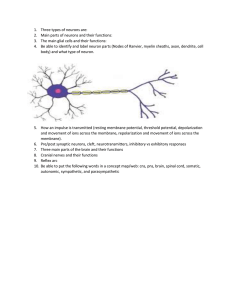
12-2 Neurons
advertisement

Chapter 9 Joints An Introduction to Joints • • Articulations o Body movement occurs at joints (articulations) where two bones connect Joint Structure o Determines direction and distance of movement (range of motion or ROM) o Joint strength decreases as mobility increases 9-1 Classification of Joints • Two Methods of Classification 1. Functional classification is based on range of motion of the joint 2. Structural classification relies on the anatomical organization of the joint 9-1 Classification of Joints • Functional Classifications o Synarthrosis (immovable joint) o Amphiarthrosis (slightly movable joint) o Diarthrosis (freely movable joint) 9-1 Classification of Joints • Structural Classifications o Bony o Fibrous o Cartilaginous o Synovial 9-1 Classification of Joints • Synarthroses (Immovable Joints) o Are very strong o Edges of bones may touch or interlock o Four types of synarthrotic joints 1. Suture 2. Gomphosis 3. Synchondrosis 4. Synostosis 9-1 Classification of Joints • Suture • o Bones interlocked o Are bound by dense fibrous connective tissue o Are found only in skull Gomphosis o Fibrous connection (periodontal ligament) o Binds teeth to sockets 9-1 Classification of Joints • • Synchondrosis o Is a rigid cartilaginous bridge between two bones Epiphyseal cartilage of long bones Between vertebrosternal ribs and sternum Synostosis o Fused bones, immovable Metopic suture of skull Epiphyseal lines of long bones 9-1 Classification of Joints • Amphiarthroses o More movable than synarthrosis o Stronger than freely movable joint o Two types of amphiarthroses 1. Syndesmosis o Bones connected by ligaments 2. Symphysis o Bones separated by fibrocartilage 9-1 Classification of Joints • Synovial Joints (Diarthroses) o Also called movable joints o At ends of long bones o Within articular capsules o Lined with synovial membrane 9-2 Synovial Joints • Articular Cartilages o Pad articulating surfaces within articular capsules Prevent bones from touching o Smooth surfaces lubricated by synovial fluid Reduce friction 9-2 Synovial Joints • Synovial Fluid o Contains slippery proteoglycans secreted by fibroblasts o Functions of synovial fluid 1. Lubrication 2. Nutrient distribution 3. Shock absorption 9-2 Synovial Joints • Accessory Structures o Cartilages o Fat pads o Ligaments o Tendons o Bursae 9-2 Synovial Joints • • • Cartilages o Cushion the joint Fibrocartilage pad called a meniscus (or articular disc; plural, menisci) Fat Pads o Superficial to the joint capsule o Protect articular cartilages Ligaments o Support, strengthen joints o Sprain – ligaments with torn collagen fibers 9-2 Synovial Joints • • Tendons o Attach to muscles around joint o Help support joint Bursae o Singular, bursa, a pouch o Pockets of synovial fluid o Cushion areas where tendons or ligaments rub 9-2 Synovial Joints • Factors That Stabilize Synovial Joints o Prevent injury by limiting range of motion Collagen fibers (joint capsule, ligaments) Articulating surfaces and menisci Other bones, muscles, or fat pads Tendons of articulating bones 9-2 Synovial Joints • Injuries o Dislocation (luxation) Articulating surfaces forced out of position Damages articular cartilage, ligaments, joint capsule o Subluxation A partial dislocation 9-3 Movements • • Three Types of Dynamic Motion 1. Linear movement (gliding) 2. Angular movement 3. Rotation Planes (Axes) of Dynamic Motion o Monaxial (1 axis) o Biaxial (2 axes) o Triaxial (3 axes) 9-3 Movements • Types of Movement at Synovial Joints o Terms describe: Plane or direction of motion Relationship between structures • 9-3 Movements • Types of Movement at Synovial Joints o Gliding movement Two surfaces slide past each other o Between carpal or tarsal bones 9-3 Movements • Angular Movement o Flexion Angular motion Anterior–posterior plane Reduces angle between elements o Extension Angular motion Anterior–posterior plane Increases angle between elements 9-3 Movements • Angular Movement o Hyperextension Angular motion Extension past anatomical position 9-3 Movements • Angular Movement o Abduction Angular motion Frontal plane Moves away from longitudinal axis o Adduction Angular motion Frontal plane Moves toward longitudinal axis 9-3 Movements • Angular Movement o Circumduction Circular motion without rotation Angular motion 9-3 Movements • Types of Movement at Synovial Joints o Rotation Direction of rotation from anatomical position Relative to longitudinal axis of body Left or right rotation Medial rotation (inward rotation) o Rotates toward axis Lateral rotation (outward rotation) o Rotates away from axis 9-3 Movements • Types of Movements at Synovial Joints o Rotation Pronation o Rotates forearm, radius over ulna Supination o Forearm in anatomical position Figure 9-4b Rotational Movements. 9-3 Movements • Special Movements o Inversion Twists sole of foot medially o Eversion Twists sole of foot laterally o Dorsiflexion Flexion at ankle (lifting toes) o Plantar flexion Extension at ankle (pointing toes) 9-3 Movements • Special Movements o Opposition Thumb movement toward fingers or palm (grasping) o Reposition Opposite of opposition o Protraction Moves anteriorly In the horizontal plane (pushing forward) o Retraction Opposite of protraction Moving anteriorly (pulling back) 9-3 Movements • Special Movements o Elevation Moves in superior direction (up) o Depression Moves in inferior direction (down) o Lateral flexion Bends vertebral column from side to side 9-3 Movements • Functional Classification of Synovial Joints o Gliding o Hinge o Pivot o Condylar o Saddle o Ball-and-socket 9-3 Movements • • • Gliding Joints o Flattened or slightly curved faces o Limited motion (nonaxial) Hinge Joints o Angular motion in a single plane (monaxial) Condylar Joints o Oval articular face within a depression o Motion in two planes (biaxial) 9-3 Movements • • • Saddle Joints o Two concave, straddled (biaxial) Pivot Joints o Rotation only (monaxial) Ball-and-Socket Joints o Round articular face in a depression (triaxial) 9-3 Movements • Joints o A joint cannot be both mobile and strong o The greater the mobility, the weaker the joint o Mobile joints are supported by muscles and ligaments, not bone-to-bone connections 9-4 Intervertebral Joints • Intervertebral Joints o C2 to L5 spinal vertebrae articulate: At inferior and superior articular processes (gliding joints) Between adjacent vertebral bodies (symphyseal joints) 9-4 Intervertebral Joints • Intervertebral Discs o Pads of fibrocartilage o Separate vertebral bodies o Anulus fibrosus Tough outer layer Attaches disc to vertebrae o Nucleus pulposus Elastic, gelatinous core Absorbs shocks 9-4 Intervertebral Joints • • Vertebral Joints o Also called symphyseal joints o As vertebral column moves: Nucleus pulposus shifts Disc shape conforms to motion Intervertebral Ligaments o Bind vertebrae together o Stabilize the vertebral column 9-4 Intervertebral Joints • Six Intervertebral Ligaments 1. Anterior longitudinal ligament Connects anterior bodies 2. Posterior longitudinal ligament Connects posterior bodies 3. Ligamentum flavum Connects laminae 9-4 Intervertebral Joints • Six Intervertebral Ligaments 4. Interspinous ligament Connects spinous processes 5. Supraspinous ligament Connects tips of spinous processes (C7 to sacrum) 6. Ligamentum nuchae Continues supraspinous ligament (C7 to skull) 9-4 Intervertebral Joints • Damage to Intervertebral Discs o Slipped disc Bulge in anulus fibrosus Invades vertebral canal o Herniated disc Nucleus pulposus breaks through anulus fibrosus Presses on spinal cord or nerves 9-4 Intervertebral Joints • Movements of the Vertebral Column 1. Flexion 2. Extension 3. Lateral flexion 4. Rotation 9-5 The Shoulder Joint • The Shoulder Joint o Also called the glenohumeral joint o Allows more motion than any other joint o Is the least stable o Supported by skeletal muscles, tendons, ligaments o Ball-and-socket diarthrosis o Between head of humerus and glenoid cavity of scapula 9-5 The Shoulder Joint • Socket of the Shoulder Joint o Glenoid labrum Deepens socket of glenoid cavity Fibrocartilage lining Extends past the bone 9-5 The Shoulder Joint • Processes of the Shoulder Joint o Acromion (clavicle) and coracoid process (scapula) Project laterally, superior to the humerus Help stabilize the joint 9-5 The Shoulder Joint • • Shoulder Ligaments o Glenohumeral o Coracohumeral o Coracoacromial o Coracoclavicular o Acromioclavicular Shoulder Separation o Dislocation of the shoulder joint 9-5 The Shoulder Joint • Shoulder Muscles (Rotator Cuff) o Supraspinatus o Infraspinatus o Subscapularis o Teres minor 9-5 The Shoulder Joint • Shoulder Bursae o Subacromial o Subcoracoid o Subdeltoid o Subscapular 9-5 The Elbow Joint • The Elbow Joint o A stable hinge joint o With articulations involving humerus, radius, and ulna 9-5 The Elbow Joint • Joints of the Elbow o Humeroulnar joint Largest joint Trochlea of humerus and trochlear notch of ulna Limited movement 9-5 The Elbow Joint • Joints of the Elbow o Humeroradial joint Smaller joint Capitulum of humerus and head of radius 9-5 The Elbow Joint • Supporting Structures of the Elbow o Biceps brachii muscle Attached to radial tuberosity Controls elbow motion o Elbow ligaments Radial collateral Annular Ulnar collateral 9-6 The Hip Joint • The Hip Joint o Also called coxal joint o Strong ball-and-socket diarthrosis o Wide range of motion 9-6 The Hip Joint • Structures of the Hip Joint o Head of femur fits into it o Socket of acetabulum o Which is extended by fibrocartilaginous acetabular labrum 9-6 The Hip Joint • Ligaments of the Hip Joint o Iliofemoral o Pubofemoral o Ischiofemoral o Transverse acetabular o Ligamentum teres 9-6 The Knee Joint • The Knee Joint o A complicated hinge joint o Transfers weight from femur to tibia o Articulations of the knee joint Two femur–tibia articulations o At medial and lateral condyles One between patella and patellar surface of femur 9-6 The Knee Joint • The Articular Capsule and Joint Cavity o Medial and lateral menisci Fibrocartilage pads At femur–tibia articulations Cushion and stabilize joint Give lateral support 9-6 The Knee Joint • Seven Major Supporting Ligaments 1. Patellar ligament (anterior) 2. & 3. Two popliteal ligaments (posterior) 4. & 5. Anterior and posterior cruciate ligaments (inside joint capsule) 6. Tibial collateral ligament (medial) 7. Fibular collateral ligament (lateral) 9-7 Effects of Aging on Joints • Degenerative Changes o Rheumatism A pain and stiffness of skeletal and muscular systems o Arthritis All forms of rheumatism that damage articular cartilages of synovial joints o Osteoarthritis Caused by wear and tear of joint surfaces, or genetic factors affecting collagen formation Generally in people over age 60 9-7 Effects of Aging on Joints • • Rheumatoid Arthritis o An inflammatory condition o Caused by infection, allergy, or autoimmune disease o Involves the immune system Gouty Arthritis o Occurs when crystals (uric acid or calcium salts) Form within synovial fluid Due to metabolic disorders 9-7 Effects of Aging on Joints • • Joint Immobilization o Reduces flow of synovial fluid o Can cause arthritis symptoms o Treated by continuous passive motion or CPM (therapy) Bones and Aging o Bone mass decreases o Bones weaken o Increases risk of hip fracture, hip dislocation, or pelvic fracture 9-8 Integration with Other Systems • Bone Recycling o Living bones maintain equilibrium between: Bone building (osteoblasts) And breakdown (osteoclasts) 9-8 Integration with Other Systems • Factors Affecting Bone Strength 1. Age 2. Physical stress 3. Hormone levels 4. Calcium and phosphorus uptake and excretion 5. Genetic and environmental factors 9-8 Integration with Other Systems • Bones Support Body Systems o Support and protect other systems o Store fat, calcium, and phosphorus o Manufacture cells for immune system 9-8 Integration with Other Systems • Bones Support Body Systems o Disorders in other body systems can cause: Bone tumors Osteoporosis Arthritis Rickets (vitamin D deficiency) Chapter 10 Muscle Tissue 10-1 An Introduction to Muscle Tissue • Learning Outcomes o 10-1 Specify the functions of skeletal muscle tissue. o 10-2 Describe the organization of muscle at the tissue level. o 10-3 Describe the characteristics of skeletal muscle fibers, and identify the structural components of a sarcomere. o 10-4 Identify the components of the neuromuscular junction, and summarize the events involved in the neural control of skeletal muscle contraction and relaxation. 10-1 An Introduction to Muscle Tissue • Learning Outcomes o 10-5 Describe the mechanism responsible for tension production in a muscle fiber, and compare the different types of muscle contraction. o 10-6 Describe the mechanisms by which muscle fibers obtain the energy to power contractions. o 10-7 Relate the types of muscle fibers to muscle performance, and distinguish between aerobic and anaerobic endurance. 10-1 An Introduction to Muscle Tissue • Learning Outcomes o 10-8 Identify the structural and functional differences between skeletal muscle fibers and cardiac muscle cells. o 10-9 Identify the structural and functional differences between skeletal muscle fibers and smooth muscle cells, and discuss the roles of smooth muscle tissue in systems throughout the body. An Introduction to Muscle Tissue • Muscle Tissue o A primary tissue type, divided into: Skeletal muscle tissue Cardiac muscle tissue Smooth muscle tissue 10-1 Functions of Skeletal Muscle Tissue • Skeletal Muscles o Are attached to the skeletal system o Allow us to move o The muscular system Includes only skeletal muscles 10-1 Functions of Skeletal Muscle Tissue • Six Functions of Skeletal Muscle Tissue 1. Produce skeletal movement 2. Maintain posture and body position 3. Support soft tissues 4. Guard entrances and exits 5. Maintain body temperature 6. Store nutrient reserves 10-2 Organization of Muscle • Skeletal Muscle o Muscle tissue (muscle cells or fibers) o Connective tissues o Nerves o Blood vessels 10-2 Organization of Muscle • Organization of Connective Tissues o Muscles have three layers of connective tissues 1. Epimysium 2. Perimysium 3. Endomysium 10-2 Organization of Muscle • Epimysium o Exterior collagen layer o Connected to deep fascia o Separates muscle from surrounding tissues 10-2 Organization of Muscle • Perimysium o Surrounds muscle fiber bundles (fascicles) o Contains blood vessel and nerve supply to fascicles 10-2 Organization of Muscle • Endomysium o Surrounds individual muscle cells (muscle fibers) o Contains capillaries and nerve fibers contacting muscle cells o Contains myosatellite cells (stem cells) that repair damage 10-2 Organization of Muscle • Organization of Connective Tissues o Muscle Attachments Endomysium, perimysium, and epimysium come together: o At ends of muscles o To form connective tissue attachment to bone matrix o i.e., tendon (bundle) or aponeurosis (sheet) 10-2 Organization of Muscle • Blood Vessels and Nerves o Muscles have extensive vascular systems that: Supply large amounts of oxygen Supply nutrients Carry away wastes o Skeletal muscles are voluntary muscles, controlled by nerves of the central nervous system (brain and spinal cord) 10-3 Characteristics of Skeletal Muscle Fibers • Skeletal Muscle Cells o Are very long o Develop through fusion of mesodermal cells (myoblasts) o Become very large o Contain hundreds of nuclei 10-3 Characteristics of Skeletal Muscle Fibers • The Sarcolemma and Transverse Tubules o The sarcolemma The cell membrane of a muscle fiber (cell) Surrounds the sarcoplasm (cytoplasm of muscle fiber) A change in transmembrane potential begins contractions 10-3 Characteristics of Skeletal Muscle Fibers • The Sarcolemma and Transverse Tubules o Transverse tubules (T tubules) Transmit action potential through cell Allow entire muscle fiber to contract simultaneously Have same properties as sarcolemma 10-3 Characteristics of Skeletal Muscle Fibers • Myofibrils o Lengthwise subdivisions within muscle fiber o Made up of bundles of protein filaments (myofilaments) o Myofilaments are responsible for muscle contraction o Types of myofilaments: Thin filaments o Made of the protein actin Thick filaments o Made of the protein myosin 10-3 Characteristics of Skeletal Muscle Fibers • The Sarcoplasmic Reticulum (SR) o A membranous structure surrounding each myofibril o Helps transmit action potential to myofibril o Similar in structure to smooth endoplasmic reticulum o Forms chambers (terminal cisternae) attached to T tubules 10-3 Characteristics of Skeletal Muscle Fibers • The Sarcoplasmic Reticulum (SR) o Triad Is formed by one T tubule and two terminal cisternae Cisternae o Concentrate Ca2+ (via ion pumps) o Release Ca2+ into sarcomeres to begin muscle contraction 10-3 Structural Components of a Sarcomere • Sarcomeres o The contractile units of muscle o Structural units of myofibrils o Form visible patterns within myofibrils o A striped or striated pattern within myofibrils Alternating dark, thick filaments (A bands) and light, thin filaments (I bands) 10-3 Structural Components of a Sarcomere • Sarcomeres o The A Band M line o The center of the A band o At midline of sarcomere The H Band o The area around the M line o Has thick filaments but no thin filaments Zone of overlap o The densest, darkest area on a light micrograph o Where thick and thin filaments overlap 10-3 Structural Components of a Sarcomere • Sarcomeres o The I Band Z lines o The centers of the I bands o At two ends of sarcomere Titin o Are strands of protein o Reach from tips of thick filaments to the Z line o Stabilize the filaments 10-3 Structural Components of a Sarcomere • Thin Filaments o F-actin (filamentous actin) Is two twisted rows of globular G-actin The active sites on G-actin strands bind to myosin o Nebulin Holds F-actin strands together 10-3 Structural Components of a Sarcomere • Thin Filaments o Tropomyosin Is a double strand Prevents actin–myosin interaction o Troponin A globular protein Binds tropomyosin to G-actin Controlled by Ca2+ 10-3 Structural Components of a Sarcomere • Initiating Contraction o Ca2+ binds to receptor on troponin molecule o Troponin–tropomyosin complex changes o Exposes active site of F-actin 10-3 Structural Components of a Sarcomere • Thick Filaments o Contain about 300 twisted myosin subunits o Contain titin strands that recoil after stretching o The mysosin molecule Tail o Binds to other myosin molecules Head o Made of two globular protein subunits o Reaches the nearest thin filament 10-3 Structural Components of a Sarcomere • Myosin Action o During contraction, myosin heads: Interact with actin filaments, forming cross-bridges Pivot, producing motion 10-3 Structural Components of a Sarcomere • Sliding Filaments and Muscle Contraction o Sliding filament theory Thin filaments of sarcomere slide toward M line, alongside thick filaments The width of A zone stays the same Z lines move closer together 10-3 Structural Components of a Sarcomere • Skeletal Muscle Contraction o The process of contraction Neural stimulation of sarcolemma o Causes excitation–contraction coupling Muscle fiber contraction o Interaction of thick and thin filaments Tension production 10-4 Components of the Neuromuscular Junction • The Control of Skeletal Muscle Activity o The neuromuscular junction (NMJ) Special intercellular connection between the nervous system and skeletal muscle fiber Controls calcium ion release into the sarcoplasm 10-4 Components of the Neuromuscular Junction • Excitation–Contraction Coupling o Action potential reaches a triad Releasing Ca2+ Triggering contraction o Requires myosin heads to be in “cocked” position Loaded by ATP energy 10-4 Skeletal Muscle Contraction • The Contraction Cycle 1. Contraction Cycle Begins 2. Active-Site Exposure 3. Cross-Bridge Formation 4. Myosin Head Pivoting 5. Cross-Bridge Detachment 6. Myosin Reactivation 10-4 Skeletal Muscle Contraction • Fiber Shortening o As sarcomeres shorten, muscle pulls together, producing tension o Muscle shortening can occur at both ends of the muscle, or at only one end of the muscle This depends on the way the muscle is attached at the ends 10-4 Skeletal Muscle Relaxation • Relaxation o Contraction duration Depends on: o Duration of neural stimulus o Number of free calcium ions in sarcoplasm o Availability of ATP 10-4 Skeletal Muscle Relaxation • • Relaxation o Ca2+ concentrations fall o Ca2+ detaches from troponin o Active sites are re-covered by tropomyosin Rigor Mortis o A fixed muscular contraction after death o Caused when: Ion pumps cease to function; ran out of ATP Calcium builds up in the sarcoplasm 10-4 Skeletal Muscle Contraction and Relaxation • Summary o Skeletal muscle fibers shorten as thin filaments slide between thick filaments o Free Ca2+ in the sarcoplasm triggers contraction o SR releases Ca2+ when a motor neuron stimulates the muscle fiber o Contraction is an active process o Relaxation and return to resting length are passive 10-5 Tension Production and Contraction Types • Tension Production by Muscles Fibers o As a whole, a muscle fiber is either contracted or relaxed o Depends on: The number of pivoting cross-bridges The fiber’s resting length at the time of stimulation The frequency of stimulation 10-5 Tension Production and Contraction Types • Tension Production by Muscles Fibers o Length–Tension Relationships Number of pivoting cross-bridges depends on: o Amount of overlap between thick and thin fibers Optimum overlap produces greatest amount of tension o Too much or too little reduces efficiency Normal resting sarcomere length o Is 75 to 130 percent of optimal length 10-5 Tension Production and Contraction Types • Tension Production by Muscle Fibers o The Frequency of Stimulation A single neural stimulation produces: o A single contraction or twitch o Which lasts about 7–100 msec. Sustained muscular contractions o Require many repeated stimuli 10-5 Tension Production and Contraction Types • Tension Production by Muscle Fibers o Twitches 1. Latent period o The action potential moves through sarcolemma o Causing Ca2+ release 2. Contraction phase o Calcium ions bind o Tension builds to peak 3. Relaxation phase o Ca2+ levels fall o Active sites are covered and tension falls to resting levels 10-5 Tension Production and Contraction Types • Tension Production by Muscle Fibers o Treppe A stair-step increase in twitch tension Repeated stimulations immediately after relaxation phase o Stimulus frequency 50/second Causes a series of contractions with increasing tension 10-5 Tension Production and Contraction Types • Tension Production by Muscle Fibers o Wave summation Increasing tension or summation of twitches Repeated stimulations before the end of relaxation phase o Stimulus frequency 50/second Causes increasing tension or summation of twitches 10-5 Tension Production and Contraction Types • Tension Production by Muscle Fibers o Incomplete tetanus Twitches reach maximum tension If rapid stimulation continues and muscle is not allowed to relax, twitches reach maximum level of tension o Complete tetanus If stimulation frequency is high enough, muscle never begins to relax, and is in continuous contraction 10-5 Tension Production and Contraction Types • Tension Production by Skeletal Muscles o Depends on: Internal tension produced by muscle fibers External tension exerted by muscle fibers on elastic extracellular fibers Total number of muscle fibers stimulated 10-5 Tension Production and Contraction Types • Motor Units and Tension Production o Motor units in a skeletal muscle: Contain hundreds of muscle fibers That contract at the same time Controlled by a single motor neuron 10-5 Tension Production and Contraction Types • Motor Units and Tension Production o Recruitment (multiple motor unit summation) In a whole muscle or group of muscles, smooth motion and increasing tension are produced by slowly increasing the size or number of motor units stimulated o Maximum tension Achieved when all motor units reach tetanus Can be sustained only a very short time 10-5 Tension Production and Contraction Types • Motor Units and Tension Production o Sustained tension Less than maximum tension Allows motor units to rest in rotation o Muscle tone The normal tension and firmness of a muscle at rest Muscle units actively maintain body position, without motion Increasing muscle tone increases metabolic energy used, even at rest 10-5 Tension Production and Contraction Types • Motor Units and Tension Production o Contractions are classified based on pattern of tension production Isotonic contraction Isometric contraction 10-5 Tension Production and Contraction Types • Isotonic Contraction o Skeletal muscle changes length Resulting in motion o If muscle tension load (resistance): Muscle shortens (concentric contraction) o If muscle tension load (resistance): Muscle lengthens (eccentric contraction) 10-5 Tension Production and Contraction Types • Isometric Contraction o Skeletal muscle develops tension, but is prevented from changing length o iso- same, metric measure 10-5 Tension Production and Contraction Types • Load and Speed of Contraction o Are inversely related o The heavier the load (resistance) on a muscle: The longer it takes for shortening to begin And the less the muscle will shorten 10-5 Tension Production and Contraction Types • Muscle Relaxation and the Return to Resting Length o Elastic forces The pull of elastic elements (tendons and ligaments) Expands the sarcomeres to resting length o Opposing muscle contractions Reverse the direction of the original motion Are the work of opposing skeletal muscle pairs 10-5 Tension Production and Contraction Types • Muscle Relaxation and the Return to Resting Length o Gravity Can take the place of opposing muscle contraction to return a muscle to its resting state 10-6 Energy to Power Contractions • ATP Provides Energy for Muscle Contraction o Sustained muscle contraction uses a lot of ATP energy o Muscles store enough energy to start contraction o Muscle fibers must manufacture more ATP as needed 10-6 Energy to Power Contractions • • ATP and CP Reserves o Adenosine triphosphate (ATP) The active energy molecule o Creatine phosphate (CP) The storage molecule for excess ATP energy in resting muscle Energy recharges ADP to ATP o Using the enzyme creatine kinase (CK) o When CP is used up, other mechanisms generate ATP 10-6 Energy to Power Contractions • ATP Generation o Cells produce ATP in two ways 1. Aerobic metabolism of fatty acids in the mitochondria 2. Anaerobic glycolysis in the cytoplasm 10-6 Energy to Power Contractions • • Aerobic Metabolism o Is the primary energy source of resting muscles o Breaks down fatty acids o Produces 34 ATP molecules per glucose molecule Glycolysis o Is the primary energy source for peak muscular activity o Produces two ATP molecules per molecule of glucose o Breaks down glucose from glycogen stored in skeletal muscles 10-6 Energy to Power Contractions • Energy Use and the Level of Muscular Activity o Skeletal muscles at rest metabolize fatty acids and store glycogen o During light activity, muscles generate ATP through anaerobic breakdown of carbohydrates, lipids, or amino acids o At peak activity, energy is provided by anaerobic reactions that generate lactic acid as a by-product 10-6 Energy to Power Contractions • • Muscle Fatigue o When muscles can no longer perform a required activity, they are fatigued Results of Muscle Fatigue o Depletion of metabolic reserves o Damage to sarcolemma and sarcoplasmic reticulum o Low pH (lactic acid) o Muscle exhaustion and pain 10-6 Energy to Power Contractions • The Recovery Period o The time required after exertion for muscles to return to normal o Oxygen becomes available o Mitochondrial activity resumes 10-6 Energy to Power Contractions • Lactic Acid Removal and Recycling o The Cori Cycle The removal and recycling of lactic acid by the liver Liver converts lactate to pyruvate Glucose is released to recharge muscle glycogen reserves 10-6 Energy to Power Contractions • The Oxygen Debt o After exercise or other exertion: The body needs more oxygen than usual to normalize metabolic activities Resulting in heavy breathing Also called excess postexercise oxygen consumption (EPOC) 10-6 Energy to Power Contractions • Heat Production and Loss o Active muscles produce heat o Up to 70 percent of muscle energy can be lost as heat, raising body temperature 10-6 Energy to Power Contractions • Hormones and Muscle Metabolism o Growth hormone o Testosterone o Thyroid hormones o Epinephrine 10-7 Types of Muscle Fibers and Endurance • Muscle Performance o Force The maximum amount of tension produced o Endurance The amount of time an activity can be sustained o Force and endurance depend on: The types of muscle fibers Physical conditioning 10-7 Types of Muscle Fibers and Endurance • Three Major Types of Skeletal Muscle Fibers 1. Fast fibers 2. Slow fibers 3. Intermediate fibers 10-7 Types of Muscle Fibers and Endurance • Fast Fibers o Contract very quickly o Have large diameter, large glycogen reserves, few mitochondria o Have strong contractions, fatigue quickly 10-7 Types of Muscle Fibers and Endurance • Slow Fibers o Are slow to contract, slow to fatigue o Have small diameter, more mitochondria o Have high oxygen supply o Contain myoglobin (red pigment, binds oxygen) 10-7 Types of Muscle Fibers and Endurance • Intermediate Fibers o Are mid-sized o Have low myoglobin o Have more capillaries than fast fibers, slower to fatigue 10-7 Types of Muscle Fibers and Endurance • Muscle Performance and the Distribution of Muscle Fibers o White muscles Mostly fast fibers Pale (e.g., chicken breast) o Red muscles Mostly slow fibers Dark (e.g., chicken legs) o Most human muscles Mixed fibers Pink 10-7 Types of Muscle Fibers and Endurance • • Muscle Hypertrophy o Muscle growth from heavy training Increases diameter of muscle fibers Increases number of myofibrils Increases mitochondria, glycogen reserves Muscle Atrophy o Lack of muscle activity Reduces muscle size, tone, and power 10-7 Types of Muscle Fibers and Endurance • Physical Conditioning o Improves both power and endurance Anaerobic activities (e.g., 50-meter dash, weightlifting) o Use fast fibers o Fatigue quickly with strenuous activity Improved by: o Frequent, brief, intensive workouts Causes hypertrophy 10-7 Types of Muscle Fibers and Endurance • Physical Conditioning o Improves both power and endurance Aerobic activities (prolonged activity) o Supported by mitochondria o Require oxygen and nutrients Improves: o Endurance by training fast fibers to be more like intermediate fibers o Cardiovascular performance 10-7 Types of Muscle Fibers and Endurance • Importance of Exercise o What you don’t use, you lose o Muscle tone indicates base activity in motor units of skeletal muscles o Muscles become flaccid when inactive for days or weeks o Muscle fibers break down proteins, become smaller and weaker o With prolonged inactivity, fibrous tissue may replace muscle fibers Chapter 12 Neural Tissue An Introduction to the Nervous System • The Nervous System o Includes all neural tissue in the body o Neural tissue contains two kinds of cells 1. Neurons o Cells that send and receive signals 2. Neuroglia (glial cells) o Cells that support and protect neurons An Introduction to the Nervous System • Organs of the Nervous System o Brain and spinal cord o Sensory receptors of sense organs (eyes, ears, etc.) o Nerves connect nervous system with other systems 12-1 Divisions of the Nervous System • Anatomical Divisions of the Nervous System o Central nervous system (CNS) o Peripheral nervous system (PNS) 12-1 Divisions of the Nervous System • The Central Nervous System (CNS) o Consists of the spinal cord and brain o Contains neural tissue, connective tissues, and blood vessels o Functions of the CNS are to process and coordinate: Sensory data from inside and outside body Motor commands control activities of peripheral organs (e.g., skeletal muscles) Higher functions of brain: intelligence, memory, learning, emotion 12-1 Divisions of the Nervous System • The Peripheral Nervous System (PNS) o Includes all neural tissue outside the CNS o Functions of the PNS Deliver sensory information to the CNS Carry motor commands to peripheral tissues and systems 12-1 Divisions of the Nervous System • The Peripheral Nervous System (PNS) o Nerves (also called peripheral nerves) Bundles of axons with connective tissues and blood vessels Carry sensory information and motor commands in PNS o Cranial nerves – connect to brain o Spinal nerves – attach to spinal cord 12-1 Divisions of the Nervous System • Functional Divisions of the PNS o Afferent division Carries sensory information From PNS sensory receptors to CNS o Efferent division Carries motor commands From CNS to PNS muscles and glands 12-1 Divisions of the Nervous System • Functional Divisions of the PNS o Receptors and effectors of afferent division Receptors o Detect changes or respond to stimuli o Neurons and specialized cells o Complex sensory organs (e.g., eyes, ears) Effectors o Respond to efferent signals o Cells and organs 12-1 Divisions of the Nervous System • Functional Divisions of the PNS o The efferent division Somatic nervous system (SNS) o Controls voluntary and involuntary (reflexes) skeletal muscle contractions 12-1 Divisions of the Nervous System • Functional Divisions of the PNS o The efferent division Autonomic nervous system (ANS) o Controls subconscious actions, contractions of smooth muscle and cardiac muscle, and glandular secretions o Sympathetic division has a stimulating effect o Parasympathetic division has a relaxing effect 12-2 Neurons • Neurons o The basic functional units of the nervous system o The structure of neurons The multipolar neuron o Common in the CNS Cell body (soma) Short, branched dendrites Long, single axon 12-2 Neurons • The Cell Body o Large nucleus and nucleolus o Perikaryon (cytoplasm) o Mitochondria (produce energy) o RER and ribosomes (produce neurotransmitters) 12-2 Neurons • The Cell Body o Cytoskeleton Neurofilaments and neurotubules in place of microfilaments and microtubules Neurofibrils: bundles of neurofilaments that provide support for dendrites and axon o Nissl bodies Dense areas of RER and ribosomes Make neural tissue appear gray (gray matter) 12-2 Neurons • Dendrites o Highly branched o Dendritic spines Many fine processes Receive information from other neurons 80–90 percent of neuron surface area 12-2 Neurons • The axon o Is long o Carries electrical signal (action potential) to target o Axon structure is critical to function o 12-2 Neurons • Structures of the Axon o Axoplasm Cytoplasm of axon Contains neurofibrils, neurotubules, enzymes, organelles o Axolemma Specialized cell membrane Covers the axoplasm 12-2 Neurons • Structures of the Axon o Axon hillock Thick section of cell body Attaches to initial segment o Initial segment Attaches to axon hillock 12-2 Neurons • Structures of the Axon o Collaterals Branches of a single axon o Telodendria Fine extensions of distal axon o Axon terminals Tips of telodendria 12-2 Neurons • The Structure of Neurons o The synapse Area where a neuron communicates with another cell 12-2 Neurons • The Structure of Neurons o The synapse Presynaptic cell o Neuron that sends message Postsynaptic cell o Cell that receives message The synaptic cleft o The small gap that separates the presynaptic membrane and the postsynaptic membrane 12-2 Neurons • The Synapse o The synaptic terminal Is expanded area of axon of presynaptic neuron Contains synaptic vesicles of neurotransmitters 12-2 Neurons • Neurotransmitters o Are chemical messengers o Are released at presynaptic membrane o Affect receptors of postsynaptic membrane o Are broken down by enzymes o Are reassembled at axon terminal 12-2 Neurons • Recycling Neurotransmitters o Axoplasmic transport Neurotubules within the axon Transport raw materials Between cell body and axon terminal Powered by mitochondria, kinesin, and dynein 12-2 Neurons • Types of Synapses o Neuromuscular junction Synapse between neuron and muscle o Neuroglandular junction Synapse between neuron and gland 12-2 Neurons • Structural Classification of Neurons o Anaxonic neurons Found in brain and sense organs o Bipolar neurons Found in special sensory organs (sight, smell, hearing) o Unipolar neurons Found in sensory neurons of PNS o Multipolar neurons Common in the CNS Include all skeletal muscle motor neurons 12-2 Neurons • Anaxonic Neurons o Small • o All cell processes look alike Bipolar Neurons o Are small o One dendrite, one axon 12-2 Neurons • • Unipolar Neurons o Also called pseudounipolar neurons o Have very long axons o Fused dendrites and axon o Cell body to one side Multipolar Neurons o Have very long axons o Multiple dendrites, one axon 12-2 Neurons • Three Functional Classifications of Neurons 1. Sensory neurons Afferent neurons of PNS 2. Motor neurons Efferent neurons of PNS 3. Interneurons Association neurons 12-2 Neurons • • Functions of Sensory Neurons o Monitor internal environment (visceral sensory neurons) o Monitor effects of external environment (somatic sensory neurons) Structures of Sensory Neurons o Unipolar o Cell bodies grouped in sensory ganglia o Processes (afferent fibers) extend from sensory receptors to CNS 12-2 Neurons • Three Types of Sensory Receptors 1. Interoceptors Monitor internal systems (digestive, respiratory, cardiovascular, urinary, reproductive) Internal senses (taste, deep pressure, pain) 2. Exteroceptors External senses (touch, temperature, pressure) Distance senses (sight, smell, hearing) 3. Proprioceptors Monitor position and movement (skeletal muscles and joints) 12-2 Neurons • Motor Neurons o Carry instructions from CNS to peripheral effectors o Via efferent fibers (axons) 12-2 Neurons • Motor Neurons o Two major efferent systems 1. Somatic nervous system (SNS) o Includes all somatic motor neurons that innervate skeletal muscles 2. Autonomic (visceral) nervous system (ANS) o Visceral motor neurons innervate all other peripheral effectors Smooth muscle, cardiac muscle, glands, adipose tissue 12-2 Neurons • Motor Neurons o Two groups of efferent axons Signals from CNS motor neurons to visceral effectors pass synapses at autonomic ganglia dividing axons into: o Preganglionic fibers o Postganglionic fibers 12-2 Neurons • Interneurons o Most are located in brain, spinal cord, and autonomic ganglia Between sensory and motor neurons o Are responsible for: Distribution of sensory information Coordination of motor activity o Are involved in higher functions Memory, planning, learning 12-3 Neuroglia • Neuroglia o Half the volume of the nervous system o Many types of neuroglia in CNS and PNS 12-3 Neuroglia • Four Types of Neuroglia in the CNS 1. Ependymal cells Cells with highly branched processes; contact neuroglia directly 2. Astrocytes Large cell bodies with many processes 3. Oligodendrocytes Smaller cell bodies with fewer processes 4. Microglia Smallest and least numerous neuroglia with many fine-branched processes 12-3 Neuroglia • Ependymal Cells o Form epithelium called ependyma o Line central canal of spinal cord and ventricles of brain Secrete cerebrospinal fluid (CSF) Have cilia or microvilli that circulate CSF Monitor CSF Contain stem cells for repair 12-3 Neuroglia • Astrocytes o Maintain blood–brain barrier (isolates CNS) o Create three-dimensional framework for CNS o Repair damaged neural tissue o Guide neuron development o Control interstitial environment 12-3 Neuroglia • Oligodendrocytes o Myelination Increases speed of action potentials Myelin insulates myelinated axons Makes nerves appear white 12-3 Neuroglia • Oligodendrocytes o Nodes and internodes Internodes – myelinated segments of axon Nodes (also called nodes of Ranvier) o Gaps between internodes o Where axons may branch 12-3 Neuroglia • Myelination o White matter Regions of CNS with many myelinated nerves o Gray matter Unmyelinated areas of CNS 12-3 Neuroglia • Microglia o Migrate through neural tissue o Clean up cellular debris, waste products, and pathogens 12-3 Neuroglia • Neuroglia of the Peripheral Nervous System o Ganglia Masses of neuron cell bodies Surrounded by neuroglia Found in the PNS 12-3 Neuroglia • Neuroglia of the Peripheral Nervous System o Satellite cells Also called amphicytes Surround ganglia Regulate environment around neuron 12-3 Neuroglia • Neuroglia of the Peripheral Nervous System o Schwann cells Also called neurilemma cells Form myelin sheath (neurilemma) around peripheral axons One Schwann cell sheaths one segment of axon o Many Schwann cells sheath entire axon 12-3 Neuroglia • Neurons and Neuroglia o Neurons perform: All communication, information processing, and control functions of the nervous system o Neuroglia preserve: Physical and biochemical structure of neural tissue o Neuroglia are essential to: Survival and function of neurons 12-3 Neuroglia • Neural Responses to Injuries o Wallerian degeneration Axon distal to injury degenerates o Schwann cells Form path for new growth Wrap new axon in myelin 12-3 Neuroglia • Nerve Regeneration in CNS o Limited by chemicals released by astrocytes that: Block growth Produce scar tissue 12-4 Membrane Potential • Ion Movements and Electrical Signals o All plasma (cell) membranes produce electrical signals by ion movements o Membrane potential is particularly important to neurons 12-4 Membrane Potential • Five Main Membrane Processes in Neural Activities 1. Resting potential The membrane potential of resting cell 2. Graded potential Temporary, localized change in resting potential Caused by stimulus 12-4 Membrane Potential • Five Main Membrane Processes in Neural Activities 3. Action potential Is an electrical impulse Produced by graded potential Propagates along surface of axon to synapse 12-4 Membrane Potential • Five Main Membrane Processes in Neural Activities 4. Synaptic activity Releases neurotransmitters at presynaptic membrane Produces graded potentials in postsynaptic membrane 5. Information processing Response (integration of stimuli) of postsynaptic cell 12-4 Membrane Potential • The Membrane Potential o Three important concepts 1. The extracellular fluid (ECF) and intracellular fluid (cytosol) differ greatly in ionic composition o Concentration gradient of ions (Na+, K+) 2. Cells have selectively permeable membranes 3. Membrane permeability varies by ion 12-4 Membrane Potential • Passive Forces Acting across the Plasma Membrane o Chemical gradients Concentration gradients (chemical gradient) of ions (Na+, K+) o Electrical gradients Separate charges of positive and negative ions Result in potential difference 12-4 Membrane Potential • Electrical Currents and Resistance o Electrical current Movement of charges to eliminate potential difference o Resistance The amount of current a membrane restricts 12-4 Membrane Potential • The Electrochemical Gradient o For a particular ion (Na+, K+) is: The sum of chemical and electrical forces o Acting on the ion across a plasma membrane A form of potential energy 12-4 Membrane Potential • Equilibrium Potential o The membrane potential at which there is no net movement of a particular ion across the cell membrane o Examples: K+ mV Na+ 66 mV 12-4 Membrane Potential • Active Forces across the Membrane o Sodium–potassium ATPase (exchange pump) Is powered by ATP Carries 3 Na+ out and 2 K+ in Balances passive forces of diffusion Maintains resting potential (70 mV) 12-4 Membrane Potential • The Resting Potential o Because the plasma membrane is highly permeable to potassium ions: The resting potential of approximately 70 mV is fairly close to 90 mV, the equilibrium potential for K+ o The electrochemical gradient for sodium ions is very large, but the membrane’s permeability to these ions is very low Na+ has only a small effect on the normal resting potential, making it just slightly less negative than the equilibrium potential for K + 12-4 Membrane Potential • The Resting Potential o The sodium–potassium exchange pump ejects 3 Na+ ions for every 2 K+ ions that it brings into the cell It serves to stabilize the resting potential when the ratio of Na + entry to K+ loss through passive channels is 3:2 o At the normal resting potential, these passive and active mechanisms are in balance The resting potential varies widely with the type of cell A typical neuron has a resting potential of approximately 70 mV 12-4 Membrane Potential • Changes in the Membrane Potential o Membrane potential rises or falls In response to temporary changes in membrane permeability Resulting from opening or closing specific membrane channels 12-4 Membrane Potential • Sodium and Potassium Channels o Membrane permeability to Na+ and K+ determines membrane potential o They are either passive or active 12-4 Membrane Potential • Passive Channels (Leak Channels) • o Are always open o Permeability changes with conditions Active Channels (Gated Channels) o Open and close in response to stimuli o At resting potential, most gated channels are closed 12-4 Membrane Potential • Three States of Gated Channels 1. Closed, but capable of opening 2. Open (activated) 3. Closed, not capable of opening (inactivated) 12-4 Membrane Potential • Three Classes of Gated Channels 1. Chemically gated channels 2. Voltage-gated channels 3. Mechanically gated channels 12-4 Membrane Potential • Chemically Gated Channels o Open in presence of specific chemicals (e.g., ACh) at a binding site o Found on neuron cell body and dendrites 12-4 Membrane Potential • Voltage-gated Channels o Respond to changes in membrane potential o Have activation gates (open) and inactivation gates (close) o Characteristic of excitable membrane o Found in neural axons, skeletal muscle sarcolemma, cardiac muscle 12-4 Membrane Potential • Mechanically Gated Channels o Respond to membrane distortion o Found in sensory receptors (touch, pressure, vibration) 12-4 Membrane Potential • • Membrane Potential Exists across Plasma Membrane o Because: Cytosol and extracellular fluid have different chemical/ionic balance The plasma membrane is selectively permeable Membrane Potential o Changes with plasma membrane permeability o In response to chemical or physical stimuli 12-4 Membrane Potential • Graded Potentials o Also called local potentials o Changes in membrane potential That cannot spread far from site of stimulation o Any stimulus that opens a gated channel Produces a graded potential 12-4 Membrane Potential • Graded Potentials o The resting state Opening sodium channel produces graded potential o Resting membrane exposed to chemical o Sodium channel opens o Sodium ions enter the cell o Membrane potential rises o Depolarization occurs 12-4 Membrane Potential • Graded Potentials o Depolarization A shift in membrane potential toward 0 mV o Movement of Na+ through channel o Produces local current o Depolarizes nearby plasma membrane (graded potential) o Change in potential is proportional to stimulus 12-4 Membrane Potential • Graded Potentials o Whether depolarizing or hyperpolarizing, share four basic characteristics 1. The membrane potential is most changed at the site of stimulation, and the effect decreases with distance 2. The effect spreads passively, due to local currents 12-4 Membrane Potential • Graded Potentials o Whether depolarizing or hyperpolarizing, share four basic characteristics 3. The graded change in membrane potential may involve either depolarization or hyperpolarization The properties and distribution of the membrane channels involved determine the nature of the change o For example, in a resting membrane, the opening of sodium channels causes depolarization, whereas the opening of potassium channels causes hyperpolarization The change in membrane potential reflects whether positive charges enter or leave the cell 12-4 Membrane Potential • Graded Potentials o Whether depolarizing or hyperpolarizing, share four basic characteristics 4. The stronger the stimulus, the greater the change in the membrane potential and the larger the area affected 12-4 Membrane Potential • Graded Potentials o Repolarization When the stimulus is removed, membrane potential returns to normal o Hyperpolarization Increasing the negativity of the resting potential Result of opening a potassium channel Opposite effect of opening a sodium channel Positive ions move out, not into cell 12-4 Membrane Potential • Graded Potentials o Effects of graded potentials At cell dendrites or cell bodies o Trigger specific cell functions o For example, exocytosis of glandular secretions At motor end plate o Release ACh into synaptic cleft 12-5 Action Potential • Action Potentials o Propagated changes in membrane potential o Affect an entire excitable membrane o Link graded potentials at cell body with motor end plate actions 12-5 Action Potential • Initiating Action Potential o Initial stimulus A graded depolarization of axon hillock large enough (10 to 15 mV) to change resting potential (70 mV) to threshold level of voltage-gated sodium channels (60 to 55 mV) 12-5 Action Potential • Initiating Action Potential o All-or-none principle If a stimulus exceeds threshold amount o The action potential is the same o No matter how large the stimulus Action potential is either triggered, or not 12-5 Action Potential • Four Steps in the Generation of Action Potentials o Step 1: Depolarization to threshold o Step 2: Activation of Na channels o Step 3: Inactivation of Na channels and activation of K channels o Step 4: Return to normal permeability 12-5 Action Potential • • Step 1: Depolarization to Threshold Step 2: Activation of Na Channels o Rapid depolarization o Na+ ions rush into cytoplasm o Inner membrane changes from negative to positive 12-5 Action Potential • Step 3: Inactivation of Na Channels and Activation of K Channels o At 30 mV o Inactivation gates close (Na channel inactivation) o K channels open o Repolarization begins 12-5 Action Potential • Step 4: Return to Normal Permeability o K+ channels begin to close When membrane reaches normal resting potential (70 mV) o K+ channels finish closing Membrane is hyperpolarized to 90 mV Membrane potential returns to resting level Action potential is over 12-5 Action Potential • The Refractory Period o The time period: From beginning of action potential To return to resting state During which membrane will not respond normally to additional stimuli 12-5 Action Potential • • Absolute Refractory Period o Sodium channels open or inactivated o No action potential possible Relative Refractory Period o Membrane potential almost normal o Very large stimulus can initiate action potential 12-5 Action Potential • Powering the Sodium–Potassium Exchange Pump o To maintain concentration gradients of Na+ and K+ over time Requires energy (1 ATP for each 2 K+/3 Na+ exchange) o Without ATP Neurons stop functioning 12-5 Action Potential • Propagation of Action Potentials o Propagation Moves action potentials generated in axon hillock Along entire length of axon o Two methods of propagating action potentials 1. Continuous propagation (unmyelinated axons) 2. Saltatory propagation (myelinated axons) 12-5 Action Potential • Continuous Propagation o Of action potentials along an unmyelinated axon o Affects one segment of axon at a time o Steps in propagation Step 1: Action potential in segment 1 o Depolarizes membrane to 30 mV o Local current Step 2: Depolarizes second segment to threshold o Second segment develops action potential 12-5 Action Potential • Continuous Propagation o Steps in propagation Step 3: First segment enters refractory period Step 4: Local current depolarizes next segment o Cycle repeats Action potential travels in one direction (1 m/sec) 12-5 Action Potential • Saltatory Propagation o Action potential along myelinated axon o Faster and uses less energy than continuous propagation o Myelin insulates axon, prevents continuous propagation o Local current “jumps” from node to node o Depolarization occurs only at nodes 12-6 Axon Diameter and Speed • Axon Diameter and Propagation Speed o Ion movement is related to cytoplasm concentration o Axon diameter affects action potential speed o The larger the diameter, the lower the resistance 12-6 Axon Diameter and Speed • Three Groups of Axons 1. Type A fibers 2. Type B fibers 3. Type C fibers These groups are classified by: o Diameter o Myelination o Speed of action potentials 12-6 Axon Diameter and Speed • Type A Fibers o Myelinated o Large diameter o High speed (140 m/sec) o Carry rapid information to/from CNS o For example, position, balance, touch, and motor impulses 12-6 Axon Diameter and Speed • Type B Fibers o Myelinated o Medium diameter o Medium speed (18 m/sec) o Carry intermediate signals o For example, sensory information, peripheral effectors 12-6 Axon Diameter and Speed • Type C Fibers o Unmyelinated o Small diameter o Slow speed (1 m/sec) o Carry slower information o For example, involuntary muscle, gland controls 12-6 Axon Diameter and Speed • Information o “Information” travels within the nervous system As propagated electrical signals (action potentials) o The most important information (vision, balance, motor commands) Is carried by large-diameter, myelinated axons 12-7 Synapses • Synaptic Activity o Action potentials (nerve impulses) Are transmitted from presynaptic neuron To postsynaptic neuron (or other postsynaptic cell) Across a synapse 12-7 Synapses • Two Types of Synapses 1. Electrical synapses Direct physical contact between cells 2. Chemical synapses Signal transmitted across a gap by chemical neurotransmitters 12-7 Synapses • Electrical Synapses o Are locked together at gap junctions (connexons) o Allow ions to pass between cells o Produce continuous local current and action potential propagation o Are found in areas of brain, eye, ciliary ganglia 12-7 Synapses • Chemical Synapses o Are found in most synapses between neurons and all synapses between neurons and other cells o Cells not in direct contact o Action potential may or may not be propagated to postsynaptic cell, depending on: Amount of neurotransmitter released Sensitivity of postsynaptic cell 12-7 Synapses • Two Classes of Neurotransmitters 1. Excitatory neurotransmitters Cause depolarization of postsynaptic membranes Promote action potentials 2. Inhibitory neurotransmitters Cause hyperpolarization of postsynaptic membranes Suppress action potentials 12-7 Synapses • The Effect of a Neurotransmitter o On a postsynaptic membrane Depends on the receptor Not on the neurotransmitter o For example, acetylcholine (ACh) Usually promotes action potentials But inhibits cardiac neuromuscular junctions 12-7 Synapses • Cholinergic Synapses o Any synapse that releases ACh at: 1. All neuromuscular junctions with skeletal muscle fibers 2. Many synapses in CNS 3. All neuron-to-neuron synapses in PNS 4. All neuromuscular and neuroglandular junctions of ANS parasympathetic division 12-7 Synapses • Events at a Cholinergic Synapse 1. Action potential arrives, depolarizes synaptic terminal 2. Calcium ions enter synaptic terminal, trigger exocytosis of ACh 3. ACh binds to receptors, depolarizes postsynaptic membrane 4. ACh removed by AChE AChE breaks ACh into acetate and choline 12-7 Synapses • Synaptic Delay o A synaptic delay of 0.2–0.5 msec occurs between: Arrival of action potential at synaptic terminal And effect on postsynaptic membrane o Fewer synapses means faster response o Reflexes may involve only one synapse 12-7 Synapses • Synaptic Fatigue o Occurs when neurotransmitter cannot recycle fast enough to meet demands of intense stimuli o Synapse inactive until ACh is replenished 12-8 Neurotransmitters and Neuromodulators • Other Neurotransmitters o At least 50 neurotransmitters other than ACh, including: Biogenic amines Amino acids Neuropeptides Dissolved gases 12-8 Neurotransmitters and Neuromodulators • Important Neurotransmitters o Other than acetylcholine Norepinephrine (NE) Dopamine Serotonin Gamma aminobutyric acid (GABA) 12-8 Neurotransmitters and Neuromodulators • • Norepinephrine (NE) o Released by adrenergic synapses o Excitatory and depolarizing effect o Widely distributed in brain and portions of ANS Dopamine o A CNS neurotransmitter o May be excitatory or inhibitory o Involved in Parkinson’s disease and cocaine use 12-8 Neurotransmitters and Neuromodulators • • Serotonin o A CNS neurotransmitter o Affects attention and emotional states Gamma Aminobutyric Acid (GABA) o Inhibitory effect o Functions in CNS Not well understood 12-8 Neurotransmitters and Neuromodulators • Chemical Synapse o The synaptic terminal releases a neurotransmitter that binds to the postsynaptic plasma membrane o Produces temporary, localized change in permeability or function of postsynaptic cell o Changes affect cell, depending on nature and number of stimulated receptors 12-8 Neurotransmitters and Neuromodulators • Many Drugs o Affect nervous system by stimulating receptors that respond to neurotransmitters o Can have complex effects on perception, motor control, and emotional states 12-8 Neurotransmitters and Neuromodulators • Neuromodulators o Other chemicals released by synaptic terminals o Similar in function to neurotransmitters o Characteristics of neuromodulators Effects are long term, slow to appear Responses involve multiple steps, intermediary compounds Affect presynaptic membrane, postsynaptic membrane, or both Released alone or with a neurotransmitter 12-8 Neurotransmitters and Neuromodulators • • Neuropeptides o Neuromodulators that bind to receptors and activate enzymes Opioids o Neuromodulators in the CNS o Bind to the same receptors as opium or morphine o Relieve pain 12-8 Neurotransmitters and Neuromodulators • Four Classes of Opioids 1. Endorphins 2. Enkephalins 3. Endomorphins 4. Dynorphins 12-8 Neurotransmitters and Neuromodulators • How Neurotransmitters and Neuromodulators Work o Direct effects on membrane channels For example, ACh, glycine, aspartate o Indirect effects via G proteins For example, E, NE, dopamine, histamine, GABA o Indirect effects via intracellular enzymes For example, lipid-soluble gases (NO, CO) 12-8 Neurotransmitters and Neuromodulators • Direct Effects o Ionotropic effects o Open/close gated ion channels 12-8 Neurotransmitters and Neuromodulators • Indirect Effects – G Proteins o Work through second messengers o Enzyme complex that binds GTP o Link between neurotransmitter (first messenger) and second messenger o Activate enzyme adenylyl cyclase Which produces second messenger cyclic-AMP (cAMP) 12-8 Neurotransmitters and Neuromodulators • Indirect Effects – Intracellular Receptors o Lipid-soluble gases (NO, CO) o Bind to enzymes in brain cells