Mechanical Ventilation in the ICU: What You Need to Know
advertisement

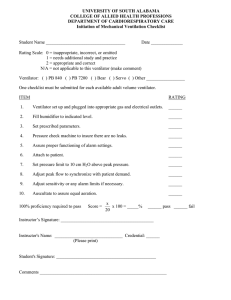
Mechanical Ventilation in the ICU: What You Need to Know Behrouz Jafari, M.D Pulmonary/Critical Care and Sleep Medicine UCI-VA Long Beach Mechanical Ventilation NIPPV When to intubate Setting the ventilator Complications of mechanical ventilation Weaning Case Study 65-year-old with COPD exacerbation using accessory muscles and wheezing after 2 bronchodilator treatments HR 110/min, BP 160/110 mm Hg, RR 30/min, T 99F ABG on 3 L/min O2: pH 7.24, PCO2 60 mm Hg, PO2 65 mm Hg What type of respiratory support should be initiated? NIPPV NPPV: Evidence-Based Recommendations: ● ● Recommended (1A) • » Severe COPD exacerbation (pH < 7.35) • » Cardiogenic pulmonary edema – No shock or ACS requiring revascularization Suggested (2B-‐2C) • » Immunocompromised hypoxemic RF (2C) • » Post-‐op respiratory failure (2C) – abdominal, lung resection • » Facilitation of extubation in high-‐risk or COPD • Keenan et al. Can Med Assoc J 2011 NIPPV Contraindications Poor Mental Status Excess Secretions Severe Respiratory Failure Shock Inability to Protect Airway Case Study ABG on 3L/min O2: pH 7.24, PaCO2 60 mm Hg, PaO2 65 mm Hg HR 110/min, BP 160/110 mm Hg, RR 30/min How should the patient be monitored? NPPV: Monitoring Patient Mask comfort Tolerance Resp distress RR, VS » Accessory muscle use » Abdominal paradox ● ● Ventilator Air leak Adequacy of IPAP (Vt), EPAP Pt-‐vent synchrony SpO2; ABG (2 hr) Setting » ICU to start »SDU if stable Case Study After 1 hr of NPPV, the patient has not improved Arterial blood gas on 40% O2: pH 7.20, PaCO2 65 mm Hg, PaO2 58 mm Hg HR 120/min, BP 142/98 mm Hg, RR 40 /min What is the next step? What predicts success or failure? NPPV: Predictors of Failure ● COPD » pH < 7.25 » RR > 35/min » Severely ill » Asynchrony » GCS < 11 » Poor tolerance Hill et al. Crit Care Med 2007;35:2402-7 ● Hypoxemic Resp Fail » ALI/ARDS » Severely ill » Metabolic acidosis » P/F < 150 after1hof NPPV » Pneumonia » Shock NPPV: Predictors of Failure ● COPD » pH < 7.25 » RR > 35/min » Severely ill » Asynchrony » GCS < 11 » Poor tolerance Hill et al. Crit Care Med 2007;35:2402-7 ● Hypoxemic Resp Fail » ALI/ARDS » Severely ill » Metabolic acidosis » P/F < 150 after1hof NPPV » Pneumonia » Shock Case Study Orotracheal intubation is performed What ventilator mode should be selected? What tidal volume is optimum? What rate of ventilation should be set? Invasive Mechanical Ventilation Breath Characteristics Airway Pressure (cm H2O) Trigger, Target, Cycle Respiratory Cycle Cycling Inspiration Triggering Time (sec) Expiration Breath characteristics Trigger •Controlled - machine timer •Assisted/supported - patient effort –Pressure trigger: Pt effort pressure drop in vent circuit vent response –Flow trigger – pt effort draws gas out of a continuous flow through the vent circuit vent response Breath characteristics Gas Delivery (Target) Breath characteristics Cycle (turning breath off) •Three common types –reach set volume –reach set time –reach certain flow reduction 5 Basic Breath 5 Basic Breath 5 Basic Breath 5 Basic Breath Modes of Support Synchronized intermittent mandatory ventilation Spontaneous SIMV + PSV Volume-cycled breath Setting the Ventilator Mode FiO2 Rate Tidal Volume PEEP Initiation of Mechanical Ventilation Initial Ventilator Settings Minute Ventilation Metabolic rate is directly related to body surface area (BSA) Males: = 4 x BSA Females: = 3.5 x BSA Nomogram Initiation of Mechanical Ventilation Initial Ventilator Settings Minute Ventilation based on BSA Example: Female patient with an estimated BSA of 2.0 m2 = 3.5 x 2.0 m2 = 7.0 L/min A patient’s requirements increase by 9% for every 1° C increase on body temperature Initiation of Mechanical Ventilation Initial Ventilator Settings Minute vent.= RR TV Tidal Volume VT for an adult is 6 – 8 ml/kg of IBW Ideal Body Weight Calculation Male IBW in lb: Female IBW in lb: 106 + [6 x (height in inches – 60)] 105 + [5 x (height in inches – 60)] Oxygen Supplementation Start with 100% after intubation FiO2 > 60% is (probably) toxic. Need to balance potential toxicities Oxygen PEEP Case Study What monitoring and assessment is needed after initiation of mechanical ventilation? Chest radiograph Vital signs SpO2 Patient-ventilator synchrony ABG Inspiratory pressures Auto-PEEP Ventilator alarms Proving Endotracheal Intubation Soft Signs Equal breath sounds Easy ventilation No stomach bubbles Adequate oxygenation Firm Signs Radiograph Expired CO2 Inspiratory Pressures Peak inspiratory pressure (Ppeak) Inspiratory plateau pressure (Pplat) Indicator of alveolar distension Compliance and Resistance High Peak/High Plateau = decreased compliance pneumonia, CHF, Pleural Effusion, Pneumothorax, ARDS, ascites, Chest wall abnormalities High Peak/Low Plateau = increased resistance secretions, bronchospasm, tubing abnormalities Case Study 18-year-old female found unresponsive at a party (wt 60 kg, ht 64 inches [162.6 cm]) Vomitus in pharynx, difficult intubation SpO2 87-88% on 100% oxygen Case Study Mode FiO2 Tidal volume Rate PEEP Assist control (volume) 1.0 550 mL 10 breaths/min 5 cm H2O Ideal body wt = 56 kg ® Case Study Mode FiO2 Tidal volume Rate PEEP Assist control (volume) 1.0 550 mL 10 breaths/min 5 cm H2O Ideal body wt = 56 kg High pressure alarm sounding ® Case Study What problems are present? SpO2 88% (FiO2 1.0) Blood gas: pH 7.38, PaCO2 36 mm Hg, PaO2 57 mm Hg Ppeak 52 cm H2O Pplat 48 cm H2O Auto-PEEP 0 cm H2O Patient’s RR 18/min ® Waveform showing decreased lung compliance ‘Square wave’ flow pattern Ppeak Pplat Pres Case Study What changes in ventilator settings would decrease inspiratory plateau pressure? Current Ventilator Settings Assist control (volume) FiO2 1.0 Tidal volume 550 mL RR 10/min PEEP 5 cm H2O ® Case Study What changes in ventilator settings would improve oxygenation? Current Ventilator Settings Assist control (volume) FiO2 1.0 Tidal volume 550 mL Respiratory rate 10 breaths/min PEEP 5 cm H2O ® NIH ARDS Network trial NEJM 2000;342:1301 Case Study 70-year-old with long smoking history failed NPPV for respiratory distress Intubated, sedated, and receiving mechanical ventilation Wt 75 kg, ht 69 inches [175.3 cm]) IBW 70 Kg Case Study Mode FiO2 Tidal volume Rate PEEP AC 1.0 700 mL 12 breath/min 5 cm H2O Case Study What are the major problems? Blood gas: pH 7.20, PaCO2 60 mm Hg, PaO2 215 mm Hg Pplat 28 cm H2O, Ppeak 50 cm H2O Auto-PEEP 8 cm H2O I:E = 1:1.5 RR 18/min BP 70/30 mm Hg, HR 130/min Low blood pressure alarm sounding What do you do next? ® Case Study What are possible causes of the patient’s hypotension? Positive intrathoracic pressure (venous return ) Auto-PEEP Hypovolemia Tension pneumothorax Myocardial ischemia ® Auto-PEEP Diagnosis Measurement Waveform analysis Gas flow Auto-PEEP Auto-PEEP Waveform showing increased airways resistance Ppeak Pplat Pres Recognizing prolonged expiration (air trapping) Recognize airway obstruction when Expiratory flow quickly tapers off and then enters a prolonged low-flow state without returning to baseline (auto- PEEP) This is classic for the flow limitation and decreased lung elastance characteristic of COPD or status asthmaticus Auto-PEEP Consequences Inspiratory pressures Hypotension Worsened oxygenation Interventions to decrease auto-PEEP Respiratory rate Tidal volume Gas flow rate ® Case Study What immediate changes in ventilator settings should be made? Current Ventilator Settings AC FiO2 1.0 Tidal volume 700 mL Respiratory rate 12 breaths/min PEEP 5 cm H2O ® Obstructive Airway Disease Initial tidal volume 6-8 mL/kg Optimize expiratory time Beware of auto-PEEP Adjust minute ventilation to low normal pH Treat obstruction with bronchodilators Mental Status, Sputum Volume & Cough Strength in Weaning ● 3 Risk factors for failure » Poor cough » Heavy endotracheal secretions » Unable to do all 4 tasks (open eyes, follow with eyes, grasp hand, stick out tongue) ● If 2/3 present, 71% sensitive, 81% specific for failure (72h) Salam et al. Intensive Care Med 2004; 30:1334-9 Spontaneous Breathing Trial ● Test of breathing for 30 min with minimal ventilatory support ● Variables in SBT » Ventilatory support: T-tube or “flow-by”, < 5 cm H2O CPAP, PSV, or automatic tube compensation » Termination criteria: RR > 35 bpm x > 5 min, SaO2 < 90%, HR > 140 bpm or sustained HR change > 20% SBP > 180 or < 90 mmHg, increased anxiety or diaphoresis Ventilator Emergency I A 55-year-old patient with ARDS suddenly has a dramatic rise in airway pressures and loss of VT and is starting to desaturate quickly. What is the differential diagnosis? Sudden worsening of lung disease Pneumothorax Atelectasis Airway obstruction Ventilator Emergency II A 69-year-old schizophrenic woman with aspiration pneumonia starts to become agitated and starts yelling at you (even though she is intubated). Low VT alarms go off. What is the differential diagnosis? Ventilator Emergency II A 69-year-old schizophrenic woman with aspiration pneumonia starts to become agitated and starts yelling at you (even though she is intubated). Low VT alarms go off. What is the differential diagnosis? Self-extubation Cuff leak Ventilator Emergency III A 23-year-old female asthmatic is being ventilated with PCV. The blood gas is 7.14/75/102 on: AC12/PCV20/TI0.5/FiO235%/PEEP 0. The RR is increased to 20, the VT’s drop, the PCO2 rises, and the patient becomes hypotensive. What is the differential dx? Progressive air trapping Tension pneumothorax What to Report on Rounds Ventilator Settings Minute Ventilation (VE) Pressures Peak Plateau Mechanics Compliance Resistance Auto-PEEP Key Points Goals of NPPV /MV: NPPV is best used in: support of oxygenation and ventilation and reduction in work of breathing Alert, cooperative patient whose condition will improve in 48-72 hours Use guidelines when initiating MV and adjust based on monitoring Maintain low TV 6-8 ml/kg IBW and Pplat 30 cm H2O. Primary determinants of oxygenation: FiO2 and mean airway pressure. Daily evaluation for possible weaning