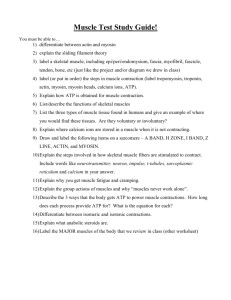
I. Microanatomy of a Skeletal Muscle Fiber
advertisement

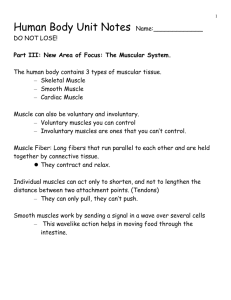
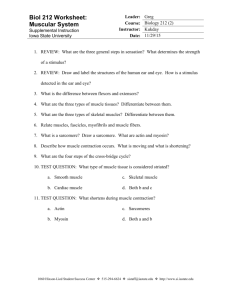
UNIT 5 Notes Title: Introduction to the Muscular System I. Muscular System A. There are four characteristics associated with muscle tissue, 1. Excitability - tissues can receive & respond to stimulation 2. Contractility - tissues can shorten & thicken 3. Extensibility - tissues can lengthen 4. Elasticity - after contracting or lengthening tissues always want to return to their resting state B. Characteristic of muscles tissue enable it to perform some important functions including: 1. Movement - both voluntary & involuntary 2. Maintaining posture 3. Supporting soft tissues within body cavities 4. Guarding entrances & exits of the body 5. Maintaining body temperature C. Types of muscle tissue: 1. Skeletal muscle tissue a. Associated with and attached to the skeleton b. Under our conscious (voluntary) control c. Cells are long, cylindrical, striated, and multinucleated 2. Cardiac muscle tissue a. Makes up myocardium of heart b. Unconsciously (involuntarily) controlled by pacemaker cells c. Cells are short, branching, striated and have a single nucleus d. Cells connect to each other at intercalated discs 3. Smooth (visceral) muscle tissue a. Makes up walls of organs and blood vessels b. Unconsciously (involuntarily) controlled by pacesetter cells or by hormonal or environmental conditions c. Cells are short, spindle-shaped, non-striated and have a single nucleus d. Tissue is extremely extensible while still retaining ability to contract II. Gross Anatomy of Skeletal Muscles A. Three fibrous layers of connective tissue make up each muscle 1. Epimysium a. Outer layer of whole muscle 2. Perimysium a. Inner covering that divides muscle into bundles called fascicles; contains vessels and nerves 3. Endomysium a. Covers a single cell (a muscle fiber) contains stem cells to repair damaged muscle B. Tendons (or aponeurosis) 1. Bundles at the ends of each muscle made of fibers of all three layers that attach muscle to bone Title: Muscle Anatomy and Terminology I. Basic Muscle Anatomy A. Origins, Insertions, and Actions 1. Origin a. Muscle attachment that remains fixed 2. Insertion a. Muscle attachment that moves 3. Action a. The joint movement a muscle produces II. Types of Muscles A. Muscles in the body rarely work alone and are usually arranged in groups surrounding a joint to allow the limb to move through the joint’s range of motion 1. Agonists – These muscles cause the movement to occur. They create the normal range of movement in a joint by contracting. a. Agonists are also referred to as prime movers since they are the muscles that are primarily responsible for generating the movement. 2. Antagonists – These muscles act in opposition to the movement generated by the agonists and are responsible for returning a limb to its initial position. 3. Synergists – These muscles perform, or assist in performing, the same set of joint motion as the agonists. a. Synergists are sometimes referred to as neutralizers because they help cancel out or neutralize extra motion from the agonists to make sure that the force generated works within the desired plane of motion. 4. Fixators – These muscles immobilize the origin of a prime movers so that all tension is exerted at the insertion. These muscles also provide the necessary support to assist in holding the rest of the body in place while the movement occurs. a. Fixators are also sometimes called stabilizers. III. Muscle Terminology A. Muscle location – bones with which 1. Rectus (straight) 2. Transverse (across) muscle associates. 1. Pectoralis (chest) 3. Oblique (diagonally) 2. Gluteus (buttock or rump) 4. Orbicularis (circular). 3. Brachii (arm) E. Origin Number 4. Supra- (above) 1. Biceps (two) 5. Infra- (below) 2. Triceps (three) 6. Sub- (under or beneath) 3. Quadriceps (four) 7. Lateralis (lateral) F. Origin and insertion location B. Relative muscle size: 1. Sternocleidomastoideus (origin on 1. Maximus (largest) the sternum and clavicle, insertion 2. Minimus (smallest) on the mastoid process) 3. Longus (long) 2. Brachioradialis (origin on the 4. Bravis (short) brachium or arm, insertion on the 5. Vastus (huge) radius). C. Muscle shape: G. Muscles action 1. Deltoid (triangular) 1. Abductor (to abduct a structure) 2. Rhomboid (like a rhombus with 2. Adductor (to adduct a structure) 3. Flexor (to flex a structure) equal and parallel sides) 3. Latissimus (wide) 4. Extensor (to extend a structure) 4. Teres (round) 5. Elevator (to lift or elevate a 5. Trapezius (like a trapezoid, a fourstructure) 6. Masseter (a chewer) sided figure with two sides parallel). D. Direction of muscle fibers – in reference to the midline of the body or longitudinal axis of the limb bone: Title: Skeletal Muscle Microanatomy I. Microanatomy of a Skeletal Muscle Fiber A. Compared to “typical” cells skeletal muscles cells are 1. Enormous - up to 60 cm/24 in long! 2. Multinucleated - contain 100s of nuclei 3. Unique cell parts and organelles such as a. Sarcolemma - muscle cell membrane b. Sarcoplasm - muscle cell cytoplasm c. Sarcoplasmic reticulum (SR) – like smooth ER d. Transverse tubules (T tubules) – tubes filled with extracellular fluid forming passageways through muscle fiber to coordinate muscle contractions e. Myofibrils (contraction organelle) - cylindrical structures encircled by T tubules f. Myofilaments - thick (myosin) and thin (actin) protein bundles that make up myofibrils B. Sarcomeres - the smallest functional unit of muscle fiber, made of repeating thick and thin myofilaments that are responsible for muscle contraction 1. Arrangement of filaments produces a banded appearance a. Z lines - boundary of each sarcomere where thin filaments attach to proteins b. M line – made of proteins that connect the middle portion of the thick filaments together c. A band – is darker and contains the thick filaments d. I band – is lighter between the A band and Z line only thin filaments e. H zone - light region inside A band only thick filaments with no thin filament present. II. Thick and Thin Filaments A. Thin filaments 1. Twisted strands of actin molecules 2. Each actin has an active site to bind to myosin 3. At rest, active sites are covered by protein strands of tropomyosin 4. Troponin molecules hold the tropomyosin strands in place B. Thick filaments 1. Composed of myosin molecules 2. Each with a tail and globular head 3. Heads point away from the center of a sarcomere 4. Myosin heads attach to actin molecules during a contraction 5. Troponin blocks this from happening unless it is “unlocked” by calcium III. Sliding Filament Theory A. Myosin heads attach to actin molecules (at binding (active) site) B. Myosin “pulls” on actin, causing thin myofilaments to slide across thick myofilaments toward the center of the sarcomere C. Sarcomere shortens, I bands get smaller, H zone gets smaller & zone of overlap increases D. As sarcomeres shorten, myofibrils shorten. As myofibrils shorten, so does the muscle fiber E. Once a muscle fiber begins to contract it contracts maximally 1. This is known as the “all or none” principle Title: Muscle Contractions I. Physiology of skeletal muscle contraction A. Skeletal muscles require stimulation from the nervous system in order to contract B. Motor neurons are the cells that cause muscle fibers to contract II. Stage 1: Brain to Muscle (Location: Neuromuscular junction) A. An action potential (AP), an electrical impulse, is generated in the primary motor cortex of the brain at a specific location associated with part of the body you wish to move (see primary motor cortex homonuculus) B. The AP travels down the axon of the motor neuron in the brain and to the spinal cord where it triggers an AP in another motor neuron that takes the signal to the specific muscle(s) that control movements you wish to make. C. When the AP reaches the end of the neuron (called the end bulbs or synaptic terminals) it causes vesicles filled with a neurotransmitter (chemical messengers) to fuse with the membrane and release the neurotransmitter Acetylcholine (Ach) into the space (synaptic cleft) between the neuron and the muscle. D. Ach diffuses across the synaptic cleft and binds to Ach receptors on a special location on the muscle called the motor end plate E. The binding of Ach to its receptors causes a new AP to be generated along the muscle cell membrane. F. Immediately after it binds to its receptors and triggers an AP, Ach will be broken down by Acetylcholinesterase (AchE) – an enzyme present in the synaptic cleft to prevent further contractions. III. Stage 2: Muscle Contraction (Location: inside sarcomeres of skeletal muscles) A. Once an action potential (AP) is generated at the motor end plate it will spread like an electrical currant along the sarcolemma of the muscle fiber B. The AP will also spread into the T-tubules exciting the terminal cisternae (the storage place of calcium in muscles) of the sarcoplasmic reticula C. This causes calcium (Ca2+) gates in the SR to open, allowing Ca2+ to diffuse into the sarcoplasm D. Calcium will bind to troponin causing it to change its shape. This then pulls tropomyosin away from the active sites of the actin molecules. E. The exposure of the active sites allow myosin “heads” to bind to actin (cross-bridge) and contract to pull the actin toward the M line. This is called the “power stroke”. F. Myosin binds to ATP and releases actin to repeat the power stroke process and shortening the sarcomere. This continues as long as Ca2+ and ATP are available. IV. Stage 3: Muscle Relaxation/Release (Location: inside sarcomeres of skeletal muscles) A. If no more APs arrive from the motor neuron, no more Ach will be released. B. AchE will remove any remaining Ach from the motor end plate, and AP transmission on the muscle fiber will end C. Ca+2 gates in the SR will close and Ca2+ will be actively transported back into the SR. D. With Ca2+ removed from the sarcoplasm and from troponin, tropomyosin will re-cover the active sites of actin and no more cross-bridge interactions can form. E. Actin passively slides back to its resting state. V. Rigor Mortis A. When all an individual’s muscles contract causing the whole body to be stiff shortly after death. 1. Onset is around 3 hours postmortem and can lasting up to 24 hours postmortem 2. Loss of circulation deprives skeletal muscle fibers of O2 and nutrients for making ATP 3. Ca2+ ions leak out of the SR, exposes all active sites causing myosin to bind to actin 4. Without ATP to remove Ca2+ ions, the myosin remains contracted to actin 5. Eventual enzymes are released to break down the myofilaments and stop contraction VI. Botulin Toxin A. A very toxic poison that prevents Ach from being released causing muscle paralysis Title: Muscle Mechanics I. Skeletal Muscle Mechanics A. Muscle tension - the pulling force on the tendons that muscle cells generate when contracting 1. Tension pulls the object toward the tension 2. Amount of tension depends on the number of muscle fibers activated and the frequency of stimulations from action potentials B. Muscle twitch - A brief contraction-relaxation response to a single action potential 1. Latent period – no tension yet but action potential sweeps across the muscle cell and calcium is released 2. Contraction phase - tension rises to a peak as myosin binds to actin 3. Relaxation phase – muscle tension falls as calcium levels drop and active sites are covered C. The Frequency of Muscle Fiber Simulation 1. Summation - Addition of twitch tension when a stimulus is applied before tension has completely relaxed 2. Incomplete tetanus – Tension peaks and falls repeatedly and builds up beyond twitch tension (all normal muscle contractions involve incomplete tetanus) 3. Complete tetanus – Tension is steady (no relaxation phase) and largest if stimuli arrive at very high rates; this is maximum muscle tension (not very frequent) D. Motor Unit 1. Skeletal muscles are made up of thousands of muscle fibers 2. A motor neuron and all the muscle fibers it stimulates are called a motor unit a. It may directly control a few fibers or hundreds to thousands of muscle fibers 3. All of the muscle fibers controlled by a single motor neuron contract together. a. The size of the motor unit determines how fine the control of the movement can be – i. small motor units precise control (e.g. eye muscles) ii. large motor units gross control (e.g. leg muscles) 4. Recruitment - the ability to activate more motor units as more force (tension) needs to be generated 5. Muscle Tone – a measure of a muscle’s resistance to stretching while in a resting state a. produced by a low level of involuntary motor neuron activity. b. function is to stabilize bones, joints and prevent atrophy (muscle breakdown) 6. There are always some motor units active even at rest. This creates a resting tension know as muscle tone II. Types of Muscle Contractions A. Isometric Contraction 1. No change in length of muscle even as tension increased 2. The length of the muscle stays constant (iso = same, metric = length) during a “contraction”. Necessary in everyday life to counteract effects of gravity (keeping head up) 3. Examples: holding a baby at arms length, pushing against a closed door B. Isotonic Contraction 1. As tension increases (more motor units recruited) length of the muscle changes usually resulting in movement of a joint 2. The tension (load) on a muscle stays constant (iso = same, tonic = tension) during a movement 3. Examples: lifting a baby, picking up an object, walking 4. Two types a. Concentric – muscle contracts and distance between origin and insertion decreases b. Eccentric – muscle contracts and distance between origin and insertion increases Title: Muscle Energetics I. Energetics of Muscle Mechanics A. ATP and Creatine Phosphate Reserves 1. Muscle contractions consume tons of ATP!!! 2. An active muscle fiber may require 600 trillion ATP a second! 3. ATP transfer energy directly to actin/myosin cross-bridges and calcium pumping 4. When more ATP is produced than needed in a resting muscle it is converted to Creatine Phosphate(CP), which is capable of being stored in muscles 5. When ATP is needed CP stores are regenerated into ATP 6. CP levels greatly exceed ATP levels in resting muscles B. ATP Generation 1. Light activity a. Aerobic metabolism of fatty acids b. Storage of glucose as glycogen (a fat storage form of glucose) 2. Moderate activity a. Breakdown of glycogen to glucose b. Glycolysis of glucose and cellular respiration (Krebs Cycle and ETC) 3. Peak activity a. Anaerobic breakdown of glucose (lactic acid fermentation) b. Produces of lactic acid C. Muscle Fatigue 1. When a muscle loses ability to contract due to a low pH (lactic acid buildup), low ATP levels, or other problems D. Recovery Period 1. Time after muscle activity required to restore pre-exertion conditions 2. Oxygen debt is the amount of excess oxygen used during the recovery period to restore the muscle to normal levels II. Two Types of Skeletal Muscle Fibers A. Red fibers (slow twitch, low threshold to contract) 1. Smaller diameter, rich capillary supply, many mitochondria, contain red pigment myoglobin (a strong oxygen-binding protein) 2. Produce slow, steady contractions that resist fatigue 3. Produce small amounts of tension 4. Use aerobic metabolism to get ATP 5. Found in high amounts in posture muscles (neck, back) and limbs B. White fibers (fast twitch, high threshold to contract) 1. Large diameter, abundant myofibril, high glycogen levels, few mitochondria, little myoglobin 2. Produce powerful, brief contractions that can react quickly but fatigue easily 3. Produce large amounts of tension 4. Uses anaerobic metabolism to get ATP 5. Found in high amounts in eye muscles and muscles to move fingers C. Intermediate fibers (fast-twitch fatigue resistant) 1. A mix between white and red fibers 2. Most of our body muscles contain this type III. Physical Conditioning A. Anaerobic endurance 1. Time over which a muscle can contract effectively under anaerobic conditions B. Hypertrophy 1. Increase in muscle bulk. Can result from anaerobic training C. Aerobic endurance 1. Time a muscle can contract supported by mitochondria