Most Probable Number (MPN)
advertisement

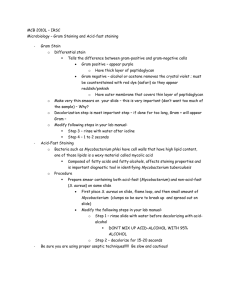
Counting Microorganisms Methods • • • • Turbidity measurements Viable counts Most probable number Direct counts Most probable Number: MPN – Based on Probability Statistics – Presumptive test based on given characteristics – Broth Technique Most Probable Number (MPN) • Begin with Broth to detect desired characteristic • Inoculate different dilutions of sample to be tested in each of three tubes -1 Dilution -2 -3 -4 -5 -6 3 Tubes/Dilution 1 ml of Each Dilution into Each Tube After suitable incubation period, record POSITIVE TUBES (Have GROWTH and desired characteristics) MPN - Continued • Objective is to “DILUTE OUT” the organism to zero • Following the incubation, the number of tubes showing the desired characteristics are recorded • Example of results for a suspension of 1g/10 ml of soil • Dilutions: -1 -2 -3 -4 • Positive tubes: 3 2 1 0 – Choose correct sequence: 321 and look up in table Pos. tubes 0.10 0.01 0.001 3 2 1 MPN/g (mL) 150 – Multiply result by middle dilution factor » 150 X 102 = 1.5 X 104/mL » Since you have 1g in 10mL must multiply again by 10 » 1.5 X 105/g Direct Counts • The sample to be counted is applied onto a hemacytometer slide that holds a fixed volume in a counting chamber • The number of cells is counted in several independent squares on the slide’s grid • The number of cells in the given volume is then calculated Determining the Direct Count • Count the number of cells in three independent squares – 8, 8 and 5 • Determine the mean – (8 + 8 + 5)/3 =7 – Therefore 7 cells/square 7 Determining the Direct Count (Cont’d) 1mm Depth: 0.1mm 1mm • Calculate the volume of a square: = 0.1cm X 0.1cm X 0.01cm= 1 X 10-4cm3 or ml • Divide the average number of cells by the the volume of a square – Therefore 7/ 1 X 10-4 ml = 7 X 104 cells/ml 8 Problem • A 500μl sample is applied to a hemacytometer slide with the following dimensions: 0.1mm X 0.1mm X 0.02mm. Counts of 6, 4 and 2 cells were obtained from three independent squares. What was the number of cells per milliliter in the original sample if the counting chamber possesses 100 squares? Microscopy Differential Staining Differential Staining Gram Stain Divides bacteria into two groups Gram Negative & Gram Positive • Stained Purple – Rods • Genera Bacillus and Clostridium – Coccus • Genera Streptococcus, Staphylococcus and Micrococcus Gram Negative • Stained Red – Rods: • Genera Escherichia, Salmonella, Proteus, etc. – Coccus: • Genera Neisseria, Moraxella and Acinetobacter Rule of thumb • If the genus is Bacillus or Clostridium = Gram (+) rod • If the genus name ends in coccus or cocci (besides 3 exceptions, which are Gram (-)) = coccus shape and Gram (+) • If not part of the rules above, = Gram (-) rods Gram + Cell Wall Vs Gram - Peptidoglycan wall Plasma Membrane Absent Lipopolysaccharide layer 15 Method – Primary staining 1. Staining with crystal violet 2. Addition of Gram’s iodine (Mordant) + + + Wall:peptidoglycan Plasma membrane + + + + + + + + + + + + LPS --------------Gram positive --------------Gram negative Method – Differential step 3. Alcohol wash Wall is dehydrated – Stain + iodine complex is trapped Wall: peptidoglycan Plasma membrane Wall is not dehydrated – Complex is not trapped LPS - - +- - -+- - +- - -+- - + - - -+ + Gram positive - - +- - -+- - +- - -+- - + - - -+ + Gram negative Method – Counter Stain 4. Staining with Safranin + + + + + + + Wall:peptidoglycan Plasma membrane + + + + + + + + LPS - - +- - -+- - +- - -+- - + - - -+ + Gram positive --------------Gram negative 18 Summary Fixation Primary staining Crystal violet Wash Destaining Counter staining Safranin 19 Acid Fast Staining • Diagnostic staining of Mycobacterium – Pathogens associated with Tuberculosis and Leprosy – Cell wall has mycoic acid • Waxy, very impermeable Method • Basis: – High level of compounds similar to waxes in their cell walls, Mycoic acid, makes these bacteria resistant to traditional staining techniques Method (Cont’d) • Cell wall is permeabilized with heat • Staining with basic fuchsine – Phenol based, soluble in mycoic layer – Cooling returns cell wall to its impermeable state • Stain is trapped • Wash with acid alcohol – Differential step • Mycobacteria retain stain • Other bacteria lose the stain Spore Stain • Spores: – Differentiated bacterial cell – Resistant to heat, desiccation, ultraviolet, and different chemical treatments • Thus very resistant to staining too! – Typical of Gram positive rods • Genera Bacillus and Clostridium – Unfavorable conditions induce sporogenesis • Differentiation of vegetative cell to endospore – E.g. Anthrax Malachite Green Staining • Permeabilization of spores with heat • Primary staining with malachite green • Wash • Counter staining with safranin Sporangium (cell + endospore) Vegetative cells (actively growing) Spores (resistant structures used for survival under unfavourable conditions.) Endospore (spore within cell) Pathogens 19th Century: Robert Koch • Studies anthrax disease which kills cows • Grows in pure culture bacteria obtained from the blood of diseased animals – Bacillus anthracis • Observations: – Blood of diseased animals transmits the disease – The microorganisms is found only in diseased animals – The microorganism grown in the lab transmits the disease to healthy animals 26 Robert Koch (Cont’d) • Conclusion: Microorganisms are responsible of diseases – Pathogens • These results lead Robert Koch to formulate guidelines to associate a microorganism to a disease – Koch’s postulates 27 Koch’s Postulates • The microorganism must be present in each diseased case but absent from healthy individuals • The microorganism must be isolated and grown in pure cultures • The disease must develop when the isolated microorganism is inoculated in a healthy host • The same microorganism must be isolated again from the diseased host 28