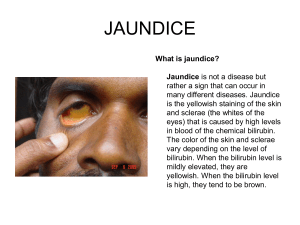
JAUNDICE
advertisement
D.D OF JAUNDICE BY DR. Hayam Hebah Associate Professor of Internal Medicine AL Maarefa College DEFINITION Jaundice is a yellowish staining of the skin, sclera, and mucous membranes by ↑ bilirubin. Clinically detected typically once the serum bilirubin level rises above 3 mg /dl. Can be caused by a wide variety of benign or life-threatening disorders. Pseudojaundice - a harmless form of jaundice in which the yellowing of the skin results from an excess of beta-carotene, not from an excess of bilirubin; usually from eating lots of carrots, pumpkin, or melon. N= 0.2-1 mg/dL (3.4-17.1 µmol/L), direct bil. ≤ 0.2 mg/dL (3.4 µmol/L) Pathophysiology Hepatic form of jaundice includes Dubin Johnson syndrome and Rotor syndrome. Bilirubin handling in Kidney Conjugated Bilirubin • Bound (20 days) • Bilirubin in urine is conjugated • Not filtered Unconjugated or secreted • Nil in urine Bilirubin Urobilinogen • Normally traces in urine • ↑ in Cholestaiss www.drsarma.in 6 DD OF UNCONJUGATED HYPERBILIRUBINEMIA(Prehepatic jaundice) Increased bilirubin production : -Hemolysis -Dyserythropoiesis -Hematoma Impaired hepatic bilirubin uptake : -Congestive heart failure - Portosystemic shunts -Drugs - Rifamycin, rifampin, probenecid Impaired bilirubin conjugation :-Crigler-Najjar syndrome types I and II - Gilbert syndrome (decreased uptake and/or conjugation) -Neonatal physiologic jaundice -Breast milk jaundice -Hypothyroidism/hyperthyroidism -Ethinyl estradiol -Liver diseases - Chronic hepatitis, cirrhosis, and Wilson disease Gilbert Syndrome AD, low glucuronyl transferase enzyme, low uptake of bilirubin, diagnosed by a history and physical examination and confirmed by standard blood tests. Repeated investigations and invasive procedures are not usually justified for establishing a diagnosis. Hyperbilirubinemia( mild) is the only biochemical serum abnormality in Gilbert syndrome. Serum bilirubin concentrations range from 1-5 mg/dL. 2 provocative tests, energy deprivation and nicotinic acid administration, have been used to diagnose the condition. SO FASTING IS associated with ↑ jaundice. Does not need ttt Hepatocellular jaundice Parenchymal liver disease , enables liver to transport bilirubin to bile. Both conjugated and unconjugated bilirubin increase Occur in acute or chronic liver disease. Associated with ↑ transaminases(AST , ALT) , GGT, ALP may also ↑ POSTHEPATIC(OBSTRUCTIVE ) (CHOLESTATIC) JAUNDICE Mechanism of jaundice: 1. Failure of hepatocytes to initiate bile flow 2. Obstruction of bile ducts or portal tracts. 3. Obstruction of bile flow in the extrahepatic bile ducts between the porta hepatis and ampulla of Vater. Causes of cholestatic jaundice Intrahepatic Primary biliary cirrhosis Primary sclerosing cholangitis Alcohol Drugs as OCP, hepatic infiltration (lymphoma, granuloma,amyloid,metasta ses) cystic fibrosis severe bacterial infections Pregnancy Chronic rt heart failure Inherited cholestatic liver disease Extrahepatic Carcinoma Ampullary Pancreatic Bile duct (cholangiocarcinoma) Liver metastasis Choledocholithiasis Parasitic infection Traumatic biliary strictures Chronic pancreatitis. Suggestive clinical features of cholestatic jaundice Static or increasing jaundice Fluctuating jaundice Abdominal pain Cholangitis Abdominal scar Irregular hepatomegaly Palpable GB Abdominal mass Occult blood in stools. Key diagnostic points in history in patients with jaundice History of itching preceding the jaundice(obstructive d.t bile acids) Abdominal pain( stones) Weight loss (CLD or malignancies) Urine and stool colors Fever ± rigors (cholangitis) Drug history Alcohol intake Iv drug abuse or blood transfusion Travel history Autoimmune diseases or IBD history Potential toxins (eg, drugs), environmental chemicals (eg, solvents), or wild mushrooms must be carefully excluded(toxic hepatitis). Risk factors for viral hepatitis should be elicited : Transfusion ,IV drug use ,multiple sexual partners ,exposure to a person who is infected. Colicky abdominal pain or fever suggests gallstone disease. Weight loss or constitutional systems suggests malignancy or chronic infection. Recent anesthesia with halothane suggests halothane hepatitis. A history of intense pruritus suggests cholestatic disease . A family history of jaundice suggests inborn errors of bilirubin metabolism. In patients with severe intercurrent illnesses, consider sepsis, hepatic ischemia, and opportunistic infections. Severe right heart failure or tricuspid insufficiency with hepatomegaly suggests hepatic congestion. Patients on parenteral nutrition may experience cholestasis that sometimes improves with the addition of lipid infusions. Patients with AIDS may experience biliary obstruction from opportunistic infections (e g, AIDS cholangiopathy). Patients with chronic liver disease may experience transient elevation of their bilirubin levels following blood transfusion, which results due to a more rapid turnover of the infused cells. In patients younger than 20-25 years, a history of a recent flulike syndrome treated with aspirin raises the possibility of Reye syndrome. Pregnancy suggests benign recurrent cholestasis or, in late pregnancy, acute fatty liver of pregnancy. Examination: Depending on the underlying illness, stigmata of chronic liver disease may or may not be present. Palpation of the abdomen may reveal the following: A mass (eg, a distended gallbladder, abdominal tumors) Tenderness over the liver (eg, as in cases of hepatitis or hepatic distention resulting from congestion or infiltrative disease) Tenderness over the gallbladder fossa (as occurs in cases of biliary disease or infection) Unexplained darkening of the skin, diabetes, or heart failure suggests hemochromatosis. Kaiser-Fleisher rings suggests Wilson disease. Cutaneous or neurologic findings of chronic alcoholism may be helpful diagnostic findings. In addition to color of sclera it self . Differential Diagnosis of Conjugated Hyperbilirubinemia I. Acute or Chronic Hepatocellular Dysfunction A. Infection Viral hepatitis A-E Cytomegalovirus (CMV) hepatitis Epstein-Barr virus hepatitis Sepsis B. Inflammation Without Toxic Infection liver injury Drug toxicity (eg, acetaminophen) Halothane hepatitis Alcoholic hepatitis Iron overload (hemochromatosis) Copper overload (Wilson disease) Autoimmune hepatitis C. Metabolic Dysfunction Ischemia ("shock liver") Acute fatty liver of pregnancy Alpha-1 antitrypsin deficiency Preeclampsia Reye syndrome Total parenteral nutrition D. Inborn Errors of Metabolism Dubin-Johnson syndrome Rotor syndrome Benign recurrent cholestasis II. Diseases That Prevent Flow of Bile into the Intestine A. Damage to Intrahepatic Bile Ducts or Portal Tracts Primary biliary cirrhosis Graft versus host disease Sclerosing cholangitis. Veno-occlusive disease B. Damage to or Obstruction of Larger Bile Ducts Choledocholithiasis Sclerosing cholangitis AIDS cholangiopathy Hepatic arterial chemotherapy Postsurgical strictures Bile duct cancers Developmental disorders of the bile ducts (eg, Caroli) Extrinsic compression of the bile duct Tumors Acute pancreatitis c. Diffuse Infiltrative Diseases Granulomatous diseases Sarcoidosis Disseminated mycobacterial infections Lymphoma Wegener granulomatosis Amyloidosis Diffuse malignancy D. Diseases That Interfere with Biliary Secretion of Bilirubin Anabolic steroids (testosterone, norethandrolone) Antithyroid agents (methimazole) Azathioprine (Immunosuppressive drug) Chlorpromazine HCI (Largactil) Clofibrate, Erythromycin estolate Oral contraceptives (containing estrogens) Oral hypoglycemics (especially chlorpropamide) ALGORITHMIC APPROACH FOR JAUNDICE First Step : estimate serum bilirubin if> 1 mg /dl so it is elevated. Second Step : is the hyperbilirubinemia conjugated (>20%) or unconjugated or both? Third Step : If CSB is increased , do AST, ALT, serum alkaline phosphatase & GGT. Fourth Step : If hepatocellular: 1. hepatitis markers, EBV, CMV 2. toxic hepatitis : drugs & alcohol 3. Malignancy: alpha fetoprotein 4. Cirrhosis: ALD-NAFLD ↑ in Unconjugated Bilirubin Hemolytic Jaundice - Uncommon 1. Hemolytic Disorders + Anemia Inherited – Sphero, SS, G6PD, PK Acquired – MAHA, PNH 2. Ineffective Erythropoesis –B12, Fe, F 3. Drugs – Rifampicin, Probenecid 4. Inherited –Crigler Najjar, Gilberts www.drsarma.in 30 Other helpful tests: Complete blood cell (CBC) count to screen for hemolysis Serologic screen for viral hepatitis, including hepatitis C virus (HCV) antibody and hepatitis B surface antigen (HBsAg) or antihepatitis B core antibody (anti-HBcAb) Alkaline phosphatase (ALP): If elevated or if an obstruction is suspected, images of the bile ducts should be obtained. Gammaglutamyl transpeptidase (GGTP) results may help differentiate a hepatic source of the elevated ALP from bone or other causes. Blood alcohol or acetaminophen levels upon admission (may be useful in certain cases). Antimitochondrial antibody (AMA)when considering primary biliary cirrhosis Antinuclear antibodies (ANAs), smooth-muscle antibodies, and when considering autoimmune hepatitis Iron and genetic studies when considering hemochromatosis Copper and ceruloplasmin when considering Wilson disease Alpha-1 antitrypsin fractionation and other studies when considering hereditary liver diseases AND ABDOMINAL U/S AUTOIMMUNE HEPATITIS More in females 2nd &3rd decades but may occur in any age or sex. Clinical presentation: acute or chronic hepatitis well-established cirrhosis rarely fulminant hepatic failure marked bycoagulopathy and jaundice 1/3 of patients present with symptoms of acute hepatitis marked by fever, hepatic tenderness, and jaundice. Chronic liver disease . CONDITIONS ASSOCIATED WITH AUTOIMMUNE HEPATITIS: Hashimoto thyroiditis Thyrotoxicosis Myxedema Pleurisy Coombs positive hemolytic anemia Ulcerative colitis SLE Rheumatoid arthritis Sjogren ‘s syndrome Diabetes Membranoproliferative GN Celiac disease. Common findings on physical examination are as follows: Hepatomegaly (83%) Jaundice (69%) Splenomegaly (32%) Spider angiomata (58%) Ascites (20%) Encephalopathy (14%) Lab diagnosis: Elevated aminotransferase levels (1.5-50 times reference values) Elevated serum immunoglobulin G (IgG) Mild to moderately elevated serum bilirubin and alkaline phosphatase – In 80-90% of patients; a sharp increase in the values during the course of autoimmune disease may reflect the development of primary sclerosing cholangitis (PSC) or the onset of hepatocellular carcinoma as a complication of cirrhosis Seropositive results for antinuclear antibodies (ANAs), smooth-muscle antibodies (SMAs), or liver-kidney microsomal type 1 (LKM-1) or anti–liver cytosol 1 (anti-LC1) antibodies Hypoalbuminemia and prolongation of prothrombin time – Markers of severe hepatic synthetic dysfunction, which may be observed in active disease or decompensated cirrhosis the hematologic abnormalities may include the following: Mild leukopenia Normochromic anemia Coombs-positive hemolytic anemia Thrombocytopenia Elevated erythrocyte sedimentation rate Eosinophilia (uncommon) Management: Corticosteroids, alone or in combination with azathioprine, have been the mainstays of drug therapy for patients with autoimmune . Relapse occurs in 50% of patients within 6 months of treatment withdrawal and in 80% of patients within 3 years of treatment. Reinstitution of the original treatment regimen usually induces another remission; however, relapse commonly recurs after a second attempt at terminating therapy. Patients who relapse twice require indefinite therapy with either prednisone or azathioprine. Liver transplantation for patients in whom medical therapy has failed or for those with decompensated cirrhosis caused by autoimmune hepatitis. FOR patients who present with fulminant hepatic failure secondary to autoimmune hepatitis. Primary Sclerosing Cholangitis Narrowed abnormal intra-heptic bile ducts. Normal Extra hepatic BD THANK YOU