CHAPTER 5 “The Integumentary System”
advertisement

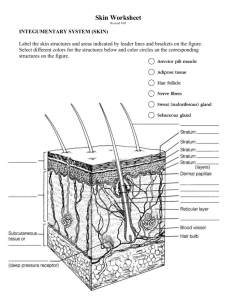
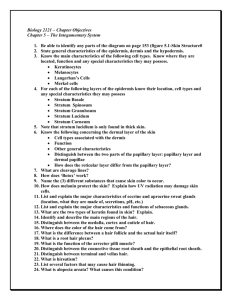
CHAPTER 5 “The Integumentary System” COURSE OBJECTIVES: 1. List functions of the integumentary system 2. Identify layers and sublayers of the skin 3. Identify accessory structures of the skin 4. Explain variations in skin pigmentation Defined • The Integumentary system is defined as the skin and all associated structures (hair, nails, and glands). • Consists of an epidermis and dermis. • The hypodermis is generally not considered to be part of the skin proper. Integumentary system Functions of the integument 1. Body temperature regulation - via perspiration and vasodilation or vasoconstriction of skin blood vessels. 2. Protection - barrier against foreign material entering body and loss of fluids and electrolytes through skin. 3. Stimuli perception – via nerve endings and receptors sensing temperature, pressure, pain, etc. 4. Excretion of waste materials – removal of urea, amino acids, electrolytes, sugars, etc. 5. Synthesis of Vitamin D3 – precursor molecules in skin are stimulated by sunlight to begin production of calcitrol. Epidermis (Epithelial layer) • Keratinized stratified squamous epithelium • Contains 4 distinct cell types: -Keratinocytes; melanocytes; Merckel cells and Langerhans cells • Is avascular and receives nutrients from dermis • Made up of 4 to 5 distinct layers; stratum basale; stratum spinosum; stratum granulosum; stratum lucidum and the stratum corneum. The stratum lucidum is present only on palms and soles . Epidermis (Epithelial layers) Cells of the skin • Keratinocytes- most predominant cell in skin; produce keratin, a tough fibrous protein that gives skin its protective properties. Also produce antibodies and enzymes that detoxify harmful chemicals and agents that may enter the skin. • Melanocytes- spider shaped cells that produce “melanin” a dark pigment in skin. • Merkel cells- hemisphere shaped cells that are sensory touch receptors. • Langerhans cells- “star shaped” macrophage phagocytic cells in skin: eat foreign proteins. Skin cells shapes Epidermal layer # 1 • Stratum basale: deepest layer of epidermis firmly attached to the dermis. – Also known as Stratum germinativum. – Consists of a single layer of stem cells representing young keratinocytes and exhibits a lot of mitotic activity. – Layer also contains Merckel cells and spider shaped melanocytes (10-25%). Epidermal layer # 2 • Stratum spinosum (spiny layer) – Several layers thick; Thickest layer in thin skin. – Derives name from many spiny keratinocyets scattered through this layer. Spiny appearance is due to fixation artifact and attached desmosomes. – Langerhans cells present act as part of immune system to scavenge foreign proteins that invade epidermis. Epidermal layer # 3 • Stratum granulosum – Consists of 1-5 layers of keratinocytes – Also contains keratinohyaline granules and lamellated granules. Former cells form keratin in more superficial layers of epidermis and latter cells form a glycolipid layer which acts as waterproofing. – Receives nutrient from capillaries in dermal layer. – Layers above here are dead keratinized cells Epidermal layer # 4 Found in thick skin only • Stratum lucidum (clear layer) – Occurs only in thick skin of palms and soles – Does not occur in thin skin – Consists of a few layers of flat dead keratinocytes that have a transparent appearance. Thick skin versus Thin skin Epidermal layer # 5 • Stratum corneum (Horny layer) – Most superficial layer of epidermis – Many cell layers thick – Consists of dead keratinized cells that are filled with keratin and no longer have nuclei and organelles. – Is the layer that is shed as dandruff flakes from scalp – Is beauty really only skin deep?? – If so than what we are looking at is dead tissue – Average person sheds ~ 40 lbs. in a lifetime Dermis (fibrous connective tissue) • Second layer of skin • Is a strong flexible dense irregular connective tissue containing mast cells, macrophages, fibroblasts, and scattered leukocytes. • Also contains elastic, reticular and collagen fibers • Dermis is what binds the body together. • Richly supplied by nerves and blood vessels. • Consists of 2 layers: Papillary and Reticular Dermal layers Papillary layer – Most superficial layer of dermis consists of areolar CT with collagen and elastic fibers. – Dermal papillae form dermal ridges that form our fingerprints, palm prints and footprints. Reticular layer - 80 % of dermis - consist of dense irregular CT - named for its network (reticulum) of collagen fibers Integumentary layers Dermal sensory receptors • Free nerve endings sensitive to temperature, pain (nociceptors) and pressure • Meissner’s corpuscles sensitive to light pressure, discriminative touch, low vibrations. • Pacinian corpuscles sensitive to deep pressure, high frequency vibration. Adapt rapidly. Hypodermis (fatty layer) • Not actually a layer of the skin • Also known as a subcutaneous layer or superficial fascia. • Deep to dermis consists of adipose and areolar connective tissue. • Anchors skin to deeper structures (mostly muscle) but loose enough to allow skin to be flexible and movable. • Acts as a good body insulator Skin Color • Three pigments contribute to skin color: – Melanin: produced by melanocytes but accumulates in keratinocytes of stratum basale and stratum spinosum. • Two forms of melanin: eumelanin and pheomelanin – Carotene: yellow pigment most conspicuous in heel calluses and corns in stratum corneum. – Hemoglobin: red pigment in rbc’s, imparts red color to skin through blood vessels Skin accessories • Glands: sebaceous and sweat (sudoriferous glands), and ceruminous glands • Hair (pilus/pili) derived from keratin • Nails are produced from keratin Skin glands • Sebaceous glands – produce an oily secretion called sebum. Usually open into a hair follicle. – Their secretion is holocrine – Sebum keeps skin moist and flexible and gives hair a sheen • Sudoriferous “sweat” glands – are of 2 kinds; apocrine and merocrine. – Merocrine: most numerous; produce watery perspiration for cooling body; most abundant on palms, soles and forehead. – Apocrine: present in groin, axilla, anal, areola, and beard regions; ducts open into hair follicle; sweat is thicker milkier due to fatty acids. Strong odor is due to bacterial decay. • Scent glands that respond to stress and sexual stimulation • Become fully functional at puberty. • Open into hair follicles Skin glands • Ceruminous glands – found only in the external auditory canal. – Secretion is called cerumen which is waxy and has a viscous texture and bitter taste. It repels insects and kills bacteria and waterproofs the eardrum. – Are modified sweat glands “apocrine”. • Mammary glands – specialized sweat glands that produce milk in pregnant females. Hair Hair (pilus) characteristics Hair is made of dead keratinized cells and consists of a bulb, root and shaft and grows within a follicle. Arrector pili muscle (sm. m.)- under sympathetic control • Three concentric layers: 1. medulla = central core 2. cortex = several layers of flattened cells; 3. cuticle = single layer of cells that overlap like shingle forming outermost portion gives hair strength and keeps it from matting Three kinds of hair • Lanugo – fine downy hair present in fetus and replaced at birth. • Vellus – fine unpigmented hair. Approx 2/3 of hair in ♀ and 1/10 in ♂ and all hair in children, except eyebrows, eyelashes and scalp hair. • Terminal - longer, coarser, and pigmented. Forms eyebrows, eyelashes, scalp and pubic, axillary, and facial hair after puberty. Hair texture and color • Shaft shape on x-section determines hair type: oval = wavy hair; flat ribbon-like = kinky/ curly; round = straight hair. • Hair color is due to amounts of melanin in cortex: – Brown and black have large amounts of eumelanin – Red has less eumelanin but more pheomelanin. – Blond has intermediate amount of pheomelanin but little eumelanin. – Gray or white is due to absence of melanin and air in the medulla. Nails Nail anatomy • Nails are a modification of stratum corneum composed of very thin dead scaly cells closely packed together and filled with parallel keratin fibers. • Claws and hooves in most mammals; nails are a distinguishing characteristic of primates. • Serve to allow us to pick up very small objects and manipulate as well as being used for tearing, digging and scratching. Nail anatomy • Nail matrix- growth zone at proximal border concealed under skin of nail plate. • Nail plate- visible portion of nail covering tip of finger or toe. Consists of root, body and free edge of nail. • Nail groove and fold- lateral edge of nail plate. • Free edge- distal most edge of nail plate over tip of finger or toe. • Eponichium- “cuticle” is dead epidermal tissue covering proximal end of nail. • Lunule- thick white crescent shaped area distal to eponichium. Obscures dermal vessels below. Injury and Repair • • The skin can regenerate after injury. After injury there are four stages of healing: 1. 2. 3. 4. After injury bleeding usually occurs into the site. Clot or scab forms at the surface of the epidermis. Granulation occurs and the clot dissolves. Scar tissue forms and the extent of scarring depends on the degree of the injury. Burns • Burns to the skin are graded in degrees: – First degree involves superficial layers of the epidermis and will be inflamed and tender – Second degree penetrate deeper and may enter reticular layer of dermis leading to blisters and pain. – Third degree kill all epidermal and dermal layers and may penetrate the hypodermis. Such injuries are very painful and can be life threatening if injury is very extensive. Burns • First degree = superficial as in sun burns • Second degree = blisters and pain into dermis • Third degree = full thickness slough of tissue Skin cancers Aging and the skin • As we get older, our skin takes on significant changes. – It tends to get thinner and drier as glandular function decreases. – Skin injuries and infections increase and immune function decreases. – Muscles become weaker and the dermis sags and becomes more wrinkly. – Elastic fiber network decreases causing the skin to become less resilient.