Geriatric Pharmacology &Polypharmacy
advertisement

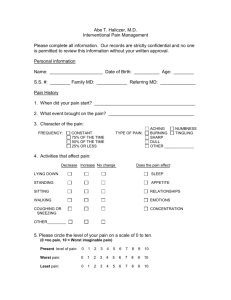
Geriatric Pharmacology & Polypharmacy Problems for Physical Therapists Marilyn James-Kracke, Ph.D. Associate Professor of Pharmacology University of Missouri - Columbia Medical School 1. Why physical therapists benefit from knowing some basic pharmacology. PT 2. Why elderly people experience more adverse drug reactions. 3. Which medications can cause problems that affect the work of physical therapists. Pharmacology Lecture outline Physical Therapy and Pharmacology • Ovid search since 1966 = 13 papers - most from an Australian group G. Lansbury et al. • Hypothesis Physical therapists • J. of Allied Health. 2002 • Conclusions • A substantial proportion of practicing physical therapists in Australia advised and administered OTC medications despite their limited training and knowledge in the area. • In their opinion, this practice adds occupational risk - either often have limited knowledge and little formal training in pharmacology, yet they frequently advise their clients on the use of over-the-counter (OTC) medications and administer these in the course of treatment. • The Lansbury et al approach was to perform a survey of 25% of all PTs teach pharm or stop prescribing. in Australia to see if their hypothesis-this was pharmacology correct. My conclusion class for PT students is unusual and beneficial • Attitude of the elderly towards PT and medications Older people are more likely to prefer physical means than medications to feel better. • Why • • • • • • • • • • Elderly distrust medications they don’t understand. too many medications prescribed for them - confusing afraid of choking on medications. Physicians are always changing and rushing them. for the elderly, PT provides social interaction as well as health care - they enjoy being with healthy fun therapist. Elderly trust personal contact - like hands on approach nuturing approach - encouragement - humor side effects of the medications often make them feel worse - disoriented, sleepy, weak, stomach ulcers, hearing impairment, etc For the elderly, medication risk is greater and benefit is less than in younger people. In contrast, physical therapy has little risk and definite benefits in both the old and the young. The physical therapist is trusted. Older patients want your advice on everything including their medications. This could be good or bad. This is probably true for younger people also! Adverse Drug reactions more common in the elderly = authors of studies Bounce back time - If an elderly person is started on a new medication and 2 to 3 days later they are taken to the emergency room, suspect a drug reaction. If a older patient seems very different than at your last PT session, ask them if they are taking any new medications. Magnitude of the Medication problems in the elderly • Patients >65 years old were 13% of the population by 2000. • Patients greater than >85 years old are the fastest growing segment of the population. • This 13% of the population consumes 30% of all medications • Elderly population is expected to triple from 1985 to 2060. • Elderly are the most physiologically heterogeneous category - state of health varies extensively - physical strength, - cardiac condition, renal and liver function for clearance of drugs. • Compliance - misuse and errors - side effects Factors contributing to adverse drug reactions in elderly patients Heart, kidney, liver, thyroid Orthostatic hypotension, when they standup, blood goes to their feet - weak sympathetic nervous system response to constrict veins and increase heart rate. Low thyroid function causes lower body temperature, metabolic rate, & heart rate. Polypharmacy How many prescription medications are too many? >4 or >6 Many elderly people receive 12 medications per day Kidney clearance is reduced Blood flow to all organs like kidney and liver is reduced therefore clearance is reduced - exercise may help them clear more drug by increasing circulation Breathing affects clearance of inhaled Note - drug absorption is normal in the elderly - slow GI tract gives plenty anesthetics but may contribute to of time for absorption lower interest in physical activity lower clearance of drugs Biggest errors made in prescribing for elderly people • Polypharmacy - a drug for every complaint and elderly people have lots of aches and pains, circulation and breathing difficulties etc • Side effects are missed because they are misinterpreted as part of getting old - particularly senility - hearing loss etc • Elderly people often see a different doctor every time and the next doctor does not realize that the patient was clever and active a week ago. • Physicians often assume that the patient is ill because they are not taking their medications when in fact they are taking them and the amount prescribed for them too much. Reasons why elderly have compliance problems for taking medications • • • • • • • • opening pill containers(weak/arthritis pain/tremors/spills) fear of choking while swallowing large pills reading the labels and information depression - sleepy - poor concept of time for doses cognitive impairment - can’t recall a few moments ago cost of medications are prohibitive -- food vs. medications adverse drug reactions limit benefit of medications Bottom line - you’re never sure whether they are taking too much or too little. Elderly are more likely to tell their PT than their doctor whether they are taking their medications or not because they are too polite to tell a doctor that his pills make them feel sicker. You are in a position to make a difference!! Medication problems that affect the physical therapist’s work • • • • • • • • • • Deafness - problem communicating visual acuity - problem seeing demonstration drowsiness &/or mental status - remembering instructions Beta2 agonist balance, fainting, strength, relax bronchioles albuterol cardiovascular strength respiratory ability-oxygenation -ability to use inhalers? abdominal discomfort joint pain, range of motion bruising skin rashes - skin thinning, cracking, bleeding Dizziness, Fainting and Weakness • Inner ear disturbances, nauseants, low blood pressure, anemia and hypoxia, electrolyte imbalances like hypokalemia, dehydration. • Antihypertensive medications - beta blockers, Ca channel blockers, diuretics, ACE inhibitors, nitrates, clonidine, alpha blockers orthostatic hypotension - side effect is an extension of the desired blood pressure lowering. • Antianginal therapy - nitrates, beta blockers, Ca channel blockers • Certain antiarrythmic drugs - bretylium, amiodarone • Drugs that cause anemia - NSAIDs can cause bleeding of the GI tract which can lead to severe anemia • Cytotoxic agents used to treat cancers or arthritis or autoimmune diseases like lupus erythematosis, and to prevent transplant rejection also inhibit the bone marrow from making red blood cells – methotrexate – cyclophosphamide – azathioprine – cyclosporine Drugs that cause drowsiness and loss of mental accuity • • • • • antihistamines (some are used as sleep aids) Pain medications muscle relaxants antinauseants some beta blockers - like propranolol • drugs that cause insomnia - prevent a good night sleep (caffeine, aminophylline, albuterol) - eventually cause daytime drowsiness. Low concentration of antidepressant are sleep aids, amitryptiline in patients with Parkinson’s while higher concentrations for depression can cause insomnia. Abdominal discomfort • Constipation, inability to void the bladder completely, stomach and gastric ulcers, inflamed bowel disease. • drugs that cause these problems are: • • • • • pain medications containing narcotics - inhibit GI motility antimuscarinic agents - inhibit motility - slow transit through GI tract. antihistamines have antimuscarinic side effects NSAIDs - inhibit prostaglandin synthesis in the gut leads to ulcers cytotoxic agents for chemotherapy - epithelial cells lining the GI tract slough off • antibiotics disturb the normal flora and allow pathogenic bacteria to grow - causes diarrhea and flatulence - solved by taking antibiotics with yogurt - Drug induced muscle wasting catabolism, anorexia, cachexia • • • • • • • • • • • Glucocorticoid steroids used as antiinflammatory agents - body burns glucose and protein (in muscle) but not fat - causes muscle wasting - fat body & thin limbs Beta2 agonists - increase blood flow to muscles but high doses cause tremor and low K. beta blockers - intermittent claudication - pain in muscles causing limping - 4 to 7 % of patients have this effect digoxin - hypokalemia = low K - causes muscle and cardiac weakness diuretics - low K - should receive K supplement or change to K sparing diuretics spironolactone - old people call these water pills. Angiotensin Converting Enzyme inhibitors = ACE inhibitors (captopril, enalopril) lower blood pressure but can also cause rhabdomyolosis Bromocriptine - Parkinson’s patients - dopamine stimulates the chemoreceptor trigger zone in the brain - anorexia Methylphenidate - stimulant to treat narcolepsy or attention deficit disorder amphetamine like - similar to agents used in diet pills to suppress appetite. Chemotherapy - cytotoxic agents cause extreme nausea Cachexia - increased tumor necrosis factor alpha causes the body to become insensitive to insulin - starvation in the midst of plenty. Muscle wasting is more likely due to disease rather than drug induced lack of appetite. Joint pain, range of motion • 30 drugs are listed to cause this - but most are low incidence • injections of microcrystalline steroids into joints = relieves pain, lasts for a month, shorter relief each time because more rapid destruction of the joint - greater pain after effect wears off. • Beta blockers betaxolol pindolol - 7 to 10% experience myalgia • Cholesterol lowering agents - fenofibrate -rhabdomyolosis • clozapine - used for abnormal movement disorders and aggressive behaviors - neuroleptic • danazol - androgenic steroid • droloxifene - nonsteroidal antiestrogen • rifampin - used to treat tuberculosis - first week of therapy • losartan valsartan- to lower blood pressure, uncommon side effect. • Ca channel blockers - uncommon Analgesics - nonsteroidal antiinflammatory drugs = NSAIDs • Old arthritic people take more of these but they are also prone to stomach/intestinal ulceration due to cycloxygenase inhibition of the synthesis of protective prostaglandins in the gastric mucosa. • chronic slow blood loss causes anemia – look for very pale weak patient • can be sudden onset - severe hemorrhage • platelet activity is slowed by NSAIDS • patients taking these meds should be asked if they have abdominal discomfort before starting activity • activity increases blood pressure - may precipitate a bleed • longer term use of high dose NSAIDs can cause kidney damage and loss of erythropoeitin made by the kidney which is a hormone that stimulates red cell production and without it there is anemia. Bruising - hematomas • Vit K is important for making clotting factors - malnutrition causes bruising -lack of green leafy vegetables in diet containing Vit K • Anticoagulant dose too high (warfarin-coumadin competes with Vit K) • NSAIDs - inhibit platelets - causes longer bleeding times • antibiotics killed bacteria in the gut that make Vit K • Steroid use - Cushing syndrome - weakens blood vessels • drugs causing dizziness - orthostatic hypotension cause falls – – diuretics (dehydration) blood pressure lowering medications • Ineffective Parkinson’s treatment - excessive falling • cancer chemotherapy - reduces platelets for clotting and makes a person weak enough to fall more frequently. • Intramuscular injections - for people on anticoagulants • Elder abuse *Muscle Relaxants - many mechanisms - not well understood - all of them cause drowsiness as a side effect •GABAB agonist = BACLOFEN, less drowsiness than benzodiazepines! • GABAA agonists = Benzodiazepines DIAZEPAM -CLOTIAZEPAM PINAZEPAM QUAZEPAM TETRAZEPAM •GABA and glycinergic receptors agonist THIOCOLCHICOSIDE •Spinal reflex blockers, MEPROBAMATE CARISOPRODOL CHLORPHENESIN - METHOCARBAMOL, CHLORZOXAZONE,CYCLOBENZAPRINE TOLPERISONE METAXALONE - •Imidazo receptor blocker and alpha2 receptor blocker CLONIDINE, TIZANIDINE - also used to lower blood pressure, ease drug addiction withdrawal - for smoking and alcohol cessation. •Blocker of Ca release from Sarcoplasmic Reticulum in muscles DANTROLENE •Neuromuscular Cholinergic receptor blockade = Curoniums ALCURONIUM ATRACURIUM - CISATRACURIUM - DOXACURIUM, ETIZOLAM, KETAZOLAM MIVACURIUM,- PANCURONIUM, PIPECURONIUM, RAPACURONIUM, ROCURONIUM - TUBOCURARINE VECURONIUM - used mainly to produce muscle paralysis in surgery •Acetylcholine agonist depolarizing blockers SUCCINYLCHOLINE used in surgery Drug induced ototoxicity (deafness) at plasma levels above therapeutic level • Aminoglycoside antibiotics cause irreversible deafness - like gentamicin, tobramycin, amikacin • antidepressants • loop diuretics - furosemide (lasix) • erythromycin azithromycin • NSAIDs and salicylates [aspirin causes tinnutis - ringing of the ears but acetominophen does not] - this type of hearing loss is reversible • quinine - tinnutis • vancomycin Drug Induced oculotoxicity (vision impairment) • Allopurinol - used to treat gout - can cause cataracts • amatadine - antiparkinson’s antiviral - corneal opacities • amiodarone - antiarrythmic corneal microdeposits -reversible • - 10% of patients - high incidence of hypothyroidism too! • • • • • • • • • anticholinergics - ipratropium atrovent blurred vision and glaucoma antidepressants - anticholinergic side effects antihistamines - anticholinergic side effects anticonvulsants - diplopia (double vision), nystagmus -adenergic blocker - reduced tears bromocriptine - myopia blurred vision corticosteroids - glaucoma cataracts digoxin - colored halos - sign of toxicity methotrexate 25% conjunctivitis – - reduced tears & photophobia • phenothiazines - deposits in lens • tamoxifen - antiestrogens, fine retinal opacities The END