Drugs Affecting the Urinary System
advertisement

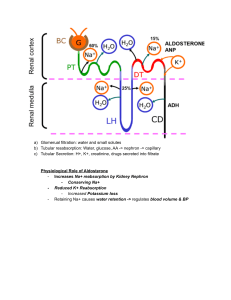
Drugs Affecting the Urinary System 1 Diuretics • Functions to lower blood pressure by primarily reducing Na reabsorption • Remember: Where sodium goes water will follow • Reduced Na reabsorption means that there is more Na in the filtrate and therefore also more water • Urine is more dilute • Systemic Effect: lower blood volume and therefore decreased blood pressure • More useful for mild to moderate hypertension 2 Thiazide Diuretics • Blocks Na/Cl transporter in distal convoluted tubule • Inhibit the transport of sodium by these cells • The diminished sodium gradient in the medulla interferes with the production of a concentrated urine • Larger amounts of a dilute urine are produced, causing a loss of water from the body and a decreased blood pressure • Drug: Hydrochlorothiazide • Most drugs in this class in in -thiazide 3 Loop Diuretics • • • • Used for hypertension Block Na/K/2Cl transporter in Loop of Henle Similar action to thiazides but better efficacy Better for severe hypertension • Drug: Furosemide 4 Osmotic Diuretics • Any osmotically active agent that is filtered by the glomerulus but not reabsorbed • These agents will prevent water reabsorption in the PCT and the descending limb of the Loop of Henle (normally these areas are freely permeable to water) • Urine is more dilute • Mannitol is used as an osmotic diuretic • Must be given IV to cause diuresis • If given PO (by mouth), will cause diarrhea • Glucose acts as an osmotic diuretic in patients with hyperglycemia 5 Diuretic: ADH Inhibitors • Drugs such as alcohol inhibit ADH release from the posterior pituitary • Decreased water reabsorption • More dilute urine 6 Diuretic: Aldosterone Receptor Blocker • Block aldosterone receptor collecting ducts • Therefore decrease sodium reabsorption • Drugs in this class also decrease the amount of potassium secreted • More dilute urine; decreased blood volume • Drug: Spironolactone 7 Renin Inhibitor • Used for hypertension • Inhibits enzyme activity of renin (prevents renin from converting angiotensinogen to angiotensin I) • Reduces angiotensin I, angiotensin II and aldosterone • Also effects ADH secretion (refer to RAAS diagram) • Drug: Aliskiren 8 Beta Receptor Blockers • Typically used to lower blood pressure • Drugs in this class block beta-adrenergic receptors of the sympathetic nervous system • Remember (from slide 69): Direct stimulation of granular cells by sympathetic nervous system causes the release of renin • Sympathetic nervous system acts on beta receptors • Drugs in this class tend to end in –olol (Propanalol, Atenolol, Pindolol) 9 10 Beta- Receptor Blockers • Propranolol • Blocks beta receptors, therefore inhibiting the stimulation for release of renin • Depresses the RAAS • • • • Less Ang II Less Na (and water) reabsorption Less Aldosterone secretion from adrenal gland Less ADH secretion from posterior pituitary • More dilute urine • Lower blood volume (and therefore lower blood pressure) • Not all beta blockers will cause this 11 12 Angiotensin-Converting Enzyme (ACE) Inhibitors • Drugs in this class inhibit ACE therefore preventing Ang I from converting to Ang II • Used to lower blood pressure • Also help stabilize renal function by decreasing proteinuria (protein in urine) • Decrease efferent arteriolar resistance therefore decreasing intraglomerular capillary pressure • Adverse effects include acute renal failure and hyperkalemia • Drugs in this class tend to end in –pril (captopril, enalapril, benzapril) 13 Angiotensin-Converting Enzyme (ACE) Inhibitors • Captopril • • • • • • Inhibits conversion of Ang I to Ang II Less Na (and water) reabsorption Less Aldosterone secretion from adrenal gland Less ADH secretion from posterior pituitary More dilute urine Decreased blood volume (and therefore blood pressure) 14 15 Angiotensin Receptor Blockers (ARBs) • Used to decrease blood pressure • Block Ang II receptors therefore preventing the actions of Ang II • • • • • Less Na (and water) reabsorption Less Aldosterone secretion from adrenal gland Less ADH secretion from posterior pituitary More dilute urine Decreased blood volume (and therefore blood pressure) • Drugs in this class tend to end in –sartan (losartan, valsartan, candesartan) 16 17 Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) • Inhibit cyclooxygenase enzymes 1 and 2 (COX1 and COX2) • COX enzymes needed to synthesize prostaglandins • Prostaglandins vasodilation • AT THE GLOMERULAR LEVEL • Inhibition of the vasodilatory effect leads to constriction of the afferent arteriole • Effect on GFR and renal perfusion pressure? _________________ • Leads to fluid retention • Decrease in urinary waste products 18 NSAIDs • Examples: • • • • • • Ibuprofen Napoxen Indomethacin Diclofenac Meloxicam Celecoxib 19 20