Chapter 22: Cardiac Failure Cardiac failure means failure of the

Chapter 22: Cardiac Failure
Cardiac failure means failure of the heart to pump enough blood to meet the needs of the body
Effects of acute cardiac failure:
Less blood pumping
Poor pumping can cause decreased cardiac output, as well as damming of blood in the veins, causing increased venous pressure and right atrial pressure
Sympathetics then kick in quickly to fix all these effects
Sympathetic response to heart failure:
Baroreceptor reflex – triggered by decreased arterial pressure
Chemoreceptor reflex
CNS ischemic response
These 3 all trigger the sympathetics, which can then: o Stimulate the remaining functioning parts of the heart to be stronger and serve as a better pump to compensate for what was lost o Increase venous return, by increasing the blood vessel tone, which increases the mean systemic filling pressure, which increases blood flow from the veins to the heart
Increases right atrial pressure
Symps work quickly, so less severe MI’s might not present too harsh or long lasting symptoms
Chronic stage of heart failure will show retention of fluid by the kidneys, and some recovery by the heart over time
A low cardiac output will cause the kidneys to excrete less urine, & hold onto more salt & water o This raises blood volume and pressure, which increases the venous return, which increases CO
To increase the venous return, it works by doing 2 things:
It increases mean systemic filling pressure, which increases venous blood flow to the heart
It distends the veins, which reduces venous resistance
Increasing the venous return can make up for loss of up to half of the heart’s pumping ability
Loss of any more pumping ability causes too little blood flow to allow the kidneys to excrete as much salt and water as what’s taken in
Since heart is already at max pumping, the excess salt and water cause holding on to fluid that doesn’t help and just increases the workload on the heart, and can cause edema throughout the body
In severe heart failure, holding on to fluid increases the workload on the heart, overstretches the heart, both of which weaken the heart
Also causes pulmonary edema and systemic edema
o The pulmonary edema decreases O
2
in the blood
New collateral blood supplies branch out to the fringe of the infarcted areas to make them functional again o At the same time, the uninjured part of the heart hypertrophies
Compensated heart failure – when CO gets close to normal following an MI after weeks of fluid retention, so the body compensates for the heart failure
Can include increased right atrial pressure to increase the CO back to normal o Can happen in people without them knowing they have any heart issues, since the damage happened a little at a time, and compensation occurred with it each time
Exercising a heart under compensated heart failure will cause the symptoms of acute failure, because the heart can’t increase its pumping to meet what the tissues need cause the heart is already working very hard o This shows that cardiac reserve is decreased in compensated heart failure
When damage to the heart is too severe for symps or fluid retention to get CO back to normalish, the decreased CO isn’t enough to allow the kidneys to excrete much fluid, so fluid gets retained
This fluid retention leads to edema that can progress to death
Called decompensated heart failure – the heart failure is not compensated for
The increased blood volume increases mean systemic filling pressure, which increases blood back to the heart, which increases right atrial pressure o As right atrial pressure rises in heart failure, at the same time the heart functioning is
getting worse from stretching and edema, causing CO to fall more, causing more fluid retention o Eventually leads to the decompensated heart failure
Can be recognized by the edema being noticed as rales in the lungs, along with dyspnea
To treat decompensated heart failure: o Strengthen the heart enough to where it can pump enough blood get the kidneys working again o Diuretic drugs – will cause kidneys to excrete and hold less water and salt
Cardiotonic drugs, like digitalis, increase the strength of a failing heart
Don’t have much effect on a healthy heart
Strengthens by increasing the amount of calcium in muscle fibers o Done by inhibiting sodium-potassium ATPase, which inhibits the sodium-potassium pump, keeping sodium in the cell, which slows the sodium-calcium exchange pump, which normally trades out calcium to bring sodium back in
Sarcoplasmic reticulum in failing hearts can’t accumulate enough calcium, so therefore can’t release enough to cause contraction o Digitalis causes enough calcium to be there to allow contraction
When only the left heart fails, blood goes normally into the lungs, but dams in the left heart, increasing the mean pulmonary filling pressure
This causes the volume of blood in the lung to increase, which increases pulmonary capillary pressure, leading to pulmonary edema
Cardiogenic (circulatory) shock – heart doesn’t pump enough blood to meet the demand of the body tissues
The decreased blood pressure from the shock decreases blood to the heart even more, decreasing CO even more, decreasing pressure more, etc.
A patient will usually die before compensatory mechanisms kick in, so treatment is needed: o Can use digitalis, infusion of blood, or a drug to increase blood pressure
The heart is very slow to cause peripheral (systemic) edema
This is because acute heart failure often causes a decrease in peripheral capillary pressure o Aortic pressure falls, and atrial pressure rises
After a day of overall heart failure or right ventricular failure, the kidneys start holding water, leading to peripheral edema
Fluid retention increases mean systemic filling pressure, increasing blood to heart, increasing right atrial pressure o Also gets aortic pressure back to normal, allowing the capillary pressure to rise enough to cause edema
Causes of decreased excretion of urine by the kidney - decreased glomerular filtration rate, activating renin-angiotensin-aldosterone, and symps
Decreased glomerular filtration rate (GFR) o Decreased CO reduces glomerular filtration rate by decreasing arterial pressure, and triggering sympathetics that vasoconstrict the arterioles of the kidney o Even a slight decrease in glomerular filtration rate causes a big decrease in urine output
Activating the renin-angiotensin system o Decreased blood to the kidneys causes them to release renin, which causes the making of angiotensin 2 o Angiotensin 2 then decreases blood through the kidneys even more, which decreases the pressure in the capillaries around the renal tubules (peritubular capillaries), allowing more reabsorption of salt and water from the tubules
Increased aldosterone secretion o Angiontensin stimulates the adrenal cortex to secrete aldosterone, during the chronic stage of heart failure
Excess K + from the kidneys not working is also a powerful way to stimulate aldosterone
o Aldosterone further increases reabsorption of salt and water from the renal tubules
Water follows salt for 2 reasons:
Sodium reabsorption decreases the osmotic pressure in the tubules, and increases the osmotic pressure in the renal interstitial fluids, causing osmosis of water from the interstitium into the blood
Absorbed sodium and chloride increase the osmotic concentration throughout the body, causing the release of antidiuretic hormone (ADH) by the posterior pituitary, which promotes reabsorption of water
Activation of the sympathetics o Sympathetics cause reabsorption of salt and water by:
Vasoconstriction of the renal arterioles, decreasing glomerular filtration rate
Activating α adrenergic receptors on renal tubule epithelial cells to cause reabsorption of salt and water
Stimulating renin release, leading to angiotensin making
Stimulating the release of antidiuretic hormone by the posterior pituitary
Atrial natriuretic peptide (ANP) is a hormone released by the atrial walls of the heart when they become stretched, causing the kidneys to excrete salt and water
Heart failure causes increased atrial pressure that stretch the atrial walls
Acute pulmonary edema in patients who already have had chronic heart failure, can cause death
A temporary increased load on the already weak left ventricle causes damming of blood in the lungs
The increased blood in the lungs increases pulmonary capillary pressure, causing edema
The edema decreases the oxygenation of the blood
Peripheral vasodilation from lack of oxygen, increases venous return even more
The increased venous return causes more damming of blood in the lungs, leading to more edema, etc.
Once this cycle gets bad enough, it becomes irreversible and leads to death o Only way to stop it is rapid and heroic therapeutic measures:
Putting tourniquets on both arms and legs to keep the blood in the veins and decrease workload on the left heart
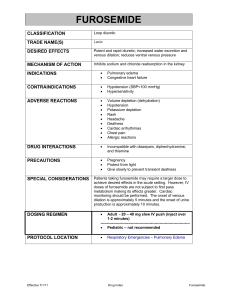
Giving a rapidly acting diuretic like furosemide, to causes rapid loss of fluid from the body
Giving them pure O
2
to breathe, to get enough O
2
to the tissues and stop vasodilation
Giving them a rapidly acting cardiotonic drug, like digitalis, to strengthen the heart
Cardiac reserve – the max percentage that the cardiac output can increase above normal
Healthy adult cardiac reserve = 300-400% , athletes can = 500% or more
There is no cardiac reserve in heart failure, it = 0%
Anything that prevents the heart’s ability as a pump will decrease the cardiac reserve
You diagnose low cardiac reserve with an exercise test: o People with low cardiac reserve usually don’t have symptoms until exercise o Usually use a treadmill or walking up stairs
Symptoms of low cardiac reserve: o Immediate and sometimes severe shortness of breath (called dyspnea), because heart can’t pump enough blood, so ischemia happens o Extreme muscle fatigue from the ischemia, which prevents the person from continuing to exercise o Excessive increase in heart rate because the symps overreact to try to fix that the cardiac output isn’t high enough
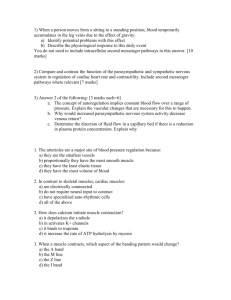
Graphing heart failure – page 262 and 263
In a normal graph of cardiac output and venous return against right atrial pressure, the only point where the circulatory system can work at is point A, where the CO & venous return meet
At the beginning of heart failure, CO decreases, and right atrial pressure increases
Then symps increase both the CO and venous return o Symps can also increase mean systemic filling pressure, shifting the venous return curve up and to the right
Over the next week, CO and venous return increase from salt and water retention, and some heart recovery, eventually getting CO back to normal o Right atrial pressure also increases o Normal CO makes the kidneys stop holding water o CO and right atrial pressure stay at this level now that CO is normal again, until some external factor affects it
Decompensated heart failure shows rising venous return curves from increased mean systemic filling pressure, but the CO never increases enough to stop the kidneys holding onto fluid, and leads to death o Treatment with digitalis can cause diuresis, which is when fluid is excreted by the kidneys o To compensate and stabilize the system, the CO, and venous return, and critical level for normal fluid balance, must all meet on the graph
Arteriovenous fistula is an opening between a large artery and a large vein
Overloads the heart by causing excessive venous return
Beriberi causes increased venous return from decreased resistance, and also depresses heart pumping
Beriberi is lack of thiamine