Vagus Nerve Lesions
advertisement

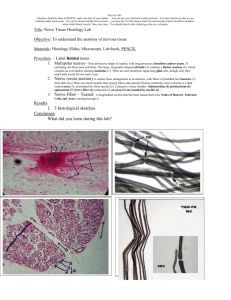
The Cranial Nerves • • • • • • • • • • • • Olfactory (I) Optic (II) Occulomotor (III) Trochlear (IV) Trigeminal (V) Abducent (VI) Facial (VII) Vestibulocochlear (VIII) Glossopharyngeal (IX) Vagus (X) Accessory (XI) Hypoglossal (XII) Glossopharyngeal Nerve • A mixed nerve (sensory, motor, parasympathetic) • Emerges from the ventral surface of the medulla oblongata • Runs laterally in the posterior cranial fossa • Leaves the skull by passing through the central part of the jugular foramen • Has superior and inferior ganglia, that are located within the jugular foramen. • At its exit from the skull, it passes forward between the internal jugular vein and internal carotid artery, within the carotid sheath • Descends to the lower border of the stylopharyngeus muscle. • Then curves forward around the stylopharyngeus and • Passes through the gap between the superior and middle constrictor muscles of the pharynx • Passes under cover of the hyoglossus muscle • Distributed to the: Palatine tonsil Mucous membrane of the fauces and base of the tongue, Mucous glands of the mouth P FPT T Functions • Receives general sensory fibers from the posterior ⅓ of the tongue, tonsil, pharynx, middle ear and carotid sinus. • Receives special sensory (taste) fibers from the posterior ⅓ of the tongue and the circumvellate papillae • Supplies parasympathetic fibres to the parotid gland via the otic ganglion • Supplies motor fibers to stylopharygeus muscle • Contributes sensory fibers to the pharyngeal plexus Branches • Tympanic branch: Passes to the tympanic plexus in the middle ear and: Supplies sensory fibers to the plexus Carries preganglionic parasympathetic fibers, that leave the plexus as lesser petrosal nerve and synapse in the otic ganglion • Carotid branch: carries sensory fibers from the carotid sinus & carotid body • Muscular branch to the stylopharyngeus muscle Branches cont’d • Lingual branch: passes to the posterior third of the tongue and the circumvellate papillae • Pharyngeal branches: carry sensory fibers to the pharyngeal plexus, which supplies the mucous membrane of the pharynx, tonsil and soft palate • Communicates with the: • Vagus & facial nerves • Superior cervical ganglion of the sympathetic chain Glossopharyngeal Nerve Lesions • Glossopharyngeal nerve lesions produce: Difficulty in swallowing Loss of general sensation over the posterior one-third of the tongue, palate, and pharynx Loss of taste sensation over the posterior one-third of the tongue and palate Dysfunction of the parotid gland Loss of the gag reflex Vagus Nerve • A mixed nerve (sensory, motor, parasympathetic) • Emerges from the ventral surface of the medulla oblongata • Runs laterally in the posterior cranial fossa • Leaves the skull by passing through the central part of the jugular foramen • Has superior and inferior ganglia, that are located within the jugular foramen • Below the inferior ganglion, it is joined by the cranial part of accessory nerve • Both right and left vagus nerves descend in the carotid sheath, lateral to the carotid artery • The right vagus nerve gives right recurrent laryngeal nerve which hooks around the right subclavian artery • Then crosses anterior to the right subclavian artery • Runs posterior to the superior vena cava • Descends posterior to the right main bronchus • Contributes to cardiac, pulmonary and esophageal plexuses • Enters the abdomen as the posterior vagal trunk through the esophageal hiatus of the diaphragm • The left vagus nerve enters the thorax between left common carotid artery and left subclavian artery • Descends on the aortic arch. • Gives rise to the left recurrent laryngeal nerve which hooks around the aortic arch • Descends posterior to the left main bronchus • Gives off thoracic cardiac branches • Contributes to cardiac, pulmonary and esophageal plexuses • Enters the abdomen as the anterior vagal trunk through the esophageal hiatus of the diaphragm. Functions • Supplies parasympathetic fibers to all the organs except the suprarenal glands, from the neck down to the proximal ⅔ of the transverse colon • Supplies motor fibers to the pharyngeal plexus that supplies the muscles of the palate, pharynx and larynx • Receives general sensation from the auricle of the ear and part of the meninges Branches • Meningeal branch • Auricular branch • Pharyngeal branch to the pharyngeal plexus. It contains nerve fibers from the cranial part of the accessory nerve • Superior laryngeal nerve divides into the: Internal laryngeal nerve: sensory to the mucous membrane of the piriform fossa and the larynx down as far as the vocal cords. External laryngeal nerve: motor, accompany the superior thyroid artery; supplies the cricothyroid muscle. • Superior & Inferior cervical cardiac branches • Recurrent laryngeal nerve: Ascends in the groove between the trachea and the esophagus closely related to the inferior thyroid artery. Mixed nerve: Sensory to mucous membrane of the larynx below the vocal cords. Motor to all the intrinsic muscles of the larynx except the cricothyroid muscles Vagus Nerve Lesions • Clinical manifestations range from mild symptoms of hoarseness of voice, loss of gag reflex and loss of effective cough mechanism, to dysphagia and choking when drinking fluids, to life-threatening airway obstruction from bilateral recurrent laryngeal nerve injury • Failure of soft palate elevation • Deviation of uvula away from the side of lesion • Abnormalities of esophageal motility, gastric acid secretion, gallbladder emptying, and heart rate; and other autonomic dysfunction. Pharyngeal Plexus • Located on the middle constrictor muscle of the pharynx • Contains: • Sensory fibers (from glossopharyngeal nerve) • Motor fibers (from cranial root of accessory nerve via vagus nerve) • Postganglionic sympathetic fibers (from superior cervical ganglion) • Supplies: • The mucous membrane of the pharynx, tonsil and soft palate • The muscles of the pharynx & larynx Accessory Nerve • A motor nerve • Has two parts: Cranial Spinal • Cranial Part: Emerges from the anterior surface of the medulla oblongata . Runs laterally in the posterior cranial fossa Joins the spinal root. • Spinal Part: • Arises from nerve cells in the ventral horn of the C1C5 segments of the spinal cord • Ascends alongside the spinal cord • Enters the skull through the foramen magnum • It then turns laterally & joins the cranial root. • The two roots unite and leave the skull through the jugular foramen • The roots then separate: The cranial root : joins the vagus nerve and is distributed in its branches (via the pharyngeal plexus) to the: muscles of the soft palate and pharynx and to the muscles of the larynx (except the cricothyroid muscle). The spinal root: runs downward and laterally and enters the deep surface of the sternocleidomastoid muscle, which it supplies, and then crosses the posterior triangle of the neck to supply the trapezius muscle Lesion of the Spinal Part • Injury to the spinal accessory nerve results in paralysis of the sternocleidomastoid and the trapezius muscles. • Patients exhibit signs of lower motor neuron disease, such as paralysis, fasciculation, and wasting of the affected muscles. • Because of its superficial position in the posterior triangle of the neck, it can be injured in penetrating wounds. The trapezius muscle gets paralyzed, and shows wasting. • Paralysis of the sternocleidomastoid muscle results in an asymmetric neckline • Paralysis of the trapezius muscle results in: Drooping of shoulder Winging of scapula Difficulty in elevating the arm above the head, having abducted it to a right angle by using the deltoid muscle. The patient is unable to shrug the shoulders. Hypoglossal Nerve • A motor nerve • Emerges from the ventral surface of the medulla oblongata • Runs laterally in the posterior cranial fossa • Leaves the skull by passing through the hypoglossal canal • Descends in the neck within the carotid sheath • Reaches lower border of digastric muscle • Curves forward by crossing the loop of lingual artery just above the tip of greater cornu of hyoid bone • Ascends deep to mylohyoid and superficial to hyoglossus muscle to reach the tongue • In the upper part of its course, it is joined by C1 fibers from the cervical plexus Functions • The hypoglossal nerve innervates: All the intrinsic muscles of the tongue All the extrinsic muscles of the tongue (except the palatoglossus, which is supplied by the pharyngeal plexus) and therefore controls the shape and movements of the tongue Branches • Meningeal branch • Descending branch: carries C1 fibers, passes downward and joins the descending cervical nerve (C2 and 3) to form the ansa cervicalis • Nerve to the thyrohyoid muscle (C1) • Nerve to the geniohyoid muscle (C1) • Muscular branches to all the muscles of the tongue except the palatoglossus Hypoglossal Nerve Lesion • If the patient is asked to protrude the tongue, it will deviate toward the paralyzed side . • As the genioglossus muscle is paralyzed on the affected side, the normal genioglossus muscle pulls the unaffected side of the tongue forward, leaving the paralyzed side of the tongue stationary. The result is the tip of the tongue deviates toward the paralyzed side. • The paralyzed muscles show wasting, and the tongue becomes wrinkled on that side.