Reabsorption of Na + and Water Along Different Parts of the Nephron
advertisement

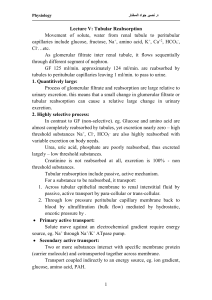
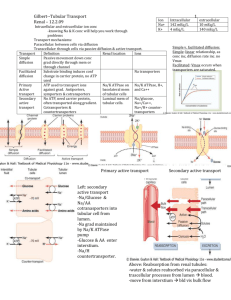
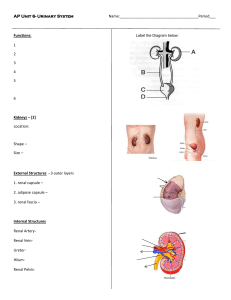
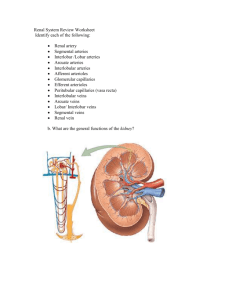
HUMAN RENAL SYSTEM PHYSIOLOGY Lecture 5,6 BY: LECT. DR. ZAINAB AL - AMILY Renal artery stenosis • Glomerular capillary blood pressure is determined in part by the aortic pressure and by the preglomerular vascular resistance. • The preglomerular vascular resistance is predominantly at the afferent arteriole. • A stenosis in the renal artery introduces a preglomerular vascular resistance and decreases glomerular capillary pressure. • The decrease in glomerular capillary pressure results in the fall in glomerular filtration rate and the shift toward retention of sodium and water. • Retention of water and sodium causes an increase in systemic arterial blood pressure; and as soon as the blood pressure is sufficiently high, glomerular capillary pressure returns to normal. • Renal artery constriction also limits blood flow to the kidney and can result in a failure of the kidney to grow and develop normally in children. • Adults with significant renal artery stenosis often exhibit an asymmetric or smaller than normal kidney. • Hypertension caused by renal artery stenosis is often refractory to treatment. • This is because the underlying defect persists and any successful treatment of systemic hypertension results in a lower renal perfusion (glomerular capillary) pressure and shifts the renal fluid balance into retention of sodium and water. Glomerular Disorders Glomerulo-nephritis:- Inflammation of the glomerulus Immunologic abnormalities (most common) Drugs or toxins Vascular disorders Systemic diseases Viral causes It is the most common cause of end-stage renal failure Glomerulonephritis Glomerular Disorders • Glomerular diseases causes:1. Glomerular membrane surface area. 2. Glomerular capillary blood flow. 3. Blood hydrostatic pressure. 5. Negative ionic charge barrier. 4. Glomerular capillary permeability. So Hematurea + Loss of Plasma Pr. In urine hypoalbuminemia Leakage of plasma fluid into the interstitial spaces Edema Glomerular diseases Two categories Nephritic syndrome Nephrotic syndrome:group of diseases Membr. glomerulonephritis All the different types Focal glomerulosclerosis inflammation & injury Minimal change disease - Proteinuria – Oliguria Loss of > 3.5 g/day of - Hematuria - Hypertension protein in urine - Pyuria - Azotemia. Hypoalbuminemia, edema - Edema hyperlipidemia, & lipiduria Pathophysiology of Nephrotic syndrome Minimal change disease Normal glumerular structure Tubular Processing of the Glomerular Filtrate: A. Tubular Reabsorption: • Unlike glomerular filtration, tubular reabsorption is more selective: i. Some substances such as glucose and AA are almost completely reabsorbed from the tubules. ii.Many ions in the plasma like Na+, Cl¯ and HCO3¯ are also highly reabsorbed (variable reabsorption rate) iii.Certain waste products such as urea and creatinine, however, are poorly reabsorbed and excreted in relatively large amounts. –Therefore, the kidneys regulate the excretion of solutes independently for the precise control of body fluid composition. • For a substance to be reabsorbed, it must first be transported across the tubular epithelial membranes into the renal interstitial fluid (ISF), and thence, the peritubular capillaries. • Reabsorption across the tubular epithelium includes active or passive transport mechanisms. • Water or solutes can be transported either through cell membranes(transcellular transport) or through junctional spaces between the cells (paracellular transport), • Then, to the peritubular capillary by (ultrafiltration or bulk flow), mediated by hydrostatic and colloid osmotic forces. Tubular Processing of the Glomerular Filtrate: A. 1. Active Transport: • is the movement of solutes against the electrochemical gradient, which requires energy that is derived from metabolism. i. Primary Active Transport: •It is coupled directly to an energy source such as the hydrolysis of ATP by way of membrane-bound ATPase pump. • A good example is the (Na+–K+ ATPase) pump that functions through most parts of the renal tubules. Other examples include the (H+–K+ ATPase) pump. • ii- Secondary Active Transport: •Two or more substances interact with a specific membrane protein (a carrier molecule) and are cotransported together across the membrane. •An example is the secondary active transport of glucose and AA in the proximal tubule. • Glucose moves from tubular fluid into the cell on the Na+-glucose cotransporter (called SGLT) in the luminal membrane. • Two Na ions and one glucose bind to the cotransport protein, Na and glucose are released into the ICF. • In this step, glucose is transported against an electrochemical gradient; the energy for this uphill transport of glucose comes from the downhill movement of Na • So secondary active transport of glucose occurs at the luminal membrane, while passive (facilitated) diffusion occurs at the basolateral membrane • The proteins involved in facilitated diffusion of glucose are Called GLUT 1 and GLUT 2 and passive uptake by bulk flow at the peritubular capillaries. Tubular Processing of the Glomerular Filtrate (continues): A. 1. Active Transport: • Transport Maximum: • For most substances that are actively reabsorbed or secreted, there is a limit, referred to as “transport maximum Tm” • due to saturation of the specific transport systems that are involved, when the tubular load of that substance exceeds the capacity of the carrier protein or the specific enzymes involved. • A good example is the glucose transport system. Under normal conditions, glucose is transported at a rate of approximately (100 mg/ minute), called the filtered load of glucose • What is filtered load? • is the amount of substance that filters through the glomerular membrane into tubules each minute. Filtered load of glucose = GFR × Pglucose • Where Pglucose=(80 mg/100mL), and hence, filtered load of glucose = 100 mg/ minute. • Essentially, all of the glucose is reabsorbed and not more than a few mgs appear in urine/day. • The amount reabsorbed is proportionate to the amount filtered and, hence, to (Pglucose) × GFR) up to the transport maximum for glucose (TmG); beyond which, the amount rises in urine • The (TmG) is about (375 mg/ minute) in men and (300 mg/ minute) in women. • What is renal threshold for a substance? • Every substance that has a transport maximum also has a specific (threshold) concentration in the plasma below which none of it appears in the urine and above which progressively larger quantities appear in urine. • This concentration is called renal threshold, e.g. renal threshold for glucose is 180 mg/100 ml. • What are non-threshold substances? • Substances which are excreted in urine at any concentration in plasma are called non threshold substances. They do not possess threshold level in plasma, e.g. urea, uric acid, sodium (in proximal tubules). • A 63-year-old hospitalized woman becomes oliguric and confused. A blood sample is drawn to measure her glucose concentration, which is found to be 35 mg/dL. • An IV access is obtained and an ampule of 50% dextrose is given followed by a continuous infusion of 10% dextrose. Most of the glucose that is filtered through the glomerulus undergoes reabsorption in which of the following areas of the nephron? • a. Proximal tubule • b. Descending limb of the loop of Henle • c. Ascending limb of the loop of Henle • d. Distal tubule • e. Collecting duct Tubular Processing of the Glomerular Filtrate: A. 2. Passive Transport (reabsorption): • Substances that are passively reabsorbed do not demonstrate a (Tm), because rate of transport is determined by two main factors: i. An electrochemical gradient for diffusion from the tubular lumen towards the peritubular capillaries. ii. Tubular cell membrane is permeable to this substance. iii.Time that the fluid containing the substance remains within the tubule. Transport of this type is referred to (gradient-time transport), which in turn depends on the tubular flow rate. – An example of passively reabsorbed substances is the passive reabsorption of urea, chloride and water: • Movement of solutes out of the tubule creates an osmotic gradient that favors water movement in the same direction. Only, if the membrane is permeable to water. • For chloride ions, the active reabsorption of Na+ is closely coupled to the passive reabsorption of Cl- through the paracellular pathways by way of an electrochemical gradient. • Finally, urea is also passively reabsorbed from the tubules down a concentration gradient caused by water reabsorption from the lumen. • Urea does not permeate the tubule as water, and therefore, about half the filtered urea passes into urine. • B.Tubular Secretion: an active or passive process. ex. (PAH). Tubular secretary processes involve the transport of substances into the tubular lumen from the tubular cells themselves, or through the tubular cells from the peritubular capillaries. The amount of a substance that is secreted in urine is calculated as the amount excreted of that substance minus the amount that is filtered. In case of active secretion, there is also a limited capacity for the tubular secretion of different substances caused by saturation of the transport systems. • The substances which are secreted by renal tubules. • Potassium ions are secreted in the distal tubule and collecting ducts. Potassium and hydrogen are both exchanged for sodium which is reabsorbed. Potassium secretion is modified by plasma level of aldosterone. • Hydrogen ions are secreted throughout the renal tubule but most significantly in the distal tubule. • Certain foreign substances and drugs are secreted. Paraaminohippuric acid (PAHA-foreign substance) is secreted actively by proximal tubular cells. • penicillin is also similarly secreted. • Tubular secretion of foreign substances is important in clearing of the plasma of a substance in one passage through the kidney. • Tubular secretion of drugs plays important role in maintaining the blood level of the drug and hence the therapeutic efficiency. Reabsorption of Na+ and Water Along Different Parts of the Nephron : • The amount of Na+ in the food is variable, but kidneys can change their excretion rate in spite of the great variation of Na+ intake. Na+ is freely filtered at the glomerulus , around 99.4% of the filtered Na+ is reabsorbed. 1) In the Proximal Convoluted Tubule: • Na+ reabsorption is an active process, produced by the activity of (Na+–K+ ATPase) pump in the basolateral membrane of the tubular cells. • In the first half of the proximal tubule, Na+ is reabsorbed by co-transport along with glucose, aminoacids, organic acids and other solutes. • The second method by which (Na+) is reabsorbed by the renal tubules is in exchange with the secreted (H+) ions. • Depending on Pco2, CO2 in the tubular cells react with H2O to form carbonic acid (H2CO3) under influence of carbonic anhydrase enzyme, H2CO3 dissociates into (H+) and (HCO3-) and (H+) is secreted in exchange with Na+ which is an example of a secondary active transport. • The energy liberated from the downhill movement of Na+ ions into the interior of the cell, enables the uphill movement in the opposite direction of H+ ions outward • There is a passive reabsorption of Cl¯ ions. • The accumulation of these substances (Na+, Cl¯ and HCO3¯) will increase the osmotic pressure in the ISF, causing the passive reabsorption of water into it • Na+, water and other substances are reabsorbed from the ISF into the peritubular capillaries by ultrafiltration (a passive process that is driven by the hydrostatic and colloid osmotic pressure gradient). • At the end of the proximal convoluted tubules, 60 – 70% of the filtered solutes and water have been removed. • What is glomerulotubular balance in proximal tubule? • Under normal condition, almost a constant percentage of sodium and fluid (about 65%) is reabsorbed while the filtrate is passing through proximal tubule regardless of the rate of glomerular filtration. • This is called glomerulotubular balance, e.g. when GFR is 100 ml/min, tubular reabsorption is 65 ml/min. If GFR increases to 200 ml/min, tubular reabsorption also increases to 130 ml/min, thus maintaining proportional balance (65%). • What is the importance of glomerulotubular balance? • Glomerulotubular balance prevents overloading of more distal tubular segments when the GFR increases. • Glomerulotubular balance therefore acts as a second line of defense to buffer the effects of spontaneous increase in GFR on urine output. • How much is the normal rate of reabsorption in renal tubules? • Normal rate of reabsorption in peritubular capillaries is 124 ml/min. GFR, i.e. amount of filtrate entering the tubule is 125 ml/min. Volume of urine formed is therefore approximately 1 ml/min. Reabsorption of Na+ and Water Along Different Parts of the Nephron : 2) In the Loop of Henle: • The descending limb and the thin segment of the ascending limb of the loop of Henle are permeable to water; • while, the thick ascending segment of Henle’s loop is impermeable to water, but permits the co-transport of (Na+, K+ and Cl¯) out of the tubular lumen. • Therefore, the fluid in the descending limb becomes hypertonic to plasma, as water moves to the hypertonic interstitium. • On the other hand, it becomes hypotonic to plasma in the ascending limb due to the movement of solutes out of the tubular lumen. • Here, another 15% of the filtered water is reabsorbed. Reabsorption of Na+ and Water Along Different Parts of the Nephron : 2) In the Loop of Henle: • The transport mechanism in the thick ascending limb depends on a carrier that transports the three ions from the tubular lumen into the tubular cells. • (Na+- K+ ATPase pump) at the basolateral membrane of the tubular cells has the important role, where it maintains a favorable gradient for the movement of Na+ from the tubular lumen into the cell. • This portion of the renal tubule has a higher Na+- K+ ATPase content than any other part. • The K+ diffuses passively back into the tubular lumen. • One Cl¯ ion diffuses passively into the ISF, and one is cotransported with K+ ion. • A 65-year-old male with a past medical history of COPD, hypertension, diabetes mellitus type II, and hypercholesterolemia presents to the emergency department with swelling of the legs and feet and shortness of breath. After complete history, physical exam, and appropriate diagnostic testing, it is determined that the patient is experiencing volume overload as a result of an acute exacerbation of congestive heart failure. The patient is started on oxygen therapy, nebulizer treatments, and intravenous furosemide, which inhibits sodium reabsorption in the thick ascending limb of the loop of Henle via which of the following mechanisms? • a. Na+ Cl− cotransport • b. Na+/H+ exchange • c. Na+/K+ exchange • d. Na+ − K+ − 2Cl− cotransport • e. Na+/nutrient cotransport Reabsorption of Na+ and Water Along Different Parts of the Nephron : 3) In the Distal Convoluted Tubule and the Cortical Collecting Duct: • The first part is in effect an extension of the thick segment of the ascending limb with the same reabsorptive characteristics. • The second part of the distal tubule and the subsequent cortical collecting duct have similar functional characteristics. They are composed of two distinct cell types: -The principal (P) cells. - The intercalated (I) cells. • P cells reabsorb Na+ and water from the tubular lumen, and secrete K+ into the lumen, depending again on the activity of the Na+- K+ ATPase pump in each cell. •Here, Na+ reabsorption and K+ secretion is under the influence of aldosterone hormone, that is secreted from the adrenal cortex. •It increases the number of special active Na+ channels in the apical (luminal) membrane of the P cells. •It increases the Na+- K+ ATPase pump; •thereby, Na+ and water reabsorption and K+ secretion are regulated according to the body requirements. Reabsorption of Na+ and Water Along Different Parts of the Nephron : 3) In the Distal Convoluted Tubule and the Cortical Collecting Duct: • The I cells avidly secrete H+ ions and reabsorb HCO3¯ and K+ ions. Here, most H+ ions are secreted by an ATP- driven proton pump (H+ ATPase). • Aldosterone hormone acts also on this pump to increase the distal H+ secretion. These I cells play a key role in acid – base regulation. • Moreover, this segment is also under the control of antidiuretic hormone (vasopressin, ADH), which increases the permeability of the renal tubules to water. • About 5% of the filtered water is removed in this segment. Reabsorption of Na+ and Water Along Different Parts of the Nephron : 4) In the Medullary Collecting Duct: • In this portion of the collecting duct, water permeability is again controlled by the levels of vasopressin hormone from the posterior pituitary gland; which increases water permeability of the membranes of the collecting ducts by causing rapid insertion of (aquaporin- 2) water channels into the luminal membrane of the P cells. • In the presence of enough vasopressin to produce maximal antidiuresis, as much as 14.7% of the filtered water is removed from the collecting ducts. • This produces concentrated urine, with a total of 99.7% of the filtered water being reabsorbed. • On the other hand, in the absence of ADH, only about 2% of the filtered water is reabsorbed along with the salt that is pumped out of the collecting duct. • A 57-year-old woman with chronic cardiac failure presented at the University Medical Center to participate in a clinical research study on the genetics of heart failure. Genetic analysis showed an increase in ADH gene expression and associated hypothalamic biosynthesis of the hormone, in addition to increased release of the hormone from the posterior pituitary. In the presence of ADH, the filtrate will be isotonic to plasma in which part of the kidney? • a. Ascending limb of the loop of Henle • b. Descending limb of the loop of Henle • c. Cortical collecting tubule • d. Medullary collecting tubule • e. Renal pelvis At which nephron site does the amount of K+ in tubular fluid exceed the amount of filtered K+ in a person on a high-K+ diet? (A) Site A (B) Site B (C) Site C (D) Site D (E) Site E