What is Blood? - Lighthouse Christian Academy
advertisement

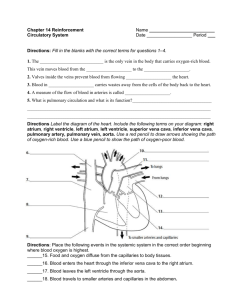
UNIT J: CIRCULATORY SYSTEM (Ch. 13, pp. 226-234 & Ch. 14, pp. 250-251, 254 & Ch. 22, pp. 430-431) J1. Describe and differentiate among the five types of blood vessels. (p. 226-227) J3. Demonstrate safe and correct dissection techniques (Not covered in text) J4. Distinguish between pulmonary and systemic circulation. (p. 234-235) J5. Identify and describe differences in structure and circulation between fetal and adult systems. (Ch. 22 p. 430-431) J2. Identify and give functions for each of the following (p. 234- 235): a) Subclavian arteries and veins b) Jugular veins c) Carotid veins d) Mesenteric arteries e) Anterior and posterior vena cava f) Pulmonary veins and arteries g) Hepatic vein h) Hepatic portal vein i) Renal arteries and veins j) Iliac arteries and veins k) Coronary arteries and veins l) Aorta J6. Demonstrate a knowledge of the path of a blood cell from the aorta through the body and back to the left ventricle. (p. 234-235) J7. List the major components of plasma. (p. 237) J8. Identify and give functions for lymph, capillaries, veins, and nodes. (Ch. 14 p. 250-251) J9. Describe the shape, function, and origin of red blood cells, white blood cells, and platelets. (p. 237-240) J10. Demonstrate the correct use of the compound microscope. (Not covered in text) J11. Explain the roles of antigens and antibodies. (Ch. 14 p. 254) J12. Describe capillary-tissue fluid exchange. (p. 241) Note: J3 and J10 are not examinable on the Provincial Biology 12 exam. •Acclimatize •Afferent arteriole •Agglutination •Anaemia •Anterior vena cava •Antibody •Antigen •Aorta •Aortic arch •Arteriole •Artery •Atrioventricular (AV) valve •Blood clot •Blood pressure •Brachial artery •Capillary •Capillary fluid exchange •Carbaminohemoglobin •Carbonic anhydrase •Carotid arteries •Chemoreceptor •Contrict •coronary •Diastole •Dilate •Ductus arteriosus (arterial duct) •Ductus venosus (venous duct) •Edema •Efferent arteriole •Electrocardiogram (EKG) •Erythrocyte •Fetus •Fibrin •Fibrinogen •Foramen ovale •Hemoglobin •Hepatic portal vein •Hepatic vein •Histamine •Hypertonic •Hypotonic •Iliac artery/vein •Jugular vein •Leucocyte •Lymph •Lymph capillary •Lymph duct •Lymph node •Lymphatic duct •Lymphatic system •Mesenteric artery •Valve •Oxyhemoglobin •Venule •Pacemaker •Villi •Phagocytic •White blood cell •Platelet •Posterior vena cava •Pressure receptor •Prothrombin •Pulmonary artery/vein •Pulmonary circulation •Pulse •Red blood cell •Renal artery/vein •Rhesus (Rh) factor •RhoGAM •Precapillary sphincter muscle •Subclavian artery/vein •Systemic circulation •Systole •Thrombin •Thrombocyte •Thromboplastin •Thymus gland •Umbilical cord •Umbilical artery/vein What is Blood? • Blood is more than just a red liquid that leaks onto your best white shirt when you cut yourself! •How much blood does your heart pump in a day? 7,000 litres •How long do red blood cells live? 4 months •How long does blood last outside your body? 5 days •In a tiny drop of blood, there are 250 million RBC’s, 375,000 WBC’s, & 16 million platelets!!! • Your body has about 5.6 liters of blood, which circulates through the body 3 times every minute. • During an average lifetime, the heart will pump enough blood to fill over 100 fullsized swimming pools. Blood is 55% Plasma (Liquid) The plasma portion of blood is: • 91% Water Maintains blood volume Transports molecules • 7% Proteins (ie: clotting proteins, albumin, immunoglobulins…) • 2 % Salts, gases (O2, CO2), nutrients, wastes, hormones, vitamins, etc… Blood is 45% Formed Elements (Solids) The solid portion of blood is: Red Blood Cells Erythrocytes/corpuscles White Blood Cells Leukocytes Platelets Thrombocytes HOW ARE RBC’s MADE? • When the liver and kidneys detect low levels of oxygen in the body, they release chemicals (REF and GLOBULINS) that stimulate the red bone marrow to increase production of RBC’s. • It takes several weeks to build up the rate of erythrocyte production and this is why it takes a while to become acclimatized when you: a) Visit or move to a higher elevation b) Hemorrage after an accident c) Have sickle cell anaemia Red Blood Cells (RBC’s) • No nuclei • Transport CO2 and O2 and H+ (acts like a buffer) • Bioconcave discs: look like donuts without complete holes! • Live for ~ 120 days (4 months) • Dark purple to bright red • Contain hemoglobin molecules, carbonic anhydrase, and antigens • There are ~800 million oxygen molecules in each RBC • Made in the red bone marrow Erythrocytes Transports oxygen as oxyhemoglobin (bright red) Hb + O2 ------------------------------- HbO2 Hb attaches to oxygen when it’s cool, high pH, and low pressure (ie: at the lungs)! Transports carbon dioxide as carboxyhemoglobin Hb + CO2 ------------------------------- HbCO2 Transports hydrogen ions as reduced hemoglobin (thus acting as a buffer) Hb + H+ ------------------------------- HHb Note: fetal hemoglobin has a greater affinity for oxygen than maternal hemoglobin! White Blood Cells (Leukocytes) • They make histamines, antibodies and hunter killer cells • Fight Infection: the antibodies attach to foreign invaders & the hunter killer cells destroy them. • WBC’s can squeeze out of blood vessels to attack invaders. They have strangely shaped nuclei. They are also made in the red bone marrow Platelets (Thrombocytes) • 150,000-300,000 / mm3 blood • They are just fragments of cells with no nuclei • We produce ~ 200 billion/day • Made in bone marrow Platelets • Aid in blood clotting • Recognize micro tears in blood vessels & bind together to form a blood clot Formation of a Blood Clot Step 1 - A Vessel and Platelets become DAMAGED some way. Step 2 - Platelets release a protein called THROMBOPLASTIN. Step 3 - Thromboplastin changes PROTHROMBIN (a blood protein produced by the liver) into THROMBIN (requires Calcium) Step 4 - Thrombin changes FIBRINOGEN (another blood protein produced by the liver) into FIBRIN (insoluble) Antigens/Antibodies & Blood Type Antigens and Antibodies have different but related functions! Antigen: an identification protein on a RBC • It is a glycoprotein on the RBC membrane • There are two kinds of antigens on human RBC's: A and/or B • Therefore, there are 4 possible blood types: Antigen A Type A blood Antigen B Type B blood Antigens A & B Type AB blood No Antigens Type O blood Antibody: a protein designed to combat any foreign protein • Made by the WBC in the body • Will bind to foreign proteins with foreign antigens • This causes AGGLUTINATION = clumping • WBC’s will then destroy the agglutinated cells Antigen + Antibody (Foreign) (Yours) + Y (Agglutinization) = YYYYY Y YY YY Our blood has antibodies that are opposite to the antigens we have on our RBC’s. WHY? So we don’t attack our own blood! This is what it ‘looks’ like Type A has B antibodies Type B has A antibodies Type O has A and B antibodies Type AB has No antibodies • Therefore blood transfusions are tricky: introducing foreign antigens can lead to… DEATH Note: Antibodies are REMOVED from donated blood – they cannot cause agglutination Blood donor Blood Type A B AB O A B AB O yes clumps clumps yes clumps yes clumps yes yes clumps yes clumps yes clumps yes yes The Rh factor is another antigen that may be present on the RBC. The presence of this antigen plays a role in childbirth. •If you are Rh+ you have the antigen and don’t have the ‘D’ antibodies. (85% of Caucasians are Rh+) Rh + NO ANTIBODIES •If you are Rh – you don’t have the antigen. You don’t normally have the ‘D’ antibodies, but can make them if you are exposed to Rh antigens. Rh - HAS ANTIBODIES, BUT ONLY WHEN EXPOSED TO Rh+ BLOOD •If Rh antigens are mixed with Rh antibodies, agglutination occurs. Donor Rh + Rh - Recipient Anti-Rh Antibodies in Recipient's Blood Rh - Will Produce anti-Rh Antibodies Rh + Will Not Produce anti-Rh Antibodies Rh Blood Rh + Blood WHY ELSE IS THIS IMPORTANT? •If an Rh- mother has an Rh+ baby, complications can occur with a second pregnancy. •Normally, the mother / fetal blood does not mix or cross the placenta. •However, at birth, there is usually some mixing, and the mother will begin to produce Rh antibodies in response to the Rh antigens on the baby's Rh+ RBC's. •There is no danger for either the mother or the first baby. BUT…If the mother becomes pregnant with another Rh+ baby, the mother’s antibodies (made during the birth of the 1st child) are small, and can cross the placenta. These antibodies will agglutinate the baby's blood. This will cause the baby to die / be still born (Erythroblastosis). How can this be prevented? When the first Rh+ baby is born, doctors can destroy the Rh+ blood cells in the mother's plasma before the mother has time to make the Rh antibodies. An injection of Rh immune globulin injection (RhoGAM) does this. CIRCULATION Blood and Blood Vessels Blood Vessels – The 5 Main Types 1. Arteries 2. Arterioles 3. Capillaries 4. Venules 5. Veins http://www.youtube.com/watch?v=PgI80Ue-AMo • The aorta, the largest artery in the body, is almost the diameter of a garden hose. • The aorta in a blue whale is so big, you could swim down it!!! • Capillaries, on the other hand, are so small that it takes ten of them to equal the thickness of a human hair. • One pound of excess fat adds approximately 200 miles of extra capillaries. This increases BP! •If you stretched your veins out, and hooked them all together, they would go around the world 2 times!! 1) Arteries Function • Transport blood AWAY from the heart Structure • Thick, elastic walls Location • Usually deep, along bones • This protects them from injury and temperature loss. Notes • Walls can expand • Arteries have very high Blood Pressure • Expansion is the “pulse” we feel Arteries of the Human Body 2) Arterioles Function • Control blood flow to capillaries Structure • Smaller in diameter than arteries, thinner walls • Have pre-capillary sphincters Location • Leading towards all capillaries Notes • Blood Pressure > Osmotic Pressure • Regulate blood pressure with pre-capillary sphincter muscles: can dilate or constrict to increase Afferent = incoming Efferent = outgoing or decrease blood flow to a particular capillary bed. 3) Capillaries Function • Connect arteries to veins • Site of “capillary-fluid exchange” Structure • Very thin walls (1 cell thick) Location • Everywhere; within a few cells of each other O2 CO2 Capillary-Fluid Exchange on Arteriole Side A. Arteriole Side • Blood pressure @ arteriole side = 40 mmHg • Osmotic pressure = 25 mmHg • Net Blood pressure (15mmHg) forces water out of the blood into the interstitial fluid • Water carries with it the O2 and nutrients • Because there is more O2 and nutrients in interstitial fluid, it diffuses into body cells • The large things (ie: RBC, WBC, platelets, blood proteins) stay in the capillary because they are too big to leave. • Because most of the water has left, the blood becomes very hyperosmotic (concentrated) • The venule side of the capillary is therefore under great osmotic pressure to draw water back into the blood. VIDEO: http://www.youtube.com/watch?v=B658Yn3INYc Capillary-Fluid Exchange on Venule Side B. Venule Side • Osmotic pressure @ venule side = 25 mmHg • Blood pressure = 10 mmHg • Blood very concentrated (has little water) • Net osmotic pressure (15mmHg) forces water back into the blood • Water carries with it CO2 and metabolic wastes (urea) • These are carried to the kidneys and other excretory organs to be removed. 4) Venules Function • Drain blood from capillaries Structure • Thinner walls than veins Location • Often near the surface Notes • Join to form veins • Osmotic Pressure > Blood Pressure • The end result is no change in blood volume (ie: no volume is lost in the exchange) 5) Veins Function • Transport blood TOWARDS the heart Structure • Inelastic walls, contain one-way valves Location • Often near to surface Notes • Blood pressure & velocity is much lower than in arteries • Valves prevent blood from flowing backwards • Surrounded by skeletal muscle, “squeezes” blood along Veins of the Human Body How Does It All Fit Together? • Arteries: – Carry blood away from the heart – Elastic • Capillaries: – Very thin tubes – Connect arteries to veins – Can close down or open up to regulate blood flow – GAS EXCHANGE • Veins: – Bring blood towards the heart – Have valves to stop blood from moving backwards The Circulatory System is organized into two parts: Systemic Circulation: system of blood vessels that delivers oxygenated blood to body systems. Pulmonary Circulation: system of blood vessels that delivers deoxygenated blood to the lungs to be replenished with oxygen What is the big deal? The systemic arteries carry oxygenated blood. The pulmonary arteries carry deoxygenated blood. PULMONARY ARTERY VENA CAVA PULMONARY VEIN AORTA Pulmonary and Systemic Circulation SYSTEMIC CIRCULATION Pulmonary and Systemic Circulation SYSTEMIC CIRCULATION Pulmonary and Systemic Circulation PULMONARY CIRCULATION Pulmonary and Systemic Circulation PULMONARY CIRCULATION B. The Major Blood Vessels of the Body Cranial vein VENA CAVA Cranial artery AORTA Brachial artery 1. Aorta • Biggest Artery • Carries O2 rich blood from left ventricle to body systems • Loops over top of heart, creating the AORTIC ARCH • Goes down inside of backbone = DORSAL AORTA • Smaller arteries branch off to ‘feed’ the body cells 2. Coronary Arteries/Veins •Very first branch off the aortic arch •Blood vessels that “FEED” the heart muscle Why can’t the heart just get its oxygen and nutrients from the blood that passes through it? 3. Carotid Arteries • Branch off the aortic arch to take the blood to the head • Supply blood to brain = highly specialized: CHEMORECEPTORS detect oxygen content PRESSURE RECEPTORS detect changes in blood pressure • Reasonably close to the surface, pulse can be found in neck 4. Jugular Veins • Take blood out of head region to the anterior vena cava • These veins DO NOT contain any valves! • Blood flows down them because of gravity only Try standing on your head for a while! 5. Subclavian Arteries/Veins • Arteries branch off of aorta and travel under the clavicle • Branch to feed chest wall/arms (via brachial arteries) • Note For Later: Lymphatic Ducts join circulatory system right before the subclavian veins meet up with the anterior vena cava 6. Mesenteric Arteries • Branch off from the dorsal aorta • Go to the intestines • Branch into capillaries of the intestinal villi • Pick up the newly digested nutrients (glucose, amino acids and nucleotides) Mesentary Mesenteric Arteries 7. Hepatic Portal Vein • Hepatic = Liver; Portal = capillary bed on either end • This vein transports blood rich in nutrients directly from the intestines to the liver Remember the liver functions?? • Significant functions for the circulatory system: regulation of blood [glucose] Destroys old RBC’s detoxification of blood HEPATIC PORTAL VEIN 8. Hepatic Veins • Carries the blood from liver to posterior vena cava 9. Renal Arteries/Veins • Renal arteries branch off dorsal aorta and bring blood to kidneys • Renal veins take blood from kidneys to posterior vena cava 10. Iliac Arteries/Veins • Dorsal aorta branches into two iliac arteries in the pelvic area • One iliac artery goes down each leg • Femoral artery branches off iliac artery to large quadricep muscle • Iliac veins return blood to posterior vena cava 11. Pulmonary Arteries/Veins • deO2 blood collected from the body is pumped into the pulmonary artery from the right ventricle • Pulmonary artery brings deO2 blood to lungs • Blood picks up O2 in the alveoli of lungs • Pulmonary vein takes high O2 blood back to left atrium of heart Pulmonary Artery Pulmonary Vein Part D. The Lymphatic System “A system of thinwalled vessels with valves that drain fluids from bodies tissue spaces” Functions of the Lymphatic System 1. Take up excessive tissue fluids 2. Transport fatty acids and glycerol (from intestines to subclavian vein) 3. Fight infection (lymphocytes) 4. Trap and remove cellular debris Structures of the Lymphatic System 1. Lymph Ducts and Capillaries • Drain and collect excess fluids from tissues • Take fluids to nodes to be cleaned • Cleansed lymph travels through lymph ducts to the subclavian vein where they are dumped into the anterior vena cava 2. Lymph Nodes • Remove debris from lymph = ‘cleanse’ lymph • Contain Phagocytic Lymphocytes • White Blood Cells make antibodies and attack invaders 3. Lacteals • absorb/transport fatty acids & glycerol in the villi of the small intestine. 4. Other Lymphoid Organs • Tonsils, Appendix, Spleen, and Thymus gland Please see attached “SCHEMATIC DIAGRAM” worksheet NOW! •A fetus does not use its lungs. •The fetus receives its O2 blood from the placenta, not its lungs. •To do this, there are four features in the fetus not present in the adult. •This is an opening between the Left and Right atria •It is covered by a flap that acts as a valve •It allows the blood to bypass the lungs •It reroutes most of the blood from the right atrium into the left atrium. •This is a small arterial connection, like a shunt. •Between the pulmonary artery and the aorta. •It further allows blood to bypass the lungs. •The Umbilical Cord has three blood vessels traveling through it. •The largest one is the umbilical vein, which transports blood with oxygen and nutrients into the fetus. •The other two are the umbilical arteries, which branch off of the iliac arteries in the fetus, and take “spent” (wastes and CO2) blood back into the mother via the placenta. •This blood vessel connects the umbilical vein to the vena cava. •The O2 blood from the umbilical vein mixes with deO2 blood in the vena cava. •The ductus venosus bypasses the liver and this blood is sent directly to the heart. •Blood will go to the liver eventually, but not until it has reached the hepatic portal vein. •This is why the fetus is so susceptible to toxins in blood. The First Breath: the lungs are filled with air instead of fluid and higher oxygen levels in the blood and alveoli results in an increase in pulmonary blood flow. Anatomical Changes: The placenta is removed from circulation. The foramen ovale, ductus venosus, and ductus arteriosus close.