Blood - Images
advertisement

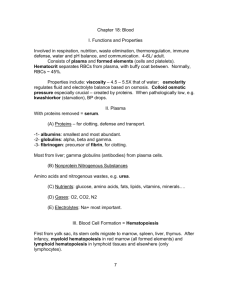
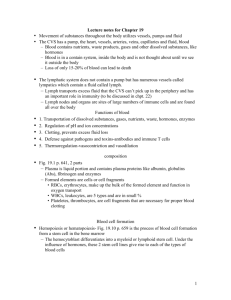
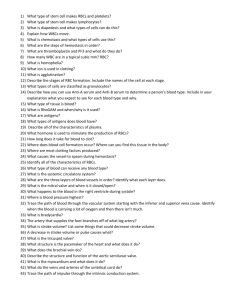
BLOOD COMPONENTS, PHYSICAL CHARACTERISTICS, AND VOLUME Blood transports everything (nutrients, wastes, and body heat) Blood is a complex fluid connective tissue with both solid and liquid components. Solid – living blood cells (formed elements) Erythrocytes (red blood cells –RBCS) Leukocytes (white blood cells –WBCS) Platelets (function in the blood-clotting process) Liquid – nonliving fluid matrix (plasma) An average blood sample (hematocrit) contains (by volume): 55% plasma 45% RBCs Less than 1% WBCs Less than 1% platelets Blood color varies from scarlet (oxygen-rich) to a dull red (oxygen-poor) Whole blood is slightly alkaline (pH 7.35 – 7.45) 8% of body weight Total adult blood volume is about 6 quarts PLASMA Straw-colored fluid 90% water Helps to distribute body heat evenly throughout the body Over 100 different solutes (plasma proteins, nutrients, respiratory gases, hormones, wastes, and products of cell metabolism) Plasma proteins are most abundant solutes Most are made by the liver Not used for cellular metabolism Composition varies continuously as cells remove or add substances to the blood Body organs make dozens of adjustments daily to maintain solutes at life-sustaining levels. FORMED ELEMENTS Erythrocytes Ferries oxygen in blood to all cells Anucleate Contain very few organelles Contains iron-containing hemoglobin (Hb) protein to transport oxygen Lack mitochondria and make ATP by anaerobic mechanisms Small biconcave cells that provide a large surface area relative to volume Outnumber WBCs by about 1000 to 1 About 5 million RBC/mm³ (as the RBC volume increases, blood viscosity increases) The more Hb a RBC contains, the more oxygen it will carry Average of 12-18 hemoglobin per 100 ml blood A single RBC contains about 250 million Hb molecules Each Hb can carry 4 molecules of oxygen So each RBC carry about 1 billion molecules of oxygen Leukocytes Far less numerous than RBCs 4,000 – 11,000 WBC/mm³ The only complete cells in blood (contain nuclei and usual organelles) Helps defend the body against damage by bacteria, viruses, parasites, and tumor cells Able to slip into and out of the blood vessels (diapedesis) to cause inflammatory or immune responses Leukopenia is an abnormally low WBC count Can locate areas of tissue damage and infection in the body Respond to certain chemicals that diffuse from the damaged cells (positive chemotaxis) Following the diffusion gradient to pinpoint areas of tissue damage Gather in large numbers to destroy foreign substances or dead cells The body speeds up their production Total WBC count above 11,000 cells/mm³is referred to as leukocytosis Indicates the presence of a bacterial or viral infection in the body Platelets Not cells in the strict sense Fragments of very large multinucleate cells called megakaryocytes that rupture Normal platelet count in blood is about 300,000/mm³ Needed for the clotting process Write a paragraph/overview of what we learned about blood. Draw a picture and thoroughly describe each of the solid/cellular components of blood (RBC, WBC and platelets) THIS IS DUE AT THE END OF THE PERIOD!!! BLOOD CELL FORMATION Occurs is red bone marrow Flat bones of the skull and pelvis, ribs, sternum, and proximal epiphysis of the humerus and femur. Each type of blood cell is produced in different numbers in response to body needs and stimuli All formed elements arise from a common type of stem cell ( hemocytoblast) in the red bone marrow Two types of descendents 1. Lymphoid stem cell – produces lymphocytes 2. Myeloid stem cell – produces all other classes of formed elements RBCs are unable to divide (anucleate) and have a limited life span of 100 to 120 days They begin to fragment and their remains are eliminated by the phagocytes in the spleen and liver Lost cells are replaced more or less continuously Developing RBCs divide many times and then begin synthesizing huge amounts of hemoglobin When hemoglobin has been accumulated, nucleus and most organelles are ejected and the cell collapses The young RBC (reticulocyte) still contains some rough ER but begins transporting oxygen Within two days they have ejected the remaining ER and have become fully functional erythrocytes The process from hemocytoblast to mature RBC takes 3 to 5 days Platelet production is accelerated by thrombopoietin Rate of erythrocyte production is controlled by a hormone called erythropoietin from liver and kidneys When blood levels of oxygen begin to decline, the kidneys increase release of erythropoietin Bone marrow is targeted and is stimulated to make more RBCs Excessive amount of oxygen in the bloodstream depresses erythropoietin release and RBC production Colony stimulating factors (a hormone) trigger formation of leukocytes and platelets and also enhance the ability of mature leukocytes to protect the body HEMOSTASIS Stoppage of blood flow is fast and localized Blood loss at the site is permanently prevented when fibrous tissue grows into the clot and seals the hole in the blood vessel. Three phases occur in rapid sequence 1. Platelet plug formation Membrane is broken so endothelium and collagen fibers are exposed to oxygen Platelets become “sticky” and cling to the damaged site Platelets release chemicals that attract more platelets Platelet plug is formed 2. Vascular spasms Platelets release serotonin that causes the blood vessel to go into spasms Blood loss decreases until clotting can occur 3. Coagulation Injured tissues release thromboplastin (helps the clotting process) A platelet phospholipid interacts with thromboplastin and Ca⁺ to form a prothrombin activator The activator converts prothrombin in the plasma into the enzyme thrombin Thrombin joins soluble fibrinogen proteins into long hair-like molecules of insoluble webbing Coagulation continued Forms a meshwork that traps the RBCs and forms the basis of the clot Within the hour, the clot begins to retract, squeezing serum (plasma minus the clotting proteins) from the mass and pulling the ruptured edges of the blood vessel closer together Normally, blood clots within 3 to 6 minutes Once the clotting cascade has started, triggering factors are rapidly inactivated to prevent widespread clotting Eventually the endothelium regenerates and the clot is broken down Create a comic strip of hemostasis including pictures and thoroughly descriptive captions. DISORDERS OF HEMOSTASIS Undesirable Clotting Usually occurs in the legs Clot that develops and persists in an unbroken blood vessel is a thrombosis May prevent blood flow if large enough A thrombosis that breaks away from the vessel wall and floats freely in the bloodstream is an embolus Usually no problem unless/until it lodges in a blood vessel Caused by anything that roughens the blood vessel endothelium and encourages clinging of platelets Slowly flowing blood or blood pooling is another risk factor (especially in immobilized patients) Bleeding disorders Common causes are platelet deficiency, deficits of clotting factors and genetic conditions Thrombocytopenia results from an insufficient number of circulating platelets Normal movement causes spontaneous bleeding from small blood vessels (petechia) Hemophilia is a hereditary bleeding disorder Lack of the factors needed for clotting Minor tissue trauma results in prolonged bleeding and can be life-threatening HUMAN BLOOD GROUPS Plasma membranes of RBCs have genetically determined proteins (antigens) Each of us tolerates our own cellular (self) antigens RBC proteins will be recognized as foreign if transfused into another person with different RBC antigens Antibodies present in the plasma attach to “foreign” RBCs causing RBCs to clump (agglutination) This leads to the clogging of small blood vessels throughout the body Foreign RBCs are lysed and Hb is unable to deliver oxygen Clogged vessels affect kidney tubules to cause kidney failure, fever, chills, nausea, and vomiting may occur. Over 30 common RBC antigens ABO blood groups are based on which of the two antigens (type A or B) a person inherits Absence of both antigens results in blood type O Presence of both antigens results in blood type AB Possession of either A or B antigen yields type A or B blood, respectively Rh blood groups are based on agglutinogen D (originally identified in Rhesus monkeys) Most Americans are Rh⁺ (RBCs carry the Rh antigen) If an Rh⁺ person receives Rh⁺ blood their immune system begins producing anti- Rh⁺ antibodies Hemolysis does not occur with the first transfusion It takes time for the body to react and start making antibodies In subsequent transfusions, a typical reaction occurs (patient’s antibodies attack/rupture donor RBCs) First time pregnant Rh⁺ women who carry Rh⁺ babies usually results in the delivery of a healthy baby Mother is sensitized by Rh⁺ antigens and forms antiRh⁺ antibodies If she becomes pregnant again with an Rh⁺ baby, her antibodies will cross the placenta and destroy the baby’s RBCs DEVELOPMENTAL ASPECTS OF BLOOD Embryonic development of the entire circulatory system occurs within 28 days Embryonic blood cells are circulating in the newly formed blood vessels around day 28 Fetal Hb has a greater ability to pick up oxygen (fetal blood is less oxygen-rich than that of the mother) Fetal blood cells are gradually replaced by RBCs that contain the more typical Hb Fetal RBCs are destroyed and the products are released in the bile If this happens at a rate faster that the immature liver can handle, the infant becomes jaundiced Write a journal entry as if you are a person suffering from a hemostatic disorder. You must explain your disorder and how you feel about having that disorder. You may also portray a doctor explain what to expect while telling a patient that they have that disorder, are pregnant with a child who has the disorder. This is due at the end of the period!