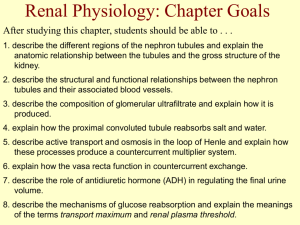
AHS renal lecture 1 V Campbell [Read
advertisement

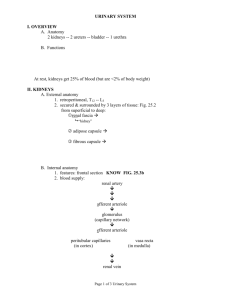
Renal System Professor Veronica Campbell vacmpbll@tcd.ie Lecture 1: The renal system Components of renal system Structure of nephron Basic renal functions Filtration - Autoregulation Tubuloglomerular feedback Reabsorption Secretion 1 Functions of kidney – Maintain H2O and salt balance in the body – Maintain proper osmolarity of body fluids, primarily through regulating H2O balance – Regulate the quantity and concentration of most ECF ions – Maintain proper plasma volume – Help maintain proper acid-base balance in the body – Excreting (eliminating) the end products (wastes) of bodily metabolism and drug metabolites – Producing erythropoietin (rbc formation) – Producing renin – Converting vitamin D into its active form 2 – Urine forming organs • Kidneys – Structures that carry urine from the kidneys to the outside for elimination from the body • Ureters • Urinary bladder • Urethra Ureters • Smooth muscle-walled duct • Exits each kidney at the medial border in close proximity to renal artery and vein • Carry urine to the urinary bladder 3 Urinary Bladder • Temporarily stores urine • Hollow, distensible, smooth muscle lining wall • Periodically empties to the outside of the body through the urethra Urethra • Conveys urine to the outside of the body • Urethra is straight and short in females • In males – Much longer and follows curving course from bladder to outside – Dual function • Provides route for eliminating urine from bladder • Passageway for semen from reproductive organs 4 NEPHRON 5 NEPHRON • Functional unit of the kidney • ~ 1 million nephrons/kidney • Each nephron has two components – Vascular component – Tubular component • Arrangement of nephrons within kidney gives rise to two distinct regions – Outer region • Renal cortex – Inner region • Renal medulla 6 Nephron • Vascular component Glomerulus • Ball-like tuft of capillaries – From renal artery, inflowing blood passes through afferent arterioles which deliver blood to glomerulus – Efferent arteriole transports blood from glomerulus – Efferent arteriole breaks down into peritubular capillaries which surround tubular part of nephron – Peritubular capillaries join into venules which transport blood into the renal vein • Water and solutes are filtered through glomerulus as blood passes through it Renal artery Efferent arteriole Afferent arteriole Glomerulus FILTRATION PTC Renal vein 7 2 1 4 5 • Tubular component – Hollow, fluid-filled tube formed by a single layer of epithelial cells – Components 1.Bowman’s capsule 2. Proximal tubule 3. Loop of Henle – Descending limb – Ascending limb 3 6 4. Juxtaglomerular apparatus 5. Distal tubule 6. Collecting duct or tubule Basic Renal Processes • Glomerular filtration • Tubular reabsorption • Tubular secretion 8 9 1. FILTRATION Glomerular Filtration • Fluid filtered from the glomerulus into Bowman’s capsule pass through three layers of the glomerular membrane – Glomerular capillary wall • Single layer of endothelial cells • More permeable to water and solutes than capillaries elsewhere in the body – Basement membrane • Acellular gelatinous layer • Composed of collagen and glycoproteins – Inner layer of Bowman’s capsule • Consists of podocytes that encircle the glomerulus tuft 10 Glomerular Filtration -The glomerular filtration rate (GFR) is about 125 ml/min in a normal adult - Ultrafiltrate is cell and protein-free and the concentration of small solutes are the same as in plasma - The filtration barrier restricts movement of solutes on a basis of size and charge. Molecules < 1.8 nm freely filtered; >3.6 nm not filtered - Serum albumin has a radius if about 3.5 nm but its negative charge prevents its movement across basement membrane - In some diseases the negative charge on the filtration barrier is lost so that proteins are more readily filtered - a condition called proteinuria 11 Forces Involved in Glomerular Filtration • Three physical forces – Glomerular capillary pressure – Plasma-colloid pressure – Bowman’s capsule pressure involved blood osmotic hydrostatic Glomerular filtration rate depends on:• Net filtration pressure • How much glomerular surface area is available for penetration • How permeable the glomerular membrane is 12 Glomerular Filtration Rate Pathologically, plasma-colloid osmotic pressure and Bowman’s capsule hydrostatic pressure can change Plasma-colloid osmotic pressure - malnourished patient -loss of plasma proteins -Reduced colloid osmotic pressure -↑ GFR Bowman’s capsule hydrostatic pressure - Obstructions such as kidney stone of enlarged prostate can decrease filtration and elevate capsular hydrostatic pressure RENAL BLOOD FLOW (RBF) Renal blood flow is 25% of the cardiac output (1.25 l/min ) - RBF determines GFR Flow l/min 1.5 - RBF also modifies solute and water reabsorption and delivers 1.0 nutrients to nephron cells. 0.5 - Renal blood flow is autoregulated between 90 0 and 180 mm Hg 0 Renal blood flow GFR 100 200 Arterial blood pressure, mm Hg 13 RENAL BLOOD FLOW - AUTOREGULATION Autoregulation uncouples renal function from arterial blood pressure and ensures that fluid and solute excretion is constant. 1. Myogenic hypothesis When arterial pressure increases the renal afferent arteriole is stretched Increase of Flow arterial pressure increases Vascular smooth muscle contracts to increase resistance Increase of vascular tone Flow returns to normal 14 RENAL BLOOD FLOW - AUTOREGULATION 2. Tubuloglomerular feedback Alteration of tubular flow is sensed by the macula densa of the juxtaglomerular apparatus (JGA) and produces a signal that alters GFR. 15 Juxtaglomerular (granular) cells capillaries Efferent Arteriole Macula Densa Afferent Arteriole Distal tubule 16 2. REABSORPTION 17 18 Reabsorption Reabsorb: 99% H2O 100% glucose, amino acids 99.5% Na+ 50% urea. Most of this occurs at proximal convoluted tubule. Tubular Reabsorption • Passive reabsorption – No energy is required for the substance’s net movement – Occurs down electrochemical or osmotic gradients • Active reabsorption – Occurs if any one of the steps in transepithelial transport of a substance requires energy – Movement occurs against electrochemical gradient 19 • An active Na+ - K+ ATPase pump in basolateral membrane is essential for Na+ reabsorption • Of total energy spent by kidneys, 80% is used for Na+ transport • Water follows reabsorbed sodium by osmosis which has a main effect on blood volume and blood pressure Sodium Reabsorption 20 Na+ Reabsorption Tubule area % of Na+ reabsorbed Role of Na+ reabsorption Proximal tubule 67% Plays role in reabsorbing glucose, amino acids, H2O, Cl-, and urea Ascending limb of the loop of Henle 25% Plays critical role in kidneys’ ability to produce urine of varying concentrations Distal and collecting tubules 8% Variable and subject to hormonal control; plays role in regulating ECF volume 21 22 3. SECRETION 23 Tubular Secretion • Transfer of substances from peritubular capillaries into the tubular lumen • Involves transepithelial transport • Kidney tubules can selectively add some substances to the substances already filtered Tubular Secretion • Most important secretory systems are for – H+ • Important in regulating acid-base balance • Secreted in proximal, distal, and collecting tubules – K+ • Keeps plasma K+ concentration at appropriate level to maintain normal membrane excitability in muscles and nerves • Secreted only in the distal and collecting tubules under control of aldosterone – Organic ions • Accomplish more efficient elimination of foreign organic compounds from the body • Secreted only in the proximal tubule 24 • At the end of this lecture you should: Be familiar with the structure of the renal system and nephron Understand the factors that control GFR Be familiar with autoregulation and tubuloglomerular feeback Understand the processes of reabsorption and secretion Be familiar with the cellular mechanisms of sodium & glucose reabsorption 25