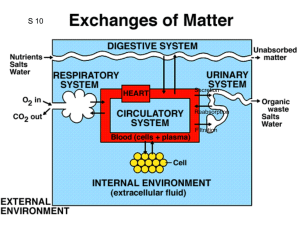
Basic Processes of Urine Formation
Lesson # 21
Chapter 26
Objectives:
1- Describe the basic processes responsible for urine formation.
2Discuss the factors that influence glomerular filtration pressure.
3Describe the hormone influence in the volume and concentration of urine.
The Urinary System 2
Basic Processes of Urine Formation
Different segments of the nephron form the urine by three different processes:
1- Filtration
Fenestrated endothelium of capillaries
It is produced in the renal corpuscle when the blood pressure (hydrostatic pressure) forces water through the filtration membrane.
Small solute molecules pass through pores and larger solutes and suspended materials are retained.
Blood pressure
Filtration
2- Reabsorption
It is the removal of water and useful solutes from the filtrate. It is a selective process.
It occurs after filtrate has left the renal corpuscle.
Blood Peritubular fluid
Renal tubule
Most of the reabsorbed materials are nutrients that the body can use.
Reabsorption
3- Secretion
It is the transport of solutes from the peritubular fluid to the filtrate.
Waste that did not pass by filtration.
Secretion
Almost any molecule smaller than 3 nm can pass freely through the filtration membrane:
1- Water, electrolytes, glucose, fatty acids, amino acids, nitrogenous wastes , and vitamins.
2- Some substances of low molecular weight are bound to the plasma proteins and cannot get through the membrane (most calcium, iron, and thyroid hormone).
Kidney infections and trauma can damage the filtration membrane and allow albumin or blood cells to filter.
Proteinuria (albuminuria):
It is the presence of protein in the urine.
Hematuria:
It is the presence of blood in the urine.
Turned back:
- Blood cells.
- Plasma proteins.
- Protein-bound minerals and hormones.
- Most molecules
> 8 nm in diameter.
Passed through filter:
- Water
- Electrolytes
- Glucose
- Aminoacids
- Fatty acids
- Vitamins
- Urea
- Acid uric
- Creatinine
BLOOD
PCT
REABSORPTION
It is the removal of water and useful solutes from the filtrate. It is a
selective process.
DCT
SECRETION
Secretion of ions, acids, drugs, toxins.
Water, ions and organic nutrients.
Renal corpuscle
FILTRATION
Small solute molecules pass through pores and larger solutes and suspended materials are retained.
Water Water
Sodium, Chloride Sodium, Chloride
Peritubular fluid
Water
Na + , K +
H + , CO
3
H -
NEPHRON LOOP
REABSORPTION
Further reabsorption of water, sodium and chloride ions.
COLLECTING DUCT
REABSORPTION and SECRETION
Variable reabsorption of water and reabsorption or secretion of sodium and potassium. Under control of Aldosterone and ADH.
Reabsorption or secretion of hydrogen, and bicarbonate.
It is an important site for the control of body fluid pH.
Na + , K +
H + , CO
3
H -
PAPILLARY DUCT
Delivery of urine to the minor calyx.
Filtration
Pressures
Efferent arteriole
Blood in glomerular capillaries
Plasma proteins
Capsular
Space
Hydrostatic
Pressure
Colloid Osmotic
Pressure
50 mm Hg
15 mm Hg
Net
Hydrostatic
Pressure:
50 – 15 =
35 mm Hg PCT
25 mm Hg
10 mm Hg
Net Filtration
Pressure:
35 – 25 =
10 mm Hg
Afferent arteriole
The concentration of sodium and chloride in the peritubular fluid produce an osmotic flow of water from the Distal Convoluted
Tubes and Collecting Ducts.
The Distal Convoluted Tubes and the
Collecting Ducts are relatively impermeable to water when ADH is not present.
The presence of ADH causes the appearance of special water channels
(aquaporins) in the membranes of the DCT and collecting ducts.
H
2
O
H
2
O H
2
O
H
2
O H
2
O
H
2
O H
2
O
H
2
O H
2
O
Small volume of concentrated urine
Large volume of dilute urine
The Control of Urine Volume and Osmotic
Concentration
1- Aldosterone
It is a steroid secreted by the adrenal cortex.
It stimulates the reabsorption of more Na + and secretion of
K + . Water and Cl follow the Na + .
The net effect is that the body retains NaCl and water and blood pressure rises.
2- Natriuretic Peptides (ANP and BNP)
They are secreted by the myocardium of the heart in response to high blood pressure.
They reduce thirst and block the release of Aldosterone and
ADH, thus increasing the diuresis and decreasing blood volume and pressure.
3- Antidiuretic Hormone (ADH)
It is secreted by posterior lobe of pituitary in response to dehydration and rising blood osmolarity.
It makes the collecting duct more permeable to water. Water in the tubular fluid reenters the tissue fluid and bloodstream rather than being lost in urine.
Consequently, less volume of more concentrated urine is produced.
ADH stimulates the hypothalamic thirst center.
4- Parathyroid Hormone (PTH)
It is secreted from parathyroid glands in response to calcium deficiency
It acts on PCT to increase phosphate excretion, and acts on the thick segment of the ascending limb of the nephron loop, and on the DCT to increase calcium reabsorption.