The power of Self-Management – Lisa Gestro, GM Primary Care CMH
advertisement

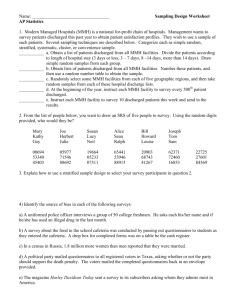
The Power of Self Management ‘Helping People Help Themselves’ Lisa Gestro GM Primary and Integrated Care 1 Why Self Management? • Unsustainable growth in demand • A system that is now over specialised • A generational shift away from families and communities caring for each other • The disease burden of lifestyles will shortly overwhelm the system 2 Unsustainable Growth in Demand • CMDHB has both the highest population growth rate and the highest ageing rate in the country. • Counties is forecast to run out of hospital beds in mid 2013 based on current growth patterns. • Middlemore hospital is already too often full • Our ED sees nearly 100,000 people per year • We are not the only DHB grappling with these issues 3 Supply and Demand Imbalance Projections of bed demand against planned beds for medical and surgical services in Middlemore Hospital 650 Existing & planned beds Existing & planned beds (subjected to approval) Number of med/surg/AOU/MSSU beds 600 Projected demographic and nondemographic growth (high growth) 550 500 450 400 350 2010 2011 2012 2013 2014 Year 2015 2016 2017 Over Specialisation • 118 unique nursing delegations that work across 175 departments • 5 cars in the driveway • Each tasked with only a very narrow scope of practice and accountability 6 Intergenerational Change ‘we used to have Self Management in the 50’s, it was called family’ Professor Harry Rea, Clinical Director Integrated Care, CMDHB • People have become disempowered as medicine as become more complex • Busy lives have overtaken our ability to care for eachother 7 So what’s happening at Counties to tip this balance? What is System Integration? Its just a step to the left… AN OPERATING SYSTEM What are the core ingredients? • Understanding and responding to community needs and engagement with community resources • Flexible use of system resources to respond to this within the district wide framework that has been agreed • Clinicians able to respond flexibly to best meet the local needs and work together in a sustainable way to achieve this • A learning system that allows local innovation but also supports shared learning about our successes and failures 12 Coordinated Care for At-Risk Individuals Very Very High High Risk 0.5% of population = comprehensive assessment & care plan GP, Registered Nurse, Social Worker or Health professional facilitated to include for eg: •End of Life care •Hospital at home nursing •Specialised therapies (eg stoma care) •Continence care Risk High Risk High Risk Moderate Moderate RiskRisk Low LowRisk Risk 5% of population = integrated health and social care plan GP, Registered Nurse, Social Worker or health professional facilitated to include for eg: • Rehabilitation, recovery, reablement • Telehealth • Medication review 20% of population = self care plans Primary care identifies people with LTCs, disability, or social needs Proportionate assessment to create a co-produced, goal led care plan, for example: •Referral to Expert Patient Programme /peer educators /health trainers •LTC pathways eg., diabetes, dementia •Assistive technology / telecare 80+% of population = health promotion plans Primary care identifies people with lifestyle risks (eg. smoking, high blood pressure) Brief interventions to screen, give advice & refer or sign post: • Smoking cessation assistance • Exercise options •Depression / anxiety (referral to IAPT) •Social isolation (referral to 3rd sector support) •Housing related support AT RISK INDIVIDUALS PROGRAMME Risk Assessment Care Planning Stratification Predictive Risk Tool Funded Measuring Interventions Common assessment tools Consistent care planning system Interventions clinicians can deliver or refer to in order to provide extra support to patients Evaluation and outcomes measurement IMPLEMENTATION TASKS Finalise predictive risk tool – agree Develop and agree budgets – input vs. outcomes Develop and agree consistent assessment tools Develop roll out plan for e-shared care Agree core set of interventions to be consistent district-wide – both value add General Practice and second tier services Disease specific outcomes Patient experience and health status outcomes Acute demand outcomes 2. SERVICE REDESIGN WORKSHOP PARTICIPANTS Name Position Allan Moffitt Clinical Director, East Health and Alliance Health Plus Benedict Hefford Director, Primary Health & Community Services Beven Telfer GP Liaison - MMH Brad Healey GM, Medicine Campbell Brebner Chief Medical Advisor – Primary Health - MMH Denis Lee GP Pakuranga Medical Centre and Chair of East Health Trust Dot McKeen Manager, Middlemore Central Geraint Martin CEO Gillian Cossey GM Surgical & Ambulatory Care Jenni Coles Director, Hospital Services John Baird Facilitator Linda Bryant GM Eastern Lisa Gestro GM Primary Care & Service Dev. Lynda Irvine GM Manakau Locality Martin Chadwick Director, Allied Health - MMH Denise Kivell Director of Nursing – MMH Karyn Sangster Acting Nurse Leader, Primary Health Paulina Baird Facilitator Peter Didsbury Chair, Procare Networks Peter Gow Clinical Director - MMH Peter Watson Clinical Director – Mental Health - MMH Harry Rea Consultant – MMH and Professor of Integrated Care Simon Bowen GM Otara/Mangare Tim Hou GP – Mangere Health Centre Willem Landman Palliative Care Physician - MMH 17