Acid and Base Balance and Imbalance
advertisement

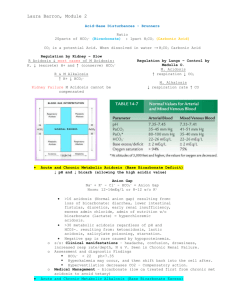
Mohammed A. Almeziny BPharm.RPh. Msc. PhD Clinical Pharmacist 1 Homeostasis of pH is tightly controlled Extracellular fluid = 7.4 Blood = 7.35 – 7.45 < 6.8 or > 8.0 death occurs Acidosis (acidemia) below 7.35 Alkalosis (alkalemia) above 7.45 2 3 Most enzymes function only with narrow pH ranges Acid-base balance can also affect electrolytes (Na+, K+, Cl-) Can also affect hormones 4 Cardiovascular Pulmonary (e.g., impaired oxygen delivery, respiratory muscle fatigue, dyspnea), Renal (e.g., impaired contractility, arrhythmias), (e.g., hypokalemia) Neurologic (e.g., decreased cerebral blood flow, seizures, coma). Acids take in with foods Acids produced by metabolism of lipids and proteins Cellular metabolism produces CO2. 6 Balance maintained by: Buffering systems Lungs Kidneys 1-Buffer systems Prevent major changes in pH Act as sponges… H+ 3 main systems • • • Bicarbonate-carbonic acid buffer Phosphate buffer Protein buffer H+ H+ Sodium Bicarbonate (NaHCO3) and carbonic acid (H2CO3) Maintain a 20:1 ratio : HCO3- : H2CO3 HCl + NaHCO3 ↔ H2CO3 + NaCl NaOH + H2CO3 ↔ NaHCO3 + H2O 9 Major intracellular buffer H+ + HPO42- ↔ H2PO4- OH- + H2PO4- ↔ H2O + H2PO42- 10 Includes hemoglobin, work in blood and ISF Carboxyl group gives up H+ Amino Group accepts H+ 11 Exhalation of carbon dioxide respiratory control center in the medulla to increase the rate and depth of ventilation. Peripheral chemoreceptors (located in the carotid arteries and the aorta) activated by arterial acidosis, hypercarbia (elevated PaCO2), and hypoxemia (decreased PaO2). Central chemoreceptors (located in the medulla). activated by cerebrospinal fluid (CSF) acidosis and by elevated carbon dioxide tension in the CSF 12 Powerful, but only works with volatile acids Doesn’t affect fixed acids like lactic acid CO2 + H20 ↔ H2CO3 ↔ H+ + HCO3Body pH can be adjusted by changing rate and depth of breathing 13 Can eliminate large amounts of acid Can also excrete base Can conserve and produce bicarb ions Most effective regulator of pH If kidneys fail, pH balance fails 14 Buffers function almost instantaneously Respiratory mechanisms take several minutes to hours Renal mechanisms may take several hours to days 15 16 pH< 7.35 acidosis pH > 7.45 alkalosis The body response to acid-base imbalance is called compensation May be complete if brought back within normal limits Partial compensation if range is still outside norms. 17 If underlying problem is metabolic, hyperventilation or hypoventilation can help : respiratory compensation. If problem is respiratory, renal mechanisms can bring about metabolic compensation. 18 Principal effect of acidosis is depression of the CNS through ↓ in synaptic transmission. Generalized weakness Deranged CNS function the greatest threat Severe acidosis causes Disorientation coma death 19 Alkalosis causes over excitability of the central and peripheral nervous systems. Numbness Lightheadedness It can cause : Nervousness muscle spasms or tetany Convulsions Loss of consciousness Death 20 21 Respiratory Acidosis Respiratory Alkalosis Metabolic Acidosis Metabolic Alkalosis Carbonic acid excess caused by blood levels of CO2 above 45 mm Hg. Hypercapnia – high levels of CO2 in blood Chronic conditions: Depression of respiratory center in brain that controls breathing rate – drugs or head trauma Paralysis of respiratory or chest muscles Emphysema 23 Acute conditons: Adult Respiratory Distress Syndrome Pulmonary edema Pneumothorax 24 Kidneys eliminate hydrogen ion and retain bicarbonate ion 25 Breathlessness Restlessness Lethargy and disorientation Tremors, convulsions, coma Respiratory rate rapid, then gradually depressed Skin warm and flushed due to vasodilation caused by excess CO2 26 Restore ventilation Treat underlying dysfunction or disease 27 28 Carbonic acid deficit pCO2 less than 35 mm Hg (hypocapnea) Most common acid-base imbalance Primary cause is hyperventilation 29 Conditions that stimulate respiratory center: Oxygen deficiency at high altitudes Pulmonary disease and Congestive heart failure – caused by hypoxia Acute anxiety Fever, anemia Early salicylate intoxication Cirrhosis Gram-negative sepsis 30 Kidneys conserve hydrogen ion Excrete bicarbonate ion 31 Treat underlying cause Breathe into a paper bag IV Chloride containing solution – Cl- ions replace lost bicarbonate ions 32 33 Bicarbonate deficit - blood concentrations of bicarb drop below 22mEq/L Causes: Loss of bicarbonate through diarrhea or renal dysfunction Accumulation of acids (lactic acid or ketones) Failure of kidneys to excrete H+ 34 Normal AG Hypokalemic Diarrhea Fistulous disease Ureteral diversions Type 1 RTA Type 2 RTA Carbonic anhydrase inhibitors Hyperkalemic Hypoaldosteronism Hydrochloric acid or precursor Type 4 RTA Potassium-sparing diuretics Amiloride Spironolactone Triamterene Elevated AG Renal Failure Lactic Acidosis (see Table 10-5) Ketoacidosis Drug Intoxications Starvation Ethanol Diabetes mellitus Ethylene glycol Methanol Salicylates AG, anion gap; RTA, renal tubular acidosis. Headache, lethargy Nausea, vomiting, diarrhea Coma Death 36 Increased ventilation Renal excretion of hydrogen ions if possible K+ exchanges with excess H+ in ECF ( H+ into cells, K+ out of cells) 37 Treat underlying cause IV Bicarbonate solution 38 39 Bicarbonate excess - concentration in blood is greater than 26 mEq/L Causes: Excess vomiting = loss of stomach acid Excessive use of alkaline drugs Certain diuretics Endocrine disorders Heavy ingestion of antacids Severe dehydration 40 Respiratory compensation difficult – hypoventilation limited by hypoxia 41 Respiration slow and shallow Hyperactive reflexes ; tetany Often related to depletion of electrolytes Atrial tachycardia Dysrhythmias 42 Treat underlying disorder Electrolytes to replace those lost IV chloride containing solution 0.1 N HCL Infusion rate 0.2 mmol/kg/hr Central line Acetazolamide 43 44 Disorder Metabolic acidosis Respiratory acidosis Metabolic alkalosis Respiratory alkalosis Arterial pH Primary Change Compensatory Change ↓ ↓HCO3- ↓PaCO2 ↓ ↑PaCO2- ↑HCO3- ↑ ↑HCO3- ↑PaCO2 ↑ ↓PaCO2- ↓HCO3- Arterial Blood Gas (ABG) Arterial carbon dioxide tension (PaCO2). Serum bicarbonate (HCO3-). Arterial oxygen tension (PaO2) pH <7.35, the patient is considered academic >7.45, the patient is considered alkalemic ABGs Normal Range pH 7.36–7.44 PaO2 90–100 mmHg PaCO2 35–45 mmHg HCO3- 22–26 mEq/L The concentration of all the unmeasured anions in the plasma eg lactate, acetoacetate, sulphate. Anion gap = [Na+] - [Cl-] - [HCO3-] Reference range is 8 to 16 mmol/l. Adjusted AG = AG + 2.5 × (normal albumin – measured albumin in g/dL Clinical Use of the Anion Gap To signal the presence of a metabolic acidosis and confirm other findings Help differentiate between causes of a metabolic acidosis To assist in assessing the biochemical severity of the acidosis and follow the response to treatment Osmolality mOsm/kg H2O= (1.86[Na])+([glucose (mmol/L)])+([BUN mmol/L]) Osmolal gap= measured Osmolality- Calculated Osmolality exists when the measured and calculated values differ by >10 mOsm/kg Obtain a detailed patient history and clinical assessment. Check the arterial blood gas, sodium, chloride, and HCO3-. Identify all abnormalities in pH, PaCO2, and HCO3-. Determine which abnormalities are primary and which are compensatory based on pH. If the pH is <7.40, then a respiratory or metabolic acidosis is primary. If the pH is >7.40, then a respiratory or metabolic alkalosis is primary. If the pH is normal (7.40) and there are abnormalities in PaCO2 and HCO3-, a mixed disorder is probably present because metabolic and respiratory compensations rarely return the pH to normal. Consider other laboratory tests to further differentiate the cause of the disorder. If the AG is normal, consider calculating the urine AG. If the AGis high and a toxic ingestion is expected, calculate an osmolal gap. If the AG is high, measure serum ketones and lactate. Always calculate the AG. If ≥20, a clinically important metabolic acidosis is usually present even if the pH is within a normal range. If the AG is increased, calculate the excess AG(AG-10). Add this value to the HCO3- to obtain corrected value. If corrected value >26, a metabolic alkalosis is also present. If corrected value is <22, a nonanion gap metabolic acidosis is also present. Consider other laboratory tests to further differentiate the cause of the disorder. If the AG is normal, consider calculating the urine AG. If the AGis high and a toxic ingestion is expected, calculate an osmolal gap. If the AG is high, measure serum ketones and lactate. Compare the identified disorders to the patient history and begin patient-specific therapy. 57 59