Ossification
advertisement

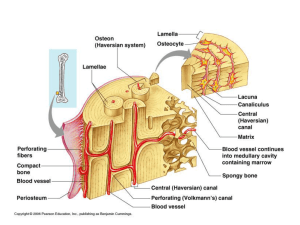
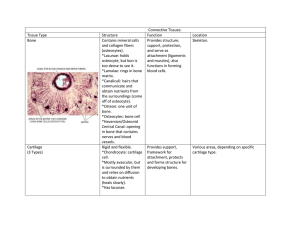
We created man from gentle extraction of clay; Then We placed him as (a drop of) sperm in a place of rest firmly fixed; Then We made the drop into an Alaqah (leech like); then We changed the leech like structure into a Mudghah (chewed substance); then We made out of the Mudghah bones and clothed the bones with flesh; then We developed out of it another creature: so blessed be Allah the Best creator! OSSIFICATION/OSTEOGENESIS/ HISTOGENESIS OF BONE Bone specialized connective tissue whose extracellular matrix is calcified, imprisoning the cells that secreted it. one of the hardest substances of the body dynamic tissue that constantly changes shape in relation to the stresses placed on it pressures applied to bone lead to its resorption, whereas tension applied to it results in development of new bone Applying these facts, the orthodontist is able to remodel the bone of the dental arches by moving and straightening the teeth to correct malocclusion This provides the patient with a more natural and pleasant smile. Functions of bones Primary structural framework for support and protection of the organs of the body Serve as levers for the muscles attached to them, thereby multiplying the force of the muscles to attain movement Reservoir -store about 99% of the body's calcium. Contain a central cavity, the marrow cavity, which houses the bone marrow, a hemopoietic organ. Composition Cells lying in an extracellular matrix that has become calcified. The calcified matrix is composed of fibers and ground substance. The fibers constituting bone are primarily type I collagen. The ground substance is rich in proteoglycans with chondroitin sulfate and keratan sulfate side chains. In addition, glycoproteins such as osteonectin, osteocalcin, osteopontin, and bone sialoprotein are present Osteons Bone Matrix Inorganic and organic constituents Inorganic ComponentCrystals of calcium hydroxyapatite [Ca10(PO4)6(OH)2], composed mostly of calcium and phosphorus. About 65% of dry weight Organic Component Predominantly type I collagen. About 35% of dry weight Collagen fibres Cells of Bone Osteoprogenitor cells Osteoblasts Osteocytes Osteoclasts. Osteoprogenitor Cells Derived from embryonic mesenchymal cells and retain their ability to undergo mitosis Located in the inner cellular layer of the periosteum, lining haversian canals, and in the endosteum Have the potential to differentiate into osteoblasts. Embryonic mesenchyme. Under certain conditions of low oxygen tension, these cells may differentiate into chondrogenic [cartilage forming]cells Most active during the period of intense bone growth OSTEOBLASTS synthesize the organic matrix of bone possess receptors for parathyroid hormone. derived from osteoprogenitor cells located on the surface of the bone in a sheet-like arrangement of cuboidal to columnar cells osteoblasts exocytose their secretory products, each cell surrounds itself with the bone matrix it has just produced when this occurs, the imprisoned cell is referred to as an osteocyte, and the space it occupies is known as a lacuna Most of the bone matrix becomes calcified Osteoblasts as well as osteocytes are always separated from the calcified substance by a thin, noncalcified layer known as the osteoid (uncalcified bone matrix). Osteocytes Mature bone cells derived from osteoblasts that became trapped in their lacunae Radiating out in all directions from the lacunaa are narrow, tunnel-like spaces (canaliculi) that contain cytoplasmic processes of the osteocyte. Processes make contact with similar processes of neighboring osteocytes, forming gap junctions through which ions and small molecules can move between the cells. Processes make contact with similar processes of neighboring osteocytes, forming gap junctions through which ions and small molecules can move between the cells Canaliculi also contain extracellular fluid carrying nutrients and metabolites that nourish the osteocytes. OSTEOCYTES OSTEOCLASTS Multinucleated cells originating from granulocyte-macrophage progenitors Play a role in bone resorption Occupy shallow depressions, called Howship's lacunae, that identify regions of bone resorption. PRIMARY BONE newly formed, immature bone, rich in osteocytes, with randomly arranged bundles of calcified collagen. Osteoclasts and osteoblasts are numerous in the surrounding endosteum. SECONDARY BONE organized as lamellae, seen faintly here as concentric lines surrounding osteonic canals An osteon. Lamellar bone: Perforating canals Hyaline cartilage INTRAMEMBRANOUS OSSIFICATION Direct formation of bone (membrane bone) within highly vascular sheets or ‘membranes’ of condensed primitive mesenchyme Mesenchymal stem cells differentiate into osteoprogenitor cells which proliferate around the branches of a capillary network, forming incomplete layers of osteoblasts in contact with the primitive bone matrix. Osteoblasts secrete a fine mesh of collagen fibres and ground substance, osteoid, from the surface which faces away from the blood vessels Earliest crystals appear in association with extracellular matrix vesicles produced by the osteoblasts Crystal formation subsequently extends into collagen fibrils in the surrounding matrix, producing woven bone As layers of calcifying matrix are added to these early trabeculae, the osteoblasts enclosed by matrix come to lie within primitive lacunae. Intramembranous ossification forming the nasal bones of a 7-month human fetus. Islands of bone (solid pink matrix [M], enclosing osteocytes) enlarge through the deposition of new matrix by osteoblasts (arrows). They subsequently fuse and are remodelled by osteoclasts to form mature lamellar bone ENDOCHONDRAL OSSIFICATION Requires the presence of a cartilage template Most of the long and short bones of the body develop by endochondral ossification Phases 1. 2. 3. Formation of a miniature hyaline cartilage model Continued growth of the model, which serves as a structural scaffold for bone development Eventual resorption and replacement by bone Cells and matrices of a primary ossification center. A small region of a primary ossification center showing key features of endochondral ossification. Compressed remnants of calcified cartilage matrix (dark purple), now devoid of chondrocytes, are enclosed by more lightly stained osteoid or bone matrix. This newly formed bone is surrounded by a layer of large, active osteoblasts. Some osteoblasts that were captured by the matrix have become smaller osteocytes (arrowheads). Zones of epiphyseal plate Zone of reserve cartilage: Chondrocytes randomly distributed throughout the matrix are mitotically active. Zone of proliferation: Chondrocytes, rapidly proliferating, form rows of isogenous cells that parallel the direction of bone growth. Zone of maturation and hypertrophy: Chondrocytes mature, hypertrophy, and accumulate glycogen in their cytoplasm The matrix between their lacunae narrows with a corresponding growth of lacunae. Zone of calcification: Lacunae become confluent, hypertrophied chondrocytes die, and cartilage matrix becomes calcified. Zone of ossification: Osteoprogenitor cells invade the area and differentiate into osteoblasts, which secrete matrix that becomes calcified on the surface of calcified cartilage This is followed by resorption of the calcified cartilage/calcified bone complex. Bone remodelling Fracture healing