Chapter 5 - Choteau Schools
advertisement
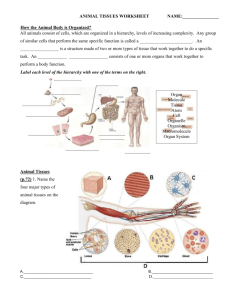
Chapter 5 - Tissues Introduction and Epithelial Tissues Background • Tissues are layers or groups of similar cells that have a common function. • Tissues can be identified by variations in cell size, shape, organization, and function. • The study of tissues is called histology. Types of Tissues • The human body has 4 major types of tissues: – Epithelial – Connective – Muscle – Nervous • These four types of tissue comprise organs. Types of Tissues Epithelial Tissues • Found throughout the body. – Cover the surface of the body – Cover organs – Form the inner lining of body cavities – Line hollow organs Epithelial Tissues • Structure – Always have a free (or apical) surface • One side of the tissue is exposed to the outside or to an open space on the inside – The other surface (underside) is anchored to connective tissue by a thin, nonliving layer call the basement membrane. – Lack blood vessels (avascular) • Nutrients diffuse into the epithelial tissue from the underlying connective tissue • Cells are tightly packed, readily divide, and often have desmosomes Epithelial Tissues • Functions – Protection • Cells divide easily to rapidly heal injuries • Cells are tightly packed (often connected by desmosomes…see p. 80) which allow the tissue to form a protective barrier – Secretion – Absorption – Excretion Epithelial Tissues • Classification – Classified according to the shape and number of layers of cells • Squamous – Composed of thin, flattened cells • Cuboidal – Composed of cube-like cells • Columnar – Composed of elongated cells • Simple – Composed of a single layer of cells • Stratified – Composed of two or more layers of cells Epithelial Tissues Simple Squamous Epithelium • Consists of a single layer of thin, flattened cells that fit tightly together and usually have broad and thin nuclei. • Found at sites of diffusion and filtration since substances can easily pass through the tissue. – Location examples: lines the air sacs (alveoli) of the lungs and the insides of blood and lymph vessels, forms the walls of capillaries, covers the membranes that line body cavities • Easily damaged because it is so thin. Simple Squamous Epithelium Simple Cuboidal Epithelium • Consists of a single layer of cube-shaped cells that usually have centrally located, spherical nuclei. • Locations: – Lines the follicles of the thyroid gland, lines the kidney tubules, lines the ducts of certain glands (such as the salivary glands, pancreas, and liver), and covers the ovaries. • Simple cuboidal epithelium functions in tubular secretion and reabsorption in the kidneys and secreted glandular products in the glands. Simple Cuboidal Epithelium Simple Columnar Epithelium • Consists of a single layer of elongated cells whose nuclei are usually near the basement membrane. • Some cells of simple columnar epithelium can be covered with cilia or microvilli. – Cilia are 7-10 µm in length and move constantly to aid in movement of particles (such as an egg through the uterine tubes) – Microvilli (tiny, cylindrical processes) are 0.5 to 1.0 µm in length and increase the surface area of the cell membrane to aid in absorption • Nonciliated simple columnar epitheleum lines the uterus and portions of the digestive tract (such as stomach and small and large intestines). – This tissue functions as a protective layer (due to its elongated cells which make the tissue thick), a secretor of digestive fluids, and an absorber of nutrients from digested food • Flask-shaped glandular cells called goblet cells are also scattered among the simple columnar epithelium cells – These cells secrete a protective fluid (mucus) onto the free surface of the tissue. Simple Columnar Epithelium Microvilli Pseudostratified Columnar Epithelium • Consists of cells that appear to be layered (but are really not) because the nuclei are at two or more layers in a row of aligned cells. • Cells have cilia which sweep away mucus that is secreted from the goblet cells that are scattered throughout the tissue. – Psuedostratified columnar epithelium lines the passages of the respiratory system, allowing the dust and microorganisms that enter with the air to be trapped in the mucus and swept out of the airways by the cilia. Pseudostratified Columnar Epithelium Stratified Squamous Epithelium • Consists of many layers of cells which make the tissue thick. • Cells nearest the free surface are flattened whereas deeper cells are cuboidal or columnar. – This occurs because the deeper cells divide and then are pushed outward where they become flattened. • Locations: – Epidermis (outer layer of the skin) • In these layers the cells obtain a protein called keratin as they age and are pushed outward. • This process (called keratonization) results in dead cells that serve as a dry, tough, protective layer that prevents water and other materials from escaping from underlying tissues and blocks chemicals and microorganisms from entering. – Oral cavity, esophagus, vagina, and anal canal • In these tissues, the outer cells remain living, keeping the tissue soft and moist. Stratified Squamous Epithelium Stratified Cuboidal Epithelium • Consists of two or three layers of cuboidal cells that form the lining of a lumen (which is a space within a tubular structure such as a blood vessel or intestine). – The layers provide more protection than a single layer. • Locations: – Lines the larger ducts of the mammary glands, sweat glands, salivary glands, and pancreas as well as lines developing ovarian follicles and seminiferous tubules. Stratified Cuboidal Epithelium Stratified Columnar Epithelium • Consists of several layers of cells. – The cells at the surface are elongated whereas the cells at the base are cube-shaped. • Found in part of the male urethra and parts of the pharynx. Stratified Columnar Epithelium Transitional Epithelium • Consists of tissue that is specialized to change in response to increases in tension. • Lines the urinary bladder, the ureters, and part of the urethra. – When the wall of one of these organs contracts, the transitional epithelium consists of several layers of cuboidal cells. – When one of these organs is distended, the tissue stretches and appears to contain only a few layers of cells. • Along with providing an expandable lining, transitional epithelium also forms a barrier that helps to prevent the contents of the urinary tract from diffusing back into the internal environment. Transitional Epithelium Glandular Epithelium • Consists of cells that are specialized to produce and secrete substances into ducts or body fluids. • Cells are found within columnar or cuboidal epithelium and constitute a gland. – Exocrine glands secrete their products into ducts that open onto surfaces (such as skin or the lining of the digestive tract). (Have ducts) – Endocrine glands secrete their products into tissue fluid or blood. (Do not have ducts) Glandular Epithelium • Structures of exocrine glands: – Unicellular glands • Consist of a single epithelial cell (such as a mucous-secreting goblet cell) – Multicellular glands • Consist of many cells and can be divided into simple and compound glands – A simple gland communicates with the surface by means of a duct that does not branch before reaching the glandular cells or secretory portion. – A compound gland has a duct that branches repeatedly before reaching the secretory position Glandular Epithelium • Simple and compound glands can further be classified in different manners: – According to the shapes of their secretory portions. • Tubular glands consist of epithelial-lined tubes • Alveolar glands have terminal portions that form saclike dilations • Branching and coiling of the secretory portions may also occur – According to the way products are secreted • Merocrine glands release fluid products by exocytosis – Most common type of exocrine secretory cell – Examples: pancreas, sweat glands – Further divided into serous cells and mucous cells » Serous cells (which are common in the linings of body cavities) secrete serous fluid which is watery and has a high concentration of enzymes » Mucous cells secrete a thicker fluid rich in the glycoprotein mucin called mucous (which is abundantly secreted from the inner linings of the digestive and respiratory systems) • Apocrine glands lose small portions of their glandular cell bodies during secretion • Examples: mammary glands, ceruminous glands • Holocrine glands release entire cells • Examples: sebaceaus glands Structures of Exocrine Glands Types of Glandular Secretions