osce cases - respiratory
advertisement

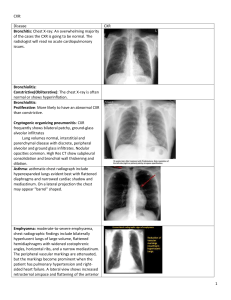
ISCEE Respiratory System 23rd Nov 2010 CASE PRESENTATION 1 Mrs R, 44 years old lady with no previous medical or surgical history Main complaint was painful red eye for one year associated with discomfort, photophobia and blurred vision. Seen by ophthalmologist and diagnosed with bilateral chronic uveitis She was then investigated to determine aetiology She has a history of Bells Palsy which resolved spontaneously after one week and a history of hyper-pigmented scaly lesion on forehead. There is no history of cough or dyspnoea. No history suggestive of TB No history of joint pain. Examination On examination she was a well looking young, not dyspnoeic, BP 129/88 PR 93/minute No significant lymphadenopathy Hyper pigmented lesions on the forehead Chest clear CVS :NAD Abdomen no organomegaly Musculoskeletal system: no arthritis and no muscle weakness CNS: NAD No cranial nerve palsy, no peripheral neuropathy Investigation FBC: Normal U&E: Normal LFT: Normal CALCIUM LEVEL: Slightly raised ESR: 40mm per hour ANF: Negative SACE LEVEL: 111 (Normal less than 52) LUNG FUNCTION TEST: Normal CHEST X RAY (next slide) SARCOIDOSIS Multisystem inflammatory disease of unknown etiology that predominantly affects the lungs. Manifested by the presence of non-caseating granulomas (NCGs) that may affect any organ system The many forms and presentation of this disease and the lack of a single diagnostic test can make the diagnosis challenging The lungs are involved in more than 90 percent of patients, with sarcoid usually presenting as interstitial disease. Symptoms are dry cough, dyspnea, and chest discomfort. Pulmonary sarcoidosis has an unpredictable course that may result in spontaneous remission or lead to progressive loss of lung function with fibrosis. Airway involvement can occur and may result in airflow limitation, persistent cough and, in severe cases, bronchiectasis. Treatment The majority of patients will have spontaneous remission and a generally benign clinical course. Treatment is reserved for patients with worsening pulmonary function tests patients with worsening pulmonary symptoms (cough, shortness of breath, chest pain or hemoptysis) and patients with extra pulmonary sarcoidosis including arthritis, neuropathy, cardiac and renal sarcoid, also in, patient with intractable fatigue, weakness or fever. Corticosteroids are the mainstay of therapy. Generally, prednisone given daily and then tapered over a 6month course is adequate for pulmonary disease. EPIDEMIOLOGY Sarcoidosis affects men and women of all races and ages Usually presents in adult younger than 40 years more frequent between 20 - 29 years, and slightly more predominant in women than in men. Course of sarcoidosis is variable, ranging from self limited acute disease to a chronic debilatating disease. Spontaneous remissions occur in nearly two thirds of patients. CASE 2 Case Presentation 2 63 years old female presented with gradual onset SOB over the last 6 months. She is known to suffer from Rheumatoid arthritis for the last 3 years and has been on treatment with methotrexate for the same. She has previously had an episode of pleural effusion which was drained and investigated but was found to be an exudate with high protein and low glucose. On examination she had dull percussion note and absent air entry in her left lower zone of the chest. Patient’s bloods were within normal limits. Chest x ray confirmed a pleural effusion. Overview Major catagories of pulmonary disease associated with RA: Pleural effusion Nodular lung disease Diffuse interstitial fibrosis BOOP (bronchiolitis obliterans organizing pneumonia) Pulmonary vasculitis Alveolar hemmorhage Obstructive disease Infections Rheumatoid Arthritis And The Lung Broad differential for pleuropulmonary disease in those with rheumatologic disorders: Secondary to, or associated with the underlying rheumatic disease Secondary to immunosuppression (infection) Secondary to drug therapy Coexistant medical problems Overlap syndromes Pleural Effusion Most common pulmonary manifestation of RA Often incidental finding on CXR Patients often asymptomatic ?Reduced physical activity prevents symptoms Most common symptoms: pleuritic pain, dyspnea, cough Pleural effusions can precede or occur simultaneously with joint symptoms in 25% More common in men with high RF titer and active arthritis Can be uni- or bilateral, resolve, recur or persist for months Post-mortem studies almost 50% of patients with RA have pleural effusions Pleural Effusion Treatment: None needed if asymptomatic Repeated thoracentesis or pleurodesis NSAIDs, steroids Intrapleural steroids Probably best to control the underlying RA Nodular Lung Disease Pulmonary nodules in RA first described by Caplan in 1953 Discovered multiple bilateral nodules on CXR of coal miners with RA Caplan’s syndrome: Pneumoconiosis in RA patient leading to multiple basilar pulmonary nodules and mild airflow obstruction Only pulmonary manifestation specific for RA Can occur before, with or after the joint manifestations of RA Usually asymptomatic, but can cause coughing and rarely hemoptysis Nodular Lung Disease Usually multiple, bilateral nodules Range from few millimeters to several centimeters in size Typically occur just below the pleura or associated with interlobular septa Can lead to bronchopleural fistula, pneumothorax, abcess or cavition Can remain static, resolve, increase in size or undergo malignant transformation More common in men, ?association with smoking Nodular Lung Disease Management usually observation suffices Transbronchial biopsy or transthoracic needle aspiration to rule out malignancy or other pathologic process Diffuse Interstitial Fibrosis More common in those with severe RA Most modifiable risk factor: smoking >25 pack-year smoking history significantly more likely to have radiographic evidence of ILD Usually occurs about five years after joint symptoms present, but can predate them Occurs mostly in those with subcutaneous nodules and high RF Symptoms: progressive SOBOE and productive cough most common Also: increased RR, clubbing, crepitations at lung bases, pulmonary hypertension CXR Reticulated pattern with progression to fine nodularity and honeycombing Diffuse Interstitial Fibrosis Prognosis is poor Treatment usually includes corticosteroids, azathioprine or other immunomodulating medications (e.g., cyclophosphamide) ?Single lung tranplantation Usually better results in those with RA associated interstitial fibrosis Usually too many comorbidities for transplantation surgery (e.g., osteoporosis, decreased mobility) Newer therapies (e.g., TNF blockers) Infections Persistent problem in those with RA Many confounding factors, especially corticosteroid or immunosuppressive medication May mask the signs of infection Lymphocyte abnormalities in RA? Patients with RA have greater occurrence of bronchitis, bronchiectasis and pneumonia than controls with degenerative joint disease Drug Related Pulmonary Disease Methotrexate: Presents with dyspnea, cough and fever Usually subacute 50% of cases diagnosed within 32 weeks of initiating MTX Re-challenge with MTX causes high rate of recurrence of lung injury 17% of patients who develop lung disease due to MTX will die of this complication