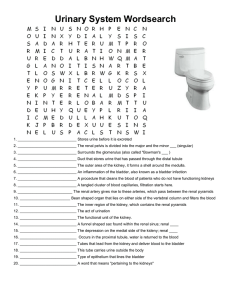
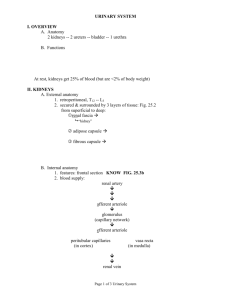
Chapter 26: Urinary System
advertisement

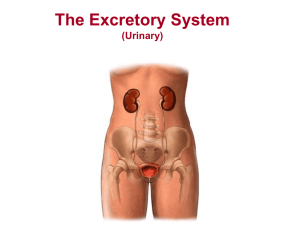
Chapter 26: The Urinary System BIO 211 Lab Instructor: Dr. Gollwitzer 1 • Today in class we will: – Identify the major function of the urinary system – Identify the major components of the urinary system and their functions – Trace the path of filtrate/urine through the urinary system – Begin our discussion on the organs and anatomical structures of the urinary system: • Kidneys – – – – – Gross anatomy Position Sectional anatomy Renal flow Blood supply and blood flow 2 Introduction • Major function: – To excrete waste products • 2 major components: – Kidneys: • Produce urine = – Fluid containing water, ions, small soluble compounds and toxic substances – Urinary tract: • Transports and stores urine prior to elimination • Consists of: – Ureters – paired tubes from the kidney to the bladder – Urinary bladder – muscular sac for temporary storage of urine – Urethra – from bladder to exterior • Kidneys urine ureters urinary bladder urethra exterior 3 Figure 26-1 4 Figure 26-3 5 Kidneys: Gross Anatomy • Paired organs on either side of vertebral column; left slightly superior to right • Reddish-brown, kidney-bean shaped • Adrenal glands on superior surface • Approximate size of hand • Hilum = depression where blood vessels (renal artery and vein) and lymphatic vessels, nerves, and ureter pass into/out of kidney 6 Figure 26-2a 7 Kidneys: Position • Retroperitoneal (“behind”): – Between muscles of dorsal body wall and parietal peritoneum – Behind parietal peritoneum of abdominal cavity in retroperitoneal space; separated by parietal peritoneum • Position in abdominal cavity maintained by: – Overlying peritoneum – Contact with adjacent visceral organs – 3 concentric layers of supportive CT 8 Figure 26-2b 9 Kidney: CT layers • Renal capsule – tough layer of collagen fibers, covers outer surface of kidney • Adipose capsule – thick middle layer, surrounds renal capsule; cushions kidney • Renal fascia – dense, fibrous outer layer (also surrounds adrenal gland) – Anchors kidney to surrounding structures – Fuses with deep fascia (surrounding muscles of body wall) and peritoneum – When renal fascia torn floating kidney • Dangerous because of potential twisting/kinking of ureters and blood vessels 10 Kidney: Sectional Anatomy • Renal cortex – outer layer in contact with renal capsule; appears grainy • Renal columns – bands of cortical tissue that extend into renal medulla and separate renal pyramids • Renal medulla: – Inner layer adjacent to renal cortex; looks like strands of combed hair – Consists of 6 – 18 renal pyramids (triangular structures) • Base of each pyramid in contact with cortex • Tip forms renal papilla • Striations = loops of Henle and collecting ducts of nephrons (functional units of kidney) • Ducts discharge urine in to cup-shaped minor calyx 11 Kidney Figure 26-4, a,b 12 Kidney: Sectional Anatomy • Renal lobe: – Functional component where urine production occurs – Consists of: • • • • Renal pyramid + Overlying renal cortex + Adjacent renal columns Note: Think 3D – visualize handful of waffle cones = Kidney – Ice cream = cortex – Cone = medulla – Paper around each cone = renal columns 13 Kidney: Renal Flow • Renal papillae from several renal pyramids discharge into a minor calyx • 4-5 minor calyces discharge into a major calyx • 2-3 major calyces form the renal pelvis = – Large funnel-shaped chamber that fills most of renal sinus and connects to ureter 14 Kidney • Renal sinus = internal cavity lined by inner surface of renal capsule 15 Nephrons • Microscopic, tubular structures in cortex of renal lobe • Functional/filtration unit of kidney = where urine production begins • Approx. 1.25 million/kidney • Consists of: – Renal corpuscle = filtering body – Renal tubule (equivalent to 85 miles) = urine collecting and concentrating tube 16 Figure 26-6, 7th edition 17 Kidney: Renal Corpuscle • Round structure consisting of: – Glomerulus – Bowman’s capsule 18 Kidney: Renal Corpuscle • Glomerulus – Ball of intertwined fenestrated capillaries (approx. 50) – Parietal and visceral epithelia separated by capsular space – Visceral epithelium • Covers glomerular capillaries • Consists of podocytes (= large simple squamous cells) with “feet” = pedicels • Narrow gaps between adjacent pedicels = filtration slits – allow filtrates to enter Bowman’s capsule 19 Kidney: Renal Corpuscle • Bowman’s capsule – Cup-shaped body – Encircles glomerular capillaries – Collects filtrate forced out of capillaries in capsular space – Connected to initial segment of renal tubule 20 Kidney: Renal Corpuscle • Blood arrives at renal corpuscle via afferent arteriole and leaves via efferent arteriole • In renal corpuscle, BP forces fluid and dissolved solutes out of glomerular capillaries (fenestrated) into capsular space (between glomerulus and capsule) = filtration protein-free solution (filtrate) 21 Figure 26-8 22 Kidney: Renal Tubule • Filtrate (tubular fluid) leaves renal corpuscle and enters renal tubule • Has 3 sections: – 2 coiled/twisted segments (located in the cortex) – Separated by a U-shaped tubule (located partially or completely in the medulla) 23 Kidney: Renal Tubule • Proximal convoluted tubule (PCT): – First segment that exits Bowman’s capsule in – Entrance opposite afferent/efferent arterioles • Loop of Henle: – Descending limb (turns toward renal medulla) – Ascending limb (turns toward cortex) • Distal convoluted tubule (DCT): – Passes between afferent and efferent arterioles – Empties into collecting duct in cortex 24 Figure 26-6, 7th edition 25 Kidney: Renal Tubule • Tubular fluid changes in composition as it travels through each segment of the nephron • Reabsorption of: – Useful organic compounds (glucose, fatty acids, amino acids, vitamins etc) – Ions (Na, K) – Water (>90%) from tubular fluid and release them into the peritubular fluid – • Secretion of waste products missed by filtration 26 Kidney: Juxtaglomerular Apparatus (JGA) • Located where DCT and afferent arteriole are in close contact with each other and the renal corpuscle • Formed by: – JG cells – Macula densa • An endocrine structure that secretes: – Hormone erythropoietin • In response to low O2 • Primary function – Enzyme renin: • Elevates BP and Na retention 27 Figure 26-8 28 Kidney: Types of Nephrons • Nephrons from different locations differ in structure • Cortical nephrons (85%) – in superficial cortex: – Short loop of Henle; descends only slightly into renal medulla – Efferent arteriole delivers blood to peritubular capillaries which surround entire renal tubule and drain into small venules interlobular veins • Juxtamedullary nephrons (15%) – near medulla: – Long loop of Henle extends deep into medulla – Peritubular capillaries connected to vasa recta = long, straight capillaries that parallel the loop of Henle 29 Figure 26-7 30 Figure 26–7 Kidney: Collecting System • Collecting duct: – Receives tubular fluid from DCT of several nephrons – Begins in cortex and ends in medulla (at papillary duct) • Papillary duct: – Receives fluid from several collecting ducts – Drains into minor calyx 31 Blood Supply to Kidneys • Major function of kidneys is to filter blood • Therefore, large volumes of blood delivered to kidneys (almost 20 gallons/hr!) • Blood flow: – Abdominal aorta renal artery segmental artery interlobar artery arcuate artery interlobular artery afferent arteriole renal corpuscle glomerulus efferent arteriole – For cortical nephrons: • peritubular capillary venule interlobular vein – For juxtamedullary nephrons: • peritubular capillary vasa recta venule interlobular vein – Interlobular vein arcuate vein interlobar vein segmental vein renal vein 32 Figure 26-5 33 • Today in class we will: – Continue our discussion on the organs and anatomical structures of the urinary system: • Urinary tract – Ureters – Urinary bladder – Urethra » Female » Male – Renal flow – Blood supply 34 Urinary Tract • Consists of: paired ureters, urinary bladder, urethra • Responsible for urine transport, storage, and elimination • Ureters: – Pair of muscular tubes from kidney renal pelvis to urinary bladder – Penetrate posterior, inferior wall of bladder – Ureteral openings are slits to prevent backflow of urine when bladder contracts – Every 30 seconds peristaltic contraction begins at renal pelvis and moves along ureter, forcing urine toward urinary bladder – Different pathways in males and females: • Due to variations in nature, size, position of reproductive organs • Males – base lies between rectum and pubic symphysis • Females – base sits inferior to uterus and anterior to vagina 35 Urinary Tract • Urinary bladder: – Hollow muscular organ/sac for temporary storage of urine; urine flows in until bladder distended and pressure closes urethral openings – Can contain approximately 1 L (stretch receptors triggered at approx 200 mL) – Held in place by umbilical ligaments – Internal surface: • Covered by transitional epithelium (“modified” columnar epithelium) • Has has rugae (folds) that disappear as bladder fills – Trigone • Triangular base (area bounded by ureteral openings and entrance of urethra) • Funnels urine into urethra as bladder contracts – Neck (surrounds urethral opening) • Contains internal urethral sphincter = smooth muscle involuntary control over discharge of urine from bladder – Smooth muscle layers of bladder wall form detrusor muscle – contraction compresses urinary bladder and expels contents into urethra 36 Urinary Tract • Urethra: – Extends from neck of urinary bladder to exterior of body – Drains urine from bladder to exterior opening of body (external urethral meatus/orifice) – Females and males differ in length and function • Female urethra: – Very short (1-2 in. long) – From bladder to vestibule – External urethral orifice/meatus = opening to outside between vagina and clitoris 37 Urinary Tract • Male urethra: – Extends from neck of bladder to tip of penis (6-8 in. long) – 3 sections: • Prostatic urethra - passes through prostate gland • Membranous urethra – Penetrates urogenital diaphragm (floor of pelvic cavity) – Surrounded by external urethral sphincter (in males and females) » = band of skeletal muscle » Acts as a valve - at rest, contracted; must be voluntarily relaxed to urinate • Penile (spongy) urethra – passes through penis: – From urogenital diaphragm – To external urethral orifice/meatus (opening to outside) 38 Figure 26-18 39