes. • Spermiogenesis refers to the maturation of spermatids into spermatazoa. • Which cell is responsible for the blood testes barrier • That would be the sertoli cell. • Is it me or does sertoli sound like a plumber? • What are the functions of the sertoli cell • Support – Physical support for spermatogenic series • Protection – Blood testes barrier • Nutrition – Regulate nutrients available to spermatocytes • Phagocytosis – Spermatocyte and spermatid castoffs • Secretion – ABP – Inhibin • What’s the difference between testis, testes, and testicle? • Testis = testicle = singular • Testes = plural • So what does that mean for estes? • What is the normal sperm count and at what level is a man considered sterile? • Normal 100 million/ml • Sterile < 20 million/ml • What are the components of semen and where are they synthesized. • Testes – Sperm • Seminal vesicles (50%) – Fructose – Prostaglandins – Proteins • Fibrinogen • Prostate (50%) – Proteins • Fibrinolysin – Citric acid – Acid phosphatase • Fructose levels in ejaculate are assays for the function of what? • The seminal vesicles. • What are the three regions of the male urethra • Prostatic • Membranous (very short) • Penile/spongy • What is the difference between emission and ejaculation • Emission is the movement of sperm into the urethra by sympathetic contraction of the smooth muscle of the ducts and glands • Ejaculation refers to the expulsion of sperm from the penis by contraction of the bulbospongiosis muscle. • Which vessel is responsible for erection in males and females? • Deep artery of the penis/clitoris • At what point are sperm able to fertilize an ova? • Only after capacitance in the uterine tubes. • Why is the blood testis barrier important? Is there an analogy in females? • The blood testes barrier prevents the activation of an immune response against the antigenically different sperm • To me it seems like the inherent isolation of the oocyte by the granulosa cells serves the same purpose • How is dihydrotestosterone formed? • DHT is formed from testosterone by 5-alpha reductase • What are the target tissues for DHT and testosterone • DHT – Scrotum – Penis – Prostate • Testosterone – – – – – – Muscle Bone Skin Adipose Brian liver • Men have estrogen at levels equivalent to certain times in the menstrual cycle of females. Why are men not feminized? • Men have a much higher quantity of testosterone than women such that the T:E ratio is about 1000:1 in men and 70:1 to 6:1 in females. It is believed that the ratio is an important factor in response to the sex steroids. • What is SRY • SRY is the sex determining region gene on the y chromosome. It induces development of leydig and sertoli cells • Explain the role of hormones in the development of the male and female reproductive tracts • Male – SRY on Y induces sertoli and leydig cells. – Single DAX1 on X promotes testes development – Leydig derived testosterone induces survival of the mesonephric ducts – Sertoli derived anti-mullerian hormone causes the regression of the paramesonephric ducts – DHT causes the differentiation of the prostate and male external genitalia • Female – Two DAX1 genes on X promotes ovary formation – Lack of testosterone allows degeneration of mesonephric duct – Lack of AMH allows maturation of paramesonephric duct • What percent of pregnancies are unplanned and what is their disposition. • 50% unplanned • 25% aborted (1/2 of unplanned) • What are the roles of mifiprex and cytotek in abortion? • They are used for medical abortions. • Mifiprex is a progesterone antagonists that causes degeneration of the endometrium • Cytotek is a PGE2 agonist that causes contraction of the myometrium. • Define cytogenetics • The study of chromosomes, their structure, and their inheritance • Define euploidy and aneuploidy • Euploidy is the state of having an exact multiple of the haploid number of chromosomes. 1n, 2n, 3n, etc • Aneuploidy is the state of having a nonintegral number of chomosomes. 2n+1 of 47, XXY • Describe the structural rearrangements of chromosome • In gross terms rearrangements may be balanced or unbalanced. In the latter there is loss or gain of genetic material • Deletion – loss of genetic material • Duplications – gain of genetic material • Inversions – swapping material within the same chromosome • Translocations – movement of material to other chromosomes • Robersonian translocations – Joining of two acrocentric chromosomes to form a single chromosome • List the descriptive locations of the centromere • Metacentric – near the middle • Sub metacentric – off-center • Acrocentric – on one side – 13,14,15,21,22 – Robertsonian translocations possible • If a person has a robertsonian translocation of 13 and 21 what is their pheonotype. What is the pheonotype of their offspring? • The carrier will be normal as they still have the full complement of 13 and 21. Their offspring may have downs if the robertsonian chromosome is assorted into the gamete along with the normal chromosome 21. • In broad terms describe the differences between sex chromosome abnormalities and autosomal chromosome abnormalities • Sex chromosome – abnormalities of stature and sexual maturation – Turner = short – Klinefelters = tall • Autosomal – Mental retardation – Birth defects • During pregnancy the total number of erythrocytes increases and yet the mother may be technically anemic. Why? • Erythrocytes increase 33% but volume increases 45-50%. Thus more RBC are distributed in an even larger volume. • What are the phases of fetal development with regard to teratogens? • Preimplantation – 0-14 days – All or nothing • Organogenesis – 15-60 days – All organ systems • Growth and differentiation – 61-term – Brain • What are the principles of teratology • Timing – Exposure timing must be consistent with defect • Genetic susceptibility – Maternal and fetal • Tissue access – Must have access to the fetus • Pattern of malformation – Must be consistent • Dosage effects • What categories of disorders are screened for in the newborn screening in Arizona • Amino acid disorders – PKU – CNS damage, limit phenylalanine – MSUD – CNS damage, limit branch chain ketoacids • Fatty acid disorders – MCAD – liver heart damage, avoid fasting • Organic acid disorders • Hemoglobinopathies – Sickle cell – Thalasemia • Others – – – – – Biotinidase deficiency – biotin cycling, exogenous biotin supplements Galactosemia – liver toxicity, limit lactose Congental adrenal hyperplasia – 21-OHase salt wasting Hypothyroidism - cretinism Cystic fibrosis – pancreatic enzymes, treatment programs • What principles are used in determining the tests on the newborn screen • Must be common disease • Must be treatable • Cost effective, sensitive, specific test must be available • Describe the phases of labor • Phase I effacement and dilation – 4cm dilation until full effacement and dilation • Phase II – delivery of infant – Cardinal movements of labor • Phase III – placenta delivery • What are the cardinal movements of labor • • • • • • • • Engagement Descent Flexion Internal rotation Extension External rotation Expulsion Don’t forget I enjoy extremely expensive equipment • Outline the role of CRH in parturition • Increases exponentially through term. • Manufactured in placenta and effects mother and fetus • Fetal – CRH /\ cortisol lung maturation phospholipid surfactants in lungs release to amniotic fluid proinflammatory effacement of cervix, /\ prostaglandins, /\ contractility • Outline the changes in the myometrium through term • Myometrial cells are hypotrophic in the resting uterus. Estrogen causes hyperplasia and hypertrophy of the cells. • Ion channel changes increase excitability as term nears • Increased synchronicity during labor (3rd tri?) allows coordinated waves of contraction proceeding from the fundus • Oxytocin receptor concentration /\ during term reaching zenith in labor • List important teratogens • TORCH organisms – Rubella – hearing loss, eye abnormalities – CMV – Blueberry muffin, cerebral calcifications • Maternal – Diabetes – spine, lower extremities, heart, kidneys – PKU – CNS development issues – Hyperthermia – CNS development issues • Medications – – – – • Anticonvulsants – various – hydantoin, valproic acid Lithium – tricuspid valve defect (ebsteins ) Vitamin A – Ear defects, CNS, Thymus Warfarin – Nasal hypoplasia, epiphyseal stippling Recreational drugs – Alcohol – FAS – Cocaine – Vascular disruption, miscarriage, fetal cerebral infarcts • Compare omission and commission • Omission = withholding care • Commission = withdrawing care • From WikiAnswers – Act of Commission is the doing of an act that causes harm. Example: I dug a hole in the road and you fell into it. I am liable because I dug the hole which caused you injury. – Act of Omission is the failure to do something which failure causes harm. Example: I saw a hole in the road, I knew it was there, I failed to cover it up or failed to warn you about it and you fell in. I did not do what a prudent person would have done to keep someone from harm. • Why does commission have two M’s? They have different Latin roots. • C + omission <> comission • C + omission = commission • Distinguish multifactorial disorders from single gene disorders • Single gene disorders occur when a disease is attributable to a defect in a single gene. Diseases caused by the confluence of many different genes are referred to as multifactorial disorders. • Single gene disorders often appear earlier in life than multifactorial. Appearance order rule of thumb is – Cytogenetic at birth – Single gene in childhood – Multifactorial adulthood • Define qualitative, discrete, and quantitative traits • Qualitative = discrete = trait absent or present in binary fashion. E.G. cleft lip • Quantitative traits are distributed along a spectrum. Disease occurs at an defined point along the spectrum. Height and intelligence are quantitative traits. • Predict the impact of genetics on a disease using the relative risk ratio. • • • • • • Recall that RR = (familial)/(population). RR=1 = no genetic link RR > 1 = increasing genetic link RR autism = 150 RR diabetes = 12 Therefore autism has a stronger genetic link than diabetes • Describe the risk threshold model for multifactorial behaviors • Within a population it is assumed that there is a continuous distribution of genetic liability for many traits. At the highest end, people exceed the risk threshold and are therefore affected. • As a person moves farther along the spectrum, disease severity increases and genetic liability increases. • In this model, increasing severity equates to increased likelihood of trait in offspring due to increased genetic liability in the adult. • In the risk threshold model, what factors affect a persons risk of disease • Increasing relatedness to someone with the disease. – Parents > grand parents >> 2nd cousin • Increases with the number of affected relatives • Increases with increasing severity of the disease • When sex linked, offspring of probands of the less commonly affected sex are higher. I.e. If your mom is color blind, and you’re male, you’re color blind. If you’re female and dad is color blind, you will be aat least a carrier and will exceed the risk threshold only if mom is color blind (100% likely) or a carrier (50% likely). • Distinguish learning disability from intellectual disability. Also, define the standard deviation for intelligence tests • Intellectual disability occurs when the following criteria are met – full scale IQ is < 2SD from the mean – Deficits in adaptive behavior – Occurs before 18 • Learning disabilities occur when there is a 1SD deviation between scores regardless of FSIQ. • 1 SD is 15 IQ points • Define the levels of intellectual disability and detail their expected reading and working levels Level IQ range Reading (grade ) Work/living Mild 2-3 SD (55-69) 3-6 Independent Moderate 3-4 SD (40-54) 1-3 Supported Severe 4-5 SD (25-39) Survival Group home Profound < 25 None Assisted for all care Note that each step falls off 1 SD. • What common medical school past-time can lead to mental retardation in offspring • Alcohol consumption leading to FAS • Based on his beard, what movie roles could Dr Weil be typecast for? • • • • Moses Santa Claus Whaling captain Villian (comic book type)