Acid-Base Imbalance - Metropolitan Community College
advertisement

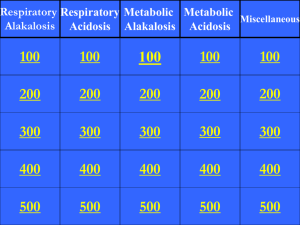
Acid-Base Imbalance Metropolitan Community College Fall 2013 Acid Base Balance Hydrogen ions - Low concentrations but highly reactive Concentration affects physiological functions Alters protein and enzyme functioning Can cause cardiac, renal, pulmonary abnormalities Alters blood clotting, Metabolization of meds Acid and Bases Acids – compounds that form hydrogen ion in a solution Bases – compounds that combine with hydrogen ion in a solution Proton donors Strong acids give up their hydrogen ion easily Weak acids hold on to their hydrogen ion more tightly Proton acceptors Neutralizes 20:1 ratio (20 parts bicarbonate to one part carbonic acid) What is pH? pH is a measurement of the acidity or alkalinity of the blood. It is inversely proportional to the number of hydrogen ions (H+) in the blood. The more H+ present, the lower the pH will be. The fewer H+ present, the higher the pH will be. Homeostasis keeps pH in a very narrow range 7.35-7.45 for optimum functioning 6.8-7.8 compatible with life Blood pH Blood pH < 7.40 acidosis Blood pH > 7.40 alkalosis Body Acids Respiratory Acid - CO2 – eliminated by lungs (288 L/day) Metabolic acids: Lactic acids Pyruvic acid Ketoacids (DKA) Acetoatic acids Beta-hydrobutyric acids Very little metabolic acid is produced on a daily basis Metabolized by the liver or eliminated by the kidneys Four Basic Categories of Abnormalities Respiratory acidosis Respiratory alkalosis Lower than normal level of carbon dioxide leading to an alkaline pH Metabolic acidosis Excess of carbon dioxide leading to an acid pH Excess of hydrogen ion or a deficiency in bicarbonate leading to an acid pH Metabolic alkalosis Excess of bicarbonate leading to an alkaline pH Buffer Systems Like a sponge Extracellular Buffers Soaks up extra ions Squeezed when there’s not enough Carbonic acid: controlled by respiration Bicarbonate: controlled by excretion Intracellular Buffers Phosphate Buffer System Dihydrogen phosphate (H2PO4) – hydrogen donor or acid Hydrogen phosphate (HPO4) – hydrogen acceptor or base Buffer Systems Protein Buffers In the blood Plasma Proteins Hemoglobin: deoxygenated is better than oxygenated at buffering Bones Carbonate and phosphate salts in bone provide a long term supply of buffer. In acute metabolic acidosis bone takes up hydrogen in exchange for calcium, sodium, and potassium. Role of the Lungs Regulate plasma pH minute to minute by regulating the level of Carbon Dioxide (CO2) Carbon Dioxide is measured as a partial pressure of carbon dioxide in arterial blood PaCO2 35-45mmHg Lungs alter rate and depth of ventilations in order to retain or excrete CO2 Minute Volume – Tidal Volume Ventilation is measured by how much air the lungs move in one minute (minute ventilation) Minute Ventilation is the product of respiratory rate and depth and is referred to as the TIDAL VOLUME (Vt) Normal depth tidal volume is about 500ml Normal respiratory rate is 12 breaths per min 12 breaths x 500 ml = 6000 ml or 6 liters Anatomic Dead Space The volume of air that doesn’t reach the alveolar airspace Estimated at 1ml/lb of ideal body weight 150lb of ideal body weight = 150ml of dead space Tidal volume – dead space = alveolar volume Trachea & Bronchi Doesn’t take part in gas exchange 500ml – 150ml = 350ml RR x alveolar volume = minute alveolar ventilation 12 x 350ml = 4200ml or 4.2 L/min Hypercarbic Drive Respiratory center in the medulla controls the rate and depth of ventilation Responds to levels of arterial CO2, denoted as PaCO2 Chemoreceptors in the medulla come into contact with CSF As PaCO2 rises the arterial PaCO2 reaches equilibrium with the CO2 in the CSF The CO2 in the CSF dissociates into hydrogen ions The hydrogen ions stimulate the chemoreceptors in the medulla which in turn stimulates the diaphragm and intercostal muscles Respiratory rate and depth increase and CO2 is blown off Hypoxic Drive There are also peripheral chemoreceptors Respond to levels of Carotid arteries Bifurcation of the common carotid and arch of aorta Oxygen in the blood or PaO2 Hydrogen ions or pH Carbon dioxide in the blood or PaCO2 As PaO2 falls below 60 mmHg the respiratory center is stimulated to increase rate and depth The role of the Kidneys Two main functions to maintain acid/base Secrete hydrogen ions Restore or reclaim bicarbonate (HCO3) In high metabolic acidosis, the kidneys can excrete ammonia as a urinary buffer. In alkalosis - the kidneys retain hydrogen ion and excrete bicarbonate to correct the pH. In acidosis - the kidneys excrete hydrogen ions and conserve bicarbonate to correct the pH. Very slow process Assessment of ACID BASE Arterial Blood Gases (ABG) most often and the most accurate to assess acid base balances. Serum Electrolytes can help fine tune acid base analysis NORMAL ABG VALUES: pH = 7.35 to 7.45 PaCO2 = 35 – 45 mEq/L HCO3 = 22 – 28 mEq/L Steps to Interpret ABG’s 1. 2. 3. 4. Assess the pH Assess the respiratory component – PaCO2 Assess the metabolic component – HCO3, base excess Evaluate compensation Compensation Once the primary cause is identified look at the other value If the value is abnormal but moving in the right direction to bring pH back to normal compensation is occuring If the pH value is normal than compensation is complete Because renal compensation is slower you can infer whether respiratory abnormalities are acute or chronic If kidneys have had time to compensate is chronic If the kidneys have not had time to compensate its acute Respiratory Acidosis Respiratory system fails to keep up with the body’s CO2 production Causes (pg. 442) Acute: drug overdose, head trauma, spinal cord injury, upper airway obstruction, pneumothorax Chronic: obesity, MS, emphysema, spinal cord injury Clinical Manifestations Anxiety, irritability, confusion, lethargy, increased heart rate, warm flushed skin Mainly seen with acute causes because chronic patients have compensated Respiratory Acidosis Medical treatment Treat the underlying problem Increase ventilation BiPAP Intubation Supplemental oxygen (care must be taken with chronic pts) Nursing care Assess PaCO2 levels and pH. Observe for signs of respiratory distress: restlessness, anxiety, confusion, tachycardia Encourage fluid intake Position patients with head elevated 30 degrees Administer oxygen with care Respiratory Alkalosis Most common cause is hyperventilation caused by anxiety, panic, or pain Stroke Meningitis Head trauma Clinical Manifestations Anxious Tachycardia Tachypnea Vertigo Forgetfulness Respiratory Alkalosis Medical treatment Treat underlying cause of condition Sedation may be needed Nursing care Administer sedatives or pain medications Provide emotional support Encourage patient to breathe slowly, which will retain carbon dioxide in the body Breath into a paper bag Metabolic Acidosis Increase in total body acid Causes (pg. 442) Starvation Diarrhea Renal failure Diabetic ketoacidosis Signs and symptoms Kussmaul respirations Altered LOC Headache V tach Metabolic Acidosis Medical treatment Treat the underlying disorder Nursing care Monitor VS & ECG Assess neurological status Provide emotional support Metabolic Alkalosis An accumulation of base or a loss of acid in the ECF Causes (pg. 442) Prolonged nasogastric suctioning or excessive vomiting Diuretics Electrolyte disturbances Large volume blood transfusions, increased citrate Clinical Manifestations Lethargy Altered LOC Tetany ECG changes Metabolic Alkalosis Medical Treatment Treat the underlying disorder Nursing care Monitor VS & ECG Monitor labs Accurate I&O including the amount of fluid removed by suction Provide emotional support Use isotonic saline solutions rather than water for irrigating NG tubes because the use of water can result in a loss of electrolytes A client’s blood gas results are pH 7.36, PaCO2 50, HCO3 30. What do these results indicate to the nurse? A. B. C. D. Respiratory acidosis, compensated Metabolic acidosis, compensated Metabolic acidosis, uncompensated Respiratory acidosis, uncompensated Reference Osborn, Wraa, & Watson chapter 19