Schizophrenia

“Halika dito”
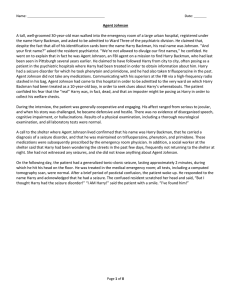
A Case of Schizophrenia
Asuncion, Dalman, Doromal, Dy,
Generoso
Identifying Data
• L.G.P.
• 28 year old
• Female
• Single
• Filipino
• Roman Catholic
• Unemployed
• College graduate
Chief Complaint
• May naririnig akong boses
History of Present Illness
10 years PTC
• Patient thinks that her dorm mates in Taiwan are making sign languages that are pertaining to her
9 years PTC
• Was sent home because condition worsened
• Started hearing familiar voices
Karen
Parents Cousins
Pricking sensation
History of Present Illness
• Sought psychiatric consult at
Mandaluyong
• Given levomepromazin 100 mg tab, half tab OD and fluphenazine decanoate 1cc every month
8 years PTC
Patient not compliant
• Taking levomepromazin only as needed for sleep
Persistence of symptoms prompted consult
Past Medical History
• Hospitalized, Measles
• No diabetes
• No HTN
• No allergies
• No asthma
Past Psychiatric History
• Previous consultation at a mental institution in
Mandaluyong, given medications and seeks monthly consult for intramuscular injections.
• Illness was never explained
OBGyne History
• LMP: 10/21/2010
• PMP: September 2010
• 3-4 days, 2 pads/day, 28-30 interval
• (-) dysmenorrhea
• Menarche 11 years old
• Coitarche 31 years old, denies contraceptive use
Family History
• HTN, BPH – father
• HTN – youngest brother
• Stroke – mother (deceased, tetanus)
• No psychiatric illnesses in the family
Past Social History
• Denies smoking and use of illicit drugs
• Occasional alcoholic drinker
ANAMNESIS
Early childhood
• 5 th of 6 children, NSD, (-) complications, primary caregiver: mother
• Father previous construction employee,
Mother (deceased, tetanus) housewife and disciplinarian
• Closer to her second older sister than most, although shares that she is not close to anyone in particular at all
Middle Childhood
• Cannot remember preschool experiences
• Public school, no separation anxiety, few friends, average grades
• Best friend during elementary school was a neighbor named Karen, although they were not schoolmates
Late Childhood
• High school at same institution, average academic achievement, no organizational activities
• No specific area of interest, no romantic involvement, few friends
• Her and Karen were just acquaintances but different barkada, no issues or problems with her
• No drug use, or smoking. Occasional alcohol drinking with family and peers
Young Adulthood
• Computer secretary at National Teacher’s College, finished college on time with average grades
• First time to leave home and live alone (dorm), no adjustment problems
• Relationships
– Sited her room mate as a real friend
– First romantic relationship lasted 1 month and ended due to a suspected 3 rd party
– Coitarche with 3 rd boyfriend, afterwards relationship ended
– Currently takes care of her father
Young Adulthood
• Work
– Department store clerk, Robinson’s, 1 year
– Coating biscuits, Taiwan factory, 1 year. Delusions prompted her to not renew contract and return home
– Bantay Bata (2004), 2 weeks training. Auditory hallucinations recurred prompting her to quit
– Currently unemployed, expressed desire to work, but not actively looking
• Currently lives at home with her father.
Dependent on father’s retirement benefits
PHYSICAL EXAM
Physical Examination
• Awake, alert, coherent, ambulatory, not in cardiorespiratory distress
• 130/90
• HEENT: anicteric sclera, pink conjunctiva, no tonsilopharyngeal congestion, no lymphadenopathies
• Respiratory: full, equal chest expansion, clear breath sounds, no rales/ rhonchi/ retractions
Physical Examination
• Cardio: adynamic precordium, normal rate, regular rhythm, no murmurs
• Abdomen: no lesions/ scars, flat, soft, normoactive bowel sounds, non-tender, no organomegaly
• DRE: not done
• Extremities: full equal pulses, CRT <2secs, no edema
Neuro Examination
• Cranial Nerves: intact
• Motor: normal gait, no unnecessary movements, 5/5 in all extremities
• Sensory: no deficits
• DTR: ++ in all
MENTAL STATUS EXAM
Mental Status Exam
• 32 year old female, looks appropriate for age, wearing glasses, dressed in jeans and a sweater. Middle built.
• Not agitated, no mannerisms
• Exemplified appropriate behavior, not easily distracted and maintained eye contact during the interview
Mental Status Exam
• Speech was spontaneous, normoproductive but with occasional stuttering, no flight of ideas
• Mood was euthymic, with appropriate affect
• At the time of interview with no visual, auditory or tactile hallucinations but admits to auditory and tactile hallucinations last heard yesterday
Mental Status Exam
• She exhibits thought blocking, unable to finish statements and thought was preoccupied with whether the voices she hears are heard by others also
• No suicidal or self-harming thoughts
• Had good attention but poor concentration exhibited by missing 4 of 5 in serials 7
Mental Status Exam
• Intact recent, recent past and past memory
• Oriented to person, place and time
• With poor insight to illness, still unable to distinguish whether some of the voices she hears are just herself or others are really saying it
Salient Features
• 28 year old
• Female
• History of tactile and auditory hallucinations
• Persecutory delusions
• Previous psychiatric consult
• Prescribed antipsychotics with poor compliance, some improvement in symptoms
Salient Features
• MSE Findings:
– Appropriately dressed
– Some poor concentration
– Thought blcking
– Intact memory
– Oriented
– Poor insight
MULTI-AXIAL
DIAGNOSIS
• AXIS I: Schizophrenia, Paranoid type
• AXIS II: none
• AXIS III: none
• AXIS IV: poor social group support, unable to work, financially limited
• AXIS V: 61-70
Schizophrenia
(DSM IV Criteria)
A. Characteristic symptoms: 2 or more present in a 1 month period
1. Delusions
2. Hallucinations
3. Disorganized speech
4. Grossly disorganized or catatonic behavior
5. Negative symptoms: affective, flattening, alogia or avolition
B. Social/occupational dysfunction
C. Duration: disturbance persists for at least 6 months
DIFFERENTIAL DIAGNOSIS
DISCUSSION
Case Discussion
• Psychosis
– State in which the person’s thought, affective response, ability to recognize reality, and ability to communicate and reality to others are sufficiently impaired
– A break from reality involving delusions,
perceptual disturbances and/or disordered thinking
Case Discussion
• Delusions
– Fixed false beliefs that cannot be altered by rational arguments and cannot be accounted for by cultural background
– Types
• Paranoid
• Ideas of reference
• Thought broadcasting
• Delusions of grandeur
• Delusions of guilt
Case Discussion
• Perceptual Disturbances
– Hallucination – sensory perception without external stimulus
• Auditory – most commonly schizophrenia patients
• Visual – drug intoxication
• Olfactory – aura, assoc epilepsy
• Tactile – secondary to drug abuse, withdrawal
– Illusion – misinterpretation of an existing sensory stimulus
Case Discussion
• Disordered thought
– Thought content – reflect patient’s beliefs, ideas, interpretation of his/her surroundings (e.g. paranoid delusions, ideas of reference)
– Thought process – manner in which patient links words and ideas together (e.g. thought blocking, looseness of associations, tangentiality)
Case Discussion
• Psychotic Disorders
– Schizophrenia
– Schizophreniform Disorder
– Brief Reactive Psychosis
– Delusional Disorder
– Schizoaffective Disorder
– Substance-Induced Psychosis
– Psychotic Features Of Mood Disorders
– Psychotic Features Of Organic Mental Disorders
Schizophrenia
• Three Phases
– Prodromal – decline in functioning preceding first psychotic episode, e.g. socially withdrawn, irritable, may have physical complaints or newfound interest in religion/ occult
– Psychotic – perceptual disturbances, delusions, and disordered thought process/ content
– Residual – occurs between episodes of psychosis, i.e. flat affect, social withdrawal, odd thinking or behavior (negative symptoms)
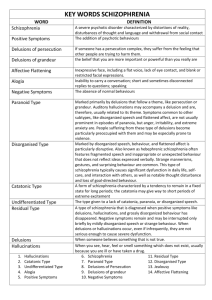
Schizophrenia
• Subtypes
– Paranoid – highest functioning, older age of onset
A. Preoccupation with 1 or more delusions or frequent auditory hallucinations
B. No predominance of disorganized speech, disorganized or catatonic behavior, or inappropriate affect
– Disorganized – poor functioning type, early onset
A. All are prominent
1. Disorganized speech,
2. Disorganized or catatonic behavior,
3. Inappropriate affect
B. Criteria not met for Catatonic type
Schizophrenia
• Subtypes
– Catatonic type – rare
A. Dominated by at least 2 of the ff:
1. Motor immobility
2. Excessive purposeless motor activity
3. Extreme negativism or mutism
4. Peculiar voluntary movements or posturing
5. Echolalia or echopraxia
– Undifferentiated type
• Present symptoms meet Criterion A, but do not meet those for paranoid, disorganized or catatonic type
Schizophrenia
• Subtypes
– Residual type – prominent negative symptoms with minimal evidence of positive symptoms
A. Absence of prominent delusions, hallucinations, disorganized speech, and grossly disorganized or catatonic behavior.
B. There is continuing evidence of the disturbance, as indicated by the presence of negative symptoms or two or more symptoms listed in Criterion A for schizophrenia, present in an attenuated form (e.g., odd beliefs, unusual perceptual experiences)
Pathophysiology
• Dopamine Hypothesis
– Increased dopamine activity in neuronal tracts
• Prefrontal cortical: negative symptoms
• Mesolimbic: positive symptoms
– Treated with dopamine receptor antagonist
– Cocaine and amphetamines (increased dopamine activity) = gives schizophrenic-like symptoms
MANAGEMENT
Pharmacologic
• Neuroleptics
– Typical
• Dopamine (mostly D
2
) antagonist, positive symptoms
• Side Effects: extrapyramidal symptoms, neuroleptic malignant syndrome, tardive dyskinesia, akathisia, acute dystonia
• e.g. Chlorpromazine, Haloperidol, Fluphenazine*,
Flupenthhixol, Thioridazine, Trifluoperazine
Pharmacologic
• Neuroleptics
– Atypical
• Higher serotonin (5HT
2
) than dopamine receptor antagonist,
negative symptoms
• Side Effects: lower incidence of extrapyramidal symptoms, substantial weight gain, increased risk for diabetes mellitus, for monitoring of glucose abnormalities
• e.g. Risperidone*, Clozapine, Olanzapine, Quetiapine
Psychotherapy
• Psychosocial approach
– Psychiatric Rehabilitation
• Range of interventions designed to help people improve their functioning and quality of life
• By enabling them to acquire the skills and supports needed to
be successful in usual adult roles and in the environments of their choice
• Emphasizes independence, community integration, and
patient preferences rather than professional goals
Psychotherapy
• Social Skills (Behavioral) Therapy
– Modality of social skills training
• Role play of simulated conversations. The trainer first provides instruction on how to perform the skill and model the behavior to demonstrate how it is performed
Psychotherapy
• Family Therapy
– Altering the interactions between or among family members, seeking to improve the functioning of the family as a unit, and/or the functioning of individual members of the family
– Aimed at increasing the family’s coping with schizophrenia and at
reducing the family’s expressed emotion aimed at individual goals
(e.g., social functioning) as well as family goals
Other forms of therapy
• Supportive psychotherapy
• Support groups
• Advocacy for mental health
PUBLIC HEALTH
World Health Report, 2001
• Advances in neuroscience and behavioral medicine have shown that, like many physical illnesses, mental and behavioral disorders are the result of a complex interaction between biological, psychological and social factors
Epidemiology
• Affects ~1% of people
• Men and women equally affected
– Men present at 20 years, more severe, more negative symptoms, less able to function in society
– Women present at 30 years
• Rare <15 years and >45years
• Strong genetic predisposition
• Strong association with substance use and depression
Stigma of Mental Disorders
• Higher in urban areas and higher levels of education
• Downward Drift Hypothesis
– Schizophrenia Unable to function well Enter lower socio-economic groups (e.g. homeless people)
Good Prognosis
• Later onset
• Good social support
• Positive symptoms 40%-50% remain significantly impaired
•
• Mood symptoms
Acute onset
• Female sex
• Few relapses
20%-30% function socially w/ medications
• Good pre-morbid functioning
“Halika dito”
A Case of Schizophrenia
Asuncion, Dalman, Doromal, Dy,
Generoso