f presentation

Chapter 18 – Anatomy of the
Cardiovascular System
Dr. Kim Wilson
Heart
• Location of the heart (Figure 18-2)
– Lies in the mediastinum, behind the body of the sternum between the points of attachment of ribs two through six
– Approximately two thirds of its mass is to the left of the midline of the body, and one third is to the right
– Posteriorly the heart rests on the bodies of vertebrae T5-T8
– Apex lies on the diaphragm, pointing to the left
– Base lies just below the second rib
– Boundaries of the heart are clinically important as an aid in diagnosing heart disorders
Location of the Heart
Size and Shape of the Heart
• Size and shape of the heart
– At birth, is transverse and appears large in proportion to the diameter of the chest cavity
– Between puberty and 25 years of age the heart attains its adult shape and weight
– In an adult, the shape of the heart tends to resemble that of the chest
Heart
Anatomy
Coverings of the Heart
– Structure of the heart coverings
• Pericardium (Figure 18-4)
– Fibrous pericardium: tough, loose-fitting inextensible sac
– Serous pericardium:
» parietal layer lies inside the fibrous pericardium
» visceral layer
(epicardium) adheres to the outside of the heart
» pericardial space with pericardial fluid separates the two layers
– Heart coverings protect against friction
Wall of the Heart
• Structure of the heart
– Wall of the heart: composed of three distinct layers (Figure
18-5)
• Epicardium: outer layer of heart wall
• Myocardium: thick, contractile middle layer of heart wall; compresses the heart cavities, and the blood within them, with great force
• Endocardium: delicate inner layer of endothelial tissue
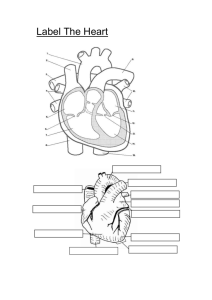
Chambers of the Heart
– Divided into four cavities with the right and left chambers separated by the septum (Figures 18-6 and 18-7)
• Atria
– Two superior chambers known as receiving chambers because they receive blood from veins
– Atria alternately contract and relax to receive blood and then push it into ventricles
– Myocardial wall of each atrium is not very thick because little pressure is needed to move blood such a small distance
– Auricle: earlike flap protruding from each atrium
Chambers of the Heart
• Ventricles
– Two lower chambers known as pumping chambers because they push blood into the large network of vessels
– Ventricular myocardium is thicker than the myocardium of the atria because great force must be generated to pump the blood a large distance
– myocardium of left ventricle is thicker than the right because it must push blood much further
Valves of the Heart
– Valves of the heart: mechanical devices that permit the flow of blood in one direction only (Figure 18-8)
• Atrioventricular (AV) valves: prevent blood from flowing back into the atria from the ventricles when the ventricles contract
– Tricuspid valve (right AV valve): guards the right atrioventricular orifice; free edges of three flaps of endocardium are attached to papillary muscles by chordae tendineae
– Bicuspid, or mitral, valve (left AV valve): similar in structure to tricuspid valve except has only two flaps
Valves of the Heart
• Semilunar valves: half-moon– shaped flaps growing out from the lining of the pulmonary artery and aorta; prevent blood from flowing back into the ventricles from the aorta and pulmonary artery
– Pulmonary valve: valve at entrance of the pulmonary artery
– Aortic valve: valve at entrance of the aorta
Skeleton of the Heart
• Set of connected rings that serve as a semirigid support for the heart valves and the attachment of cardiac muscle of the myocardium
• Serves as an electrical barrier between the myocardium of the atria and that of the ventricles
• Surface projection (Figure
18-9)
Flow of Blood Through the Heart
Right Side
Right atrium
Right atrioventricular (tricuspid) valve
Right ventricle
Pulmonary semilunar valve
Pulmonary trunk & artery
Pulmonary veins → left atrium
Left Side
Left atrium
Left atrioventricular (mitral) valve
Left ventricle
Aortic semilunar valve
Aorta
All tissues of the body
Blood Supply of Heart Tissue – Coronary
Arteries
– Blood supply of heart tissue (Figures 18-10 and 18-11)
• Coronary arteries: myocardial cells receive blood from the right and left coronary arteries
– First branches to come from the aorta
– Ventricles receive blood from branches of both right and left coronary arteries
– Each ventricle receives blood only from a small branch of the corresponding coronary artery
– Most abundant blood supply goes to the myocardium of the left ventricle
– Right coronary artery is dominant in approximately
50% of all hearts and the left in about 20%; neither coronary artery is dominant in approximately 30%
– Few anastomoses (one or more branches) exist between the larger branches of the coronary arteries
Blood Supply of Heart Tissue – Coronary
Arteries
Coronary Veins
• Veins of the coronary circulation
– As a rule, veins follow a course that closely parallels that of coronary arteries
– After going through cardiac veins, blood enters the coronary sinus to drain into the right atrium
– Several veins drain directly into the right atrium
Nerve Supply of the Heart
• Conduction system of the heart: composed of modified cardiac muscle, it generates and distributes the heart’s own rhythmic contractions; can be regulated by afferent nerves
• Cardiac plexuses: located near the arch of the aorta; composed of sympathetic and parasympathetic fibers
• Fibers from the cardiac plexus accompany the right and left coronary arteries to enter the heart
• Most fibers end in the sinoatrial (SA) node, but some end in the atrioventricular (AV) node and in the atrial myocardium; the nodes are the heart’s pacemakers
• Sympathetic nerves: accelerator nerves
• Vagus fibers: inhibitory, or depressor, nerves
Blood Vessels
• Types of blood vessels
– Arteries
• Carry blood away from heart; all arteries except pulmonary artery carry oxygenated blood
• Elastic arteries are largest in body (e.g., aorta and its major branches)
– Able to stretch without injury
– Accommodate surge of blood when heart contracts and able to recoil when ventricles relax
Types of Blood Vessels - Arteries
– Arteries (cont.)
• Muscular (distributing) arteries
– Smaller in diameter than elastic arteries
– Muscular layer is thick
– Examples: brachial, gastric, superior mesenteric
• Arterioles (resistance vessels)
– Smallest arteries
– Important in regulating blood flow to end organs
• Metarterioles
– Short connecting vessel between true arteriole and 20 to 100 capillaries
– Encircled by precapillary sphincters
– Distal end called thoroughfare channel, which is free of precapillary sphincters
Capillaries
• Types of blood vessels (cont.)
– Capillaries
• Primary exchange vessels
• Microscopic vessels
• Carry blood from arterioles to venules; together, arterioles, capillaries, and venules constitute the microcirculation (Figure 18-
14)
• Not evenly distributed; highest numbers in tissues with high metabolic rate; may be absent in some “avascular” tissues, such as cartilage
Capillaries
• Types of blood vessels (cont.)
– Capillaries (cont.)
• Types of capillaries (Figure 18-15)
– True capillaries: receive blood flowing from metarteriole with input regulated by precapillary sphincters
– Continuous capillaries
» Continuous lining of endothelial cells
» Openings called intercellular clefts exist between adjacent endothelial cells
– Fenestrated capillaries
» Have both intercellular clefts and “holes,” or fenestrations, through plasma membrane to facilitate exchange functions
– Sinusoids
» Large lumen and tortuous course
» Absent or incomplete basement membrane
» Very porous; permit migration of cells into or out of vessel lumen
Types of Capillaries
Types of Blood Vessels - Veins
• Types of blood vessels (cont.)
– Veins
• Carry blood toward the heart
• Act as collectors and reservoir vessels; called
capacitance vessels
• Structure of blood vessels (Figure 18-13)
– Layers
• Tunica externa: found in arteries and veins (tunica adventitia)
• Tunica media: found in arteries and veins
• Tunica intima: found in all blood vessels; only layer present in capillaries
Structure of Blood Vessels
– “Building blocks” commonly present
• Lining endothelial cells
– Only lining found in capillary
– Line entire vascular tree
– Provide a smooth luminal surface; protect against intravascular coagulation
– Intercellular clefts, cytoplasmic pores, and fenestrations allow exchange to occur between blood and tissue fluid
– Capable of secreting a number of substances
– Capable of reproduction
Structure of Blood Vessels
• Collagen fibers
– Exhibit woven appearance
– Formed from protein molecules that aggregate into fibers
– Visible with light microscope
– Have only a limited ability to stretch (2% to 3%) under physiological conditions
– Strengthen and keep lumen of vessel open
Structure of Blood Vessels
• Elastic fibers
– Composed of insoluble protein called elastin
– Form highly elastic networks
– Fibers can stretch more than 100% under physiological conditions
– Play important role in creating passive tension to help regulate blood pressure throughout the cardiac cycle
• Smooth muscle fibers
– Present in all segments of vascular system except capillaries
– Most numerous in elastic and muscular arteries
– Exert active tension in vessels when contracting
Circulatory Routes
• Circulatory routes (Figure 18-16)
– Systemic circulation: blood flows from the left ventricle of the heart through blood vessels to all parts of the body (except gas exchange tissues of lungs) and back to the right atrium
– Pulmonary circulation: venous blood moves from right atrium to right ventricle to pulmonary artery to lung arterioles and capillaries, where gases are exchanged; oxygenated blood returns to left atrium by pulmonary veins; from left atrium, blood enters the left ventricle
Systemic Circulation
• Systemic circulation
– Systemic arteries (Tables 18-2 to 18-6; Figures 18-17 to
18-22)
• Main arteries give off branches, which continue to rebranch, forming arterioles and then capillaries
• End arteries: arteries that eventually diverge into capillaries
• Arterial anastomoses: arteries that open into other branches of the same or other arteries; incidence of arterial anastomoses increases as distance from the heart increases
• Arteriovenous anastomoses, or shunts, occur when blood flows from an artery directly into a vein
Fig. 18-17.
Principal Arteries of the Body
Fig. 18-18.
Branches of the Aorta
Fig. 18-19. Arteries of the Head and Neck
Fig. 18-20. Arteries of the Brain
Fig. 18-21. Arteries of the Upper Extremity
Fig. 18-22. Arteries of the Lower Extremity
Veins
• Systemic circulation (cont.)
– Systemic veins (Figures 18-23 to 18-29)
• Veins are the ultimate extensions of capillaries; unite into vessels of increasing size to form venules and then veins
• Large veins of the cranial cavity are called dural sinuses
• Veins anastomose the same as arteries
• Venous blood from the head, neck, upper extremities, and thoracic cavity (except lungs) drains into superior vena cava
• Venous blood from thoracic organs drains directly into superior vena cava or azygos vein
Fig. 18-23.
Veins of the
Body
Veins of the
Head and
Neck
Fig. 18-25. Veins of the Upper
Extremity
Fig. 18-28. Veins of the Lower
Extremity
Fig. 18-26. Inferior Vena Cava
Hepatic Portal Circulation
• Hepatic portal circulation (Figures
18-16 and 18-28)
– Veins from the spleen, stomach, pancreas, gallbladder, and intestines send blood to the liver by the hepatic portal vein
– In the liver the venous blood mingles with arterial blood in the capillaries and is eventually drained from the liver by hepatic veins that join the inferior vena cava
• Venous blood from the lower extremities and abdomen drains into the inferior vena cava
Fetal Circulation
• The basic plan of fetal circulation: additional vessels needed to allow fetal blood to secure oxygen and nutrients from maternal blood at the placenta (Figure 18-29)
• Two umbilical arteries: extensions of the internal iliac arteries that carry fetal blood to the placenta
• Placenta: where exchange of oxygen and other substances between the separate maternal and fetal blood occurs; attached to uterine wall (Figure 18-30)
• Umbilical vein: returns oxygenated blood from the placenta to the fetus; enters body through the umbilicus and goes to the undersurface of the liver, where it gives off two or three branches and then continues as the ductus venosus
Fetal Circulation
• Additional vessels needed cont.
• Ductus venosus: continuation of the umbilical vein; drains into inferior vena cava
• Foramen ovale: opening in septum between the right and left atria
• Ductus arteriosus: small vessel connecting the pulmonary artery with the descending thoracic aorta
Changes in Fetal Circulation after Birth
• When umbilical cord is cut, the two umbilical arteries, placenta, and umbilical vein no longer function
• Umbilical vein within the baby’s body becomes the round ligament of the liver
• Ductus venosus becomes the ligamentum venosum of the liver
• Foramen ovale: functionally closed shortly after a newborn’s first breath and pulmonary circulation is established; structural closure takes approximately 9 months
• Ductus arteriosus: contracts with establishment of respiration; becomes ligamentum arteriosum
Cycle of Life: Cardiovascular Anatomy
• Birth: change from placenta-dependent system
• Heart and blood vessels maintain basic structure and function from childhood through adulthood
– Exercise thickens myocardium and increases the supply of blood vessels in skeletal muscle tissue
• Adulthood through later adulthood: degenerative changes
– Atherosclerosis: blockage or weakening of critical arteries
– Heart valves and myocardial tissue degenerate, reducing pumping efficiency