1. Staphylococcal inf.
advertisement

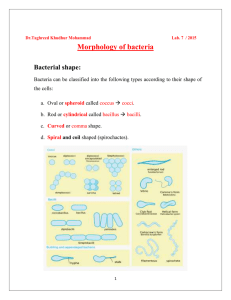
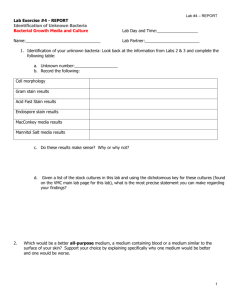
Lesson 3 WT Staphylococcal infections • Diagnosis of staphylococcal infections • Diagnostical model: abscess - pus, enterotoxicosis - food, osteomyelitis punctate, secretions, • Microscopy, cultivation, biochemical tests, detection of enzym,ATB susceptibility tests Diagnosis of staphylococcal infections • Microscopy – from the base of abscess., in aspirations and punctates – usually few bacteria and more PMNL, blood for hemocultivation – as few as 1 cell/1 ml, in rest of food in enterotoxicosis – not sufficient for prooving • Cultivation - blood agar, salt mannit, pigment, hemolysis • Identification – biochemical • Detection of plasmacoagulase, toxins, enzymes, phagotypes, analysis of nucleoacids • Serology – seldome, antibodies against teichooic acid imunodiffusion – detection of prolonged infection - bacteremia, endocarditis • Abscess - pus - sterile collection • enterotoxicosis – rest of food – detection of toxin, presence of staphylococcus is not the proof • osteomyelitis - punktate, discharge - sterile collection, blood for hemocultivation Microscopy • Broth cuture of Staphylococcus aureus fixed and stained by Gram: G+ cocci in clusters Cultivation of Staphylococci • Blood agar: Staphylococcus aureus - grey to yellow pigmented colonies, concave, buttered, beta hemolysis • Stafylococcus epidermidis - white colonies, without hemolysis • Growth on media with NaCl a indicator – salt manit - only St.aureus – changing color of indicator from red to yellow Demonstration G+cocci: Staphylococcus aureus a Staphylococcus epidermidis on the selective-diagnostic medium Salt mannit: selectively NaCl allowed growing of staphylococci that tolerate it.while others do not., mannitol is the diagnostic substrate utilised by St. aureus which metabolised it, formed acid that makes the medium becomming acid and change the pH and indicator color. St. aureus changes the original red color to yellow, St. epidermidis is growing on the mediu , tolerates salt without changing the pH and indicator color not utilising manitl ATB susceptibility testing • Disc diffusion method • 6-8 ATB discs in one plate • Zone of inhibitionof the growth in mms – comparison with standards Without zone of inhibition – resistence to tested ATB Zone of inhibition of growth sufficiently large ATB disc Growth of tested bacteria Insufficient zone of inhibition ATB susceptibility Staphylococcus aureus - PNC - penicilinase, semisyntetic PNC: oxacilin, methicilin - resistence MRSA – hospital strains and CoMRSA • - alteration on the level of target structure - pencilin binding protein PBP • – chromosomal type typ – connected with resistence to other atb - clindamycin, erytromycin, aminoglycosides Good susecptibility to vancomycine – transmissible resistance form Enterococcus Comparison od atb susceptibility • Streptococcus pyogenes – HSA / Staphyolococcus aureus PNC, TET • Staphylococcus aureus / Staphylococcus epidermidis, Staphylococcus haemolyticus OXA, CEF, Detection of plasmacoagulase summer term • Free • Bound • Slide • Tube method • Staphylococcus epidermidis • Staphylococcus aureus Free coagulase • Tube method – colony of tested strain is emulsified in 0,5 ml of plasma. Incubated for 6 h.at 37*C then at room temperature for 24 hrs. • Reading after 1 hour, 2 hrs and 24 hrs. • method – watching of coagulum. Formation of coagulum = pozit., • Because of possible presence of fibrinogen in plasma this can dissolve the coagulum. That is why we read it at 1,2 and 24 hrs. Fig. Bound coagulase • Slide method • In 2 drops of steril water or saline solution there is the suspension prepared from tested strain. 1 drop of plasma is added. Reading after 1015´sec. Odčítava sa o 10-15 sec. • White precipitate, agglutination = posit. • Negative result must be confirmed by tube test • Fig. Detection of catalase and oxidase activity Catalase: - enzyme, hydrolysing H2O2 – toxic for the cell and formation of molecular oxygen. Moraxella catarrhalis –cat.negat. H2O2 hydrolysis, bubbles - Staphylococcus sp.