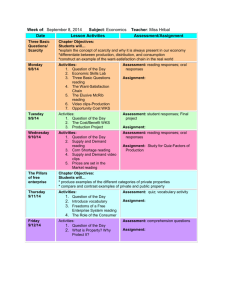
Facial Rashes
advertisement
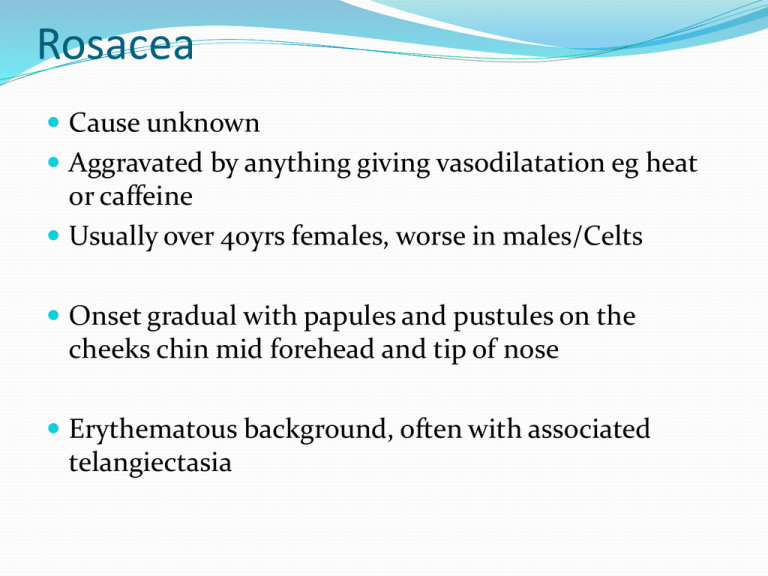
Rosacea Cause unknown Aggravated by anything giving vasodilatation eg heat or caffeine Usually over 40yrs females, worse in males/Celts Onset gradual with papules and pustules on the cheeks chin mid forehead and tip of nose Erythematous background, often with associated telangiectasia Distribution Papules/pustules/erythema Nasolabial sparing Rhinophyma Can be unilateral Subtle telangiectasiae Opthalmological problems Up to 5% rosacea patients Blepharoconjunctivitis Lid hygeine, oral oxytetracycline for 6 wks if severe Dry eyes – ocular lubricants Chronic corneal inflammation and neovascularisation respond to low dose topical steroid (but risk of perforation) Corneal perforation – keratoplasty Prominent telangiectasiae suggests topical steroid use Gross rosacea Rosacea may persist and worsen Exacerbated by anything causing flushing Persistent red face with flushing may prove resistant to treatment Remember carcinoid, facial fluishing but absence of other stigmata of rosacea. Treatment Mainstay broad spec antibiotics, mode of action unknown Oxytetracycline 500 mgs bd Rule of 1/3rds 1/3rd better after 8 wks 1/3rd better after 2nd or 3rd 8 wks of oxytet 1/3rd need long term due to persistent relapse on cessation of treatment Can use erythromycin or doxycycline Antibiotics given for 2 months, should see improvement by 16 wks Topicals 0.75% metronidazole gel (Rosex) not as effective as oral antibiotics Useful if get a flare of rosacea Helpful to women candidiasis on antibiotics Azaleic acid gel 15% Clindamycin gel 58 trials, 6633 participants Doxycycline better than placebo 40mgs as effective as 100mgs Topical metronidazole Topical alazaic acid Further well-designed, adequatelypowered randomised controlled trials are required Cochrane link Treatment failure? Most will have erythema/telangiectasiae ‘red face’ Telangiectasiae can be treated by laser Cosmetic camouflage Referral for classical rosacea not responding to treatment ?roaccutane Significant rhinophyma – laser recontouring Opthalmological rosacea Seborrhoeic Eczema Overgrowth of P. ovale (malassesia) in hair follicles giving a secondary eczematous response. >30 yrs males > females Immunocompromised (HIV) Gradual onset with erythema then scale usually in nasolabial folds Often have scalp involvement – dandruff Pink or red scaly ill defined patches, may become more acute with exudates. Typical distribution nasolabial folds, eyebrows, eyelashes (blepharitis), ext auditory meatus Scalp Chest Treatment Tends to be persistent, fluctuating with weather, stress Need to know how to look after the problem Pityrosporum ovale Inflammation antifungals topical steroids Treatment Treat yeast with imidazole eg ketoconazole Nizoral shampoo twice weekly and cream bd Maintainance shampoo once every 2 wks and cream in bursts every 2 weeks 1% Hydrocortisone cream 2% salicylic acid, 2% sulphur in aq. Cream Lithium (ethalith) may be effective SLE A syndrome Idiopathic or drug induced associated with autoantibodies General symptoms Fatigue Fever Weight loss Malaise SLE malar rash Diagnosis: SLE requires 4 of 11 criteria Malar rash Discoid rash Photosensitivity Oral Ulcers Polyarthritis involving more than 2 joints Pleuritis or Pericarditis Antinuclear antibody titer positive (1:40 or higher) Titer over 1:320 is very suggestive Renal disease Neurologic disorder (e.g. Seizures, Psychosis) Anaemia, neutropenia or thrombocytopenia Anti-dsDNA, Anti-Sm positive, syphilis false positive CDLE Probably autoimmune affecting skin only not assoc with circulating antibodies Precipitated and aggravated by sun Middle aged and above Gradual onset, patients notice scaly patches on the face Absence of systemic symptoms Prognosis, tends to persist until burnt out Treatment Potent top steroids – ie dermovate regularly High factor sunscreens Antimalarials – hydroxychloroquine if extensive or doesn’t respond Retinoids Immunosuppressants if severe and extensive Light induced problems Light sensitivity Juvenile Spring Eruption PLE Sun damaged Solar elastosis AKs DLE SLE Melasma Actinic keratoses Malignant potential 0.1 – 10% > 40yrs up to 40% population May regress, remain static or undergo malignant transformation Cryotherapy Diclofenac 5-fluouracil Imiquimod PDT Treatment Cryotherapy 5-15 secs freeze time 3% Diclofenac (Solaraze) gel BNF: Apply thinly twice daily for 60–90 days; max. 8 g daily (carry on up the…………) • Imiquimod (Aldara). BNF: apply to lesion 3 times a week for 4 weeks; assess response after a 4 week treatment-free interval; repeat 4week course if lesions persist; max. 2 courses Local reactions common on this regime – erythema, burning, ulceration, headache, flu symptoms Field change actinic damage Imiquimod weekly for 24 wks 20 patients 28 wk trial once weekly for 24 wks assessed at 28 wks 46.7% marked improvement 6.7% improved on placebo 5-FU (BNF) Apply thinly to the affected area once or twice daily; if possible, cover malignant lesions with occlusive dressing; max. area of skin treated at one time, 500 cm2 (23x23cm); usual duration of initial therapy, 3–4 weeks • Local irritation, severe discomfort (top steroid)