CXR: Disease CXR Bronchitis: Chest X
CXR:
Disease
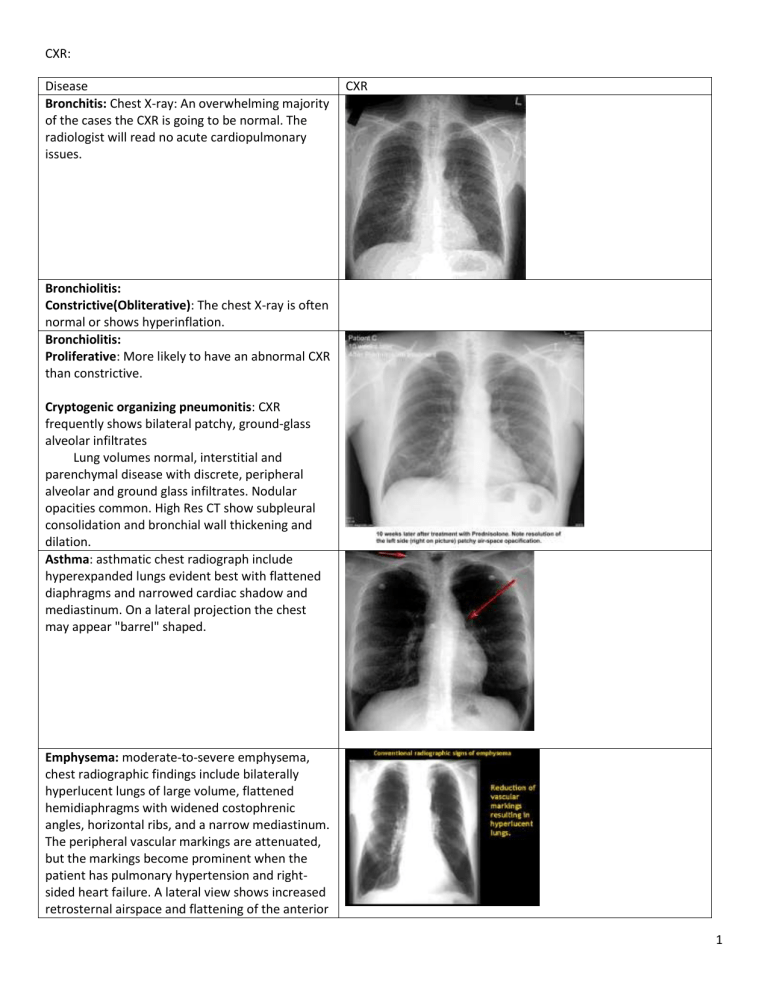
Bronchitis: Chest X-ray: An overwhelming majority of the cases the CXR is going to be normal. The radiologist will read no acute cardiopulmonary issues.
CXR
Bronchiolitis:
Constrictive(Obliterative): The chest X-ray is often normal or shows hyperinflation.
Bronchiolitis:
Proliferative: More likely to have an abnormal CXR than constrictive.
Cryptogenic organizing pneumonitis: CXR frequently shows bilateral patchy, ground-glass alveolar infiltrates
Lung volumes normal, interstitial and parenchymal disease with discrete, peripheral alveolar and ground glass infiltrates. Nodular opacities common. High Res CT show subpleural consolidation and bronchial wall thickening and dilation.
Asthma: asthmatic chest radiograph include hyperexpanded lungs evident best with flattened diaphragms and narrowed cardiac shadow and mediastinum. On a lateral projection the chest may appear "barrel" shaped.
Emphysema: moderate-to-severe emphysema, chest radiographic findings include bilaterally hyperlucent lungs of large volume, flattened hemidiaphragms with widened costophrenic angles, horizontal ribs, and a narrow mediastinum.
The peripheral vascular markings are attenuated, but the markings become prominent when the patient has pulmonary hypertension and rightsided heart failure. A lateral view shows increased retrosternal airspace and flattening of the anterior
1
diaphragmatic angle. In addition, bullae and an irregular distribution of the lung vasculature may be present
Bronchiectasis: Trim-track opacities, air-fluid levels may be seen in cystic bronchiectasis. Increase in bronchovascular markings, and bronchi seen end on may appear as ring shadows. Pulmonary vasculature appears ill-defined, thought to represent peribronchovascular fibrosis. SEEN IN
CYSTIC FIBROSIS.
Cystic Fibrosis: may be normal in those who have mild lung disease.
Peribronchial cuffing, mucus plugging, bronchiectasis(ring shadows and cysts), increased interstitial markings, small rounded peripheral opacietis, and focal atelectasis are common.
Pneumothorax can all be seen.
Community-Acquired Pneumonia (CAP):
Range from patchy airspace opacities to lobar consolidation with air bronchograms to diffuse alveolar or interstitial opacities. May also have pleural effusions and cavitation.
Nosocomial Pneumonia (HAP or HCAP): nonspecific and often confounded by other processes that led initially to hospitalization or ICU admission.
Lung abscess: appears as a thick-walled solitary cavity surrounded by consolidation. An air-fluid level is uslaly present.
Same as above!
2
Necrotizing pneumonia: multiple areas of cavitation within an area of consolidation.
Empyema is characterized by the presence of purulent pleural fluid and may accompany either of the other two radiographic findings.
Pulmonary Tuberculosis: primary disease includes small unilateral infiltrates, hilar and paratracheal lymph node enlargement, and segmental atelectasis. Pleural effusion is present in 30-40%.
Reactivation TB see with fibrocavitary apical disease, discrete nodules, and pneumonic infiltraties, usually in the apical or posterior segments of the upper lobes or in the superior segments of the lower lobes.
Miliary pattern (diffuse small nodular densities)
Resolution of active TB leaves: dense nodules in the pulmonary hila, w/ or w/o obvious calcifications, upper lobe fibronodular scarring and bronchiectasis with volume loss. Ghon(calcified primary focus) and Ranke(calcified primary focus and calicifed hilar lymph node).
Pulmonary disease caused by Nontuberculous
Mycobacteria: Infiltrates that are progressive or persist for at least 2 months, cavitary lesions and multiple nodular densities.
Interstitial lung disease (Diffuse Parenchymal
Lung disease): Low lung volumes and patchy distibrution of ground glass, reticular, nodular, reticulondular or cystic opacities.
Idiopathic interstitial pneumonias: Progressive fibrosis over several years and diffuse patchy fibrosis with pleural-based honeycombing on highres CT can.
3
Usual interstitial pneumonia (UIP): Diminised lung volume., Increased linear or reticular bibasilar and subpleural opacities. Unilateral disease is rare!!
Respiratory bronchiolitis-associated interstitial
lung disease (RB-ILD): May be indistinguishable from UIP. More often presents with a nodular or reticulonodular pattern. Honeycombing is rare.
Upperlobe emphysema
Acute interstitial Pneumonia (AIP): Diffuse bilateral airspace consolidation with areas of ground-glass attenuation on high-resolution CT scans
Nonspecific interstitial pneumonia (NSIP): May be indistinguishable from UIP. Most typical picture is bilateral areas of ground-glass attenuation and fibrosis on high res CT.
Sarcoidosis:
Stage one:Bilateral hilar adenopathy alone
Stage two: hilar adenopathy and parenchymal involvement
Stage three: parenchymal involvement alone
4
Pneumonia:
Parenchymal opacity or infiltrate
--Radiological patterns can be indeterminate and one infectious agent can produce many patterns*
Anatomic or radiologic distribution
*Lobar
*Multifocal or lobular (patchy opacity)
**Bronchopneumonia
*Interstitial
Pathologic patterns
*Consolidation, air bronchograms (see the bronchi)
*Silhouette sign
*Effusion
*Abscess, atelectasis (complications)
Pulmonary Venous Thromoboembolism: Normal in 12% of patients. Most frequent findings: atelectasis, parenchymal infiltrates and pleural effusions.
Get a CT or V/Q scan
Pulmonary Hypertension: In chronic disease, dilation of the right and left main and lobar pulmonary arteries and enlargement of the pulmonary outflow tract are seen. RT ventricular and RT atrial enlargement. Peripheral “pruning” of large pulmonary arteries.
5
Pulmonary vacuities (Wegener granulomatosis): fibrinoid necrotizing epitheloid and eosinophilic granulomas.
Coal Worker’s pneumoconiosis: formation of coal macules usually 2-5mm in diameter that appear as diffuse small opacities that are espically prominent with upper lung. (correlate with history)
Silicosis: Calcifications of the periphery of hilar lymph nodes (eggshell calcification)
Asbestosis:linear streaking at the lung bases, opacities of various shapes and sizes, and honeycomb changes in advanced cases. The presents of pleural calcifications may be a clue to
DX.
6
Hypersensitivity pneumonitis: small nodular densities sparing the apices and bases of the lungs
EX: farmer’s lung, bird fancier’s lung, mushroom picker’s disease…etc…
Pulmonary Radiation Fibrosis: Obliteration of normal lung markings, dense interstitial and pleural fibrosis, reduced lung volumes, tenting of the diaphragm, and sharp delineation of the irradiated area.
Pleural Effusion: Blunting of the costophrenic sulcus. Fluid may become trapped (loculated) by pleural adhesions.
Spontaneous Pneumothorax: Demonstration of a visceral pleural line. If there is a secondary pleural effusion will see an air-fluid level.
7
Tension Pneumothorax:Hyperlucent, overly expanded hemithorax, medistinal shift to the opposite side.
8