Presentation

Anatomy
Chapter 11 Part II – Blood Vessels
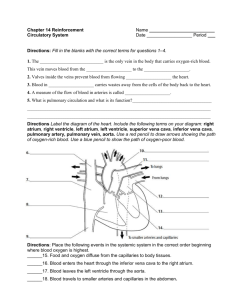
Blood Vessels
Blood circulates inside blood vessels forming a closed transport system called the
vascular system. As the heart beats the blood is propelled into the large arteries leaving the heart. As it moves through the body it enters smaller arterioles which feed the capillary beds of the tissues. Capillary beds drain into venules which empty into veins that empty into the right atria of the heart.
Arteries carry blood away from the heart and veins drain the tissues and return the blood to the heart. The capillary beds serve the needs of the body cells.
Arteries are depicted red to indicate the oxygen-rich blood and veins are depicted blue to indicate oxygen-depleted blood.
Microscopic anatomy of blood vessels
The walls of blood vessels are called tunics.
• Tunica intima – lines the lumen
• Tunica media – smooth muscle, elastic
• Tunica externa - fibrous connective tissue
Scanning electron micrograph of an
artery and a vein in cross section.
Capillaries are found between arteries and veins in the circulatory pathway. Capillaries are composed of tunica intima only, allowing for diffusion between the blood and the body cells.
Structural differences between arteries, veins, and capillaries:
Artery walls are thicker than veins – media is heavier. Arteries are closer to the heart and must be able to expand as blood is forced into them. Artery walls are strong and stretchy to take pressure changes.
Veins are farther from the heart where the pressure is low. The walls are thinner, lumen is larger, and there are valves present to prevent backflow of blood.
Skeletal muscle activity enhances venous blood flow. Inhalation drops the pressure in the thorax allowing large veins near the heart to expand and fill.
Capillary beds are our microcirculatory system.
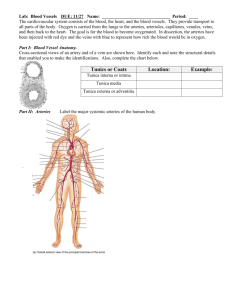
Gross Anatomy Blood Vessels
Major arteries of the systemic system:
•
Aorta – largest artery (garden hose)
• Ascending aorta – upward from heart; coronary arteries that serve the heart
• Aortic arch – arches left, downward into thorax following the spine
Brachiocephalic trunk – splits into the
R. common carotid and R. subclavian
L. Common carotid – branches to L.
internal carotid and L. external carotid to serve the brain, skin of head and neck
L. Subclavian artery – serve part of brain, arm, and the forearm
• Thoracic aorta – passes through diaphragm into abdominal cavity
Intercostal arteries – muscles of thorax walls
Bronchial arteries – lungs
Esophageal arteries – esophagus
Phrenic arteries – diaphragm
Major arteries of the systemic circulation.
Major arteries of the systemic system:
• Abdominal aorta –
Celiac trunk – first branch of abdominal aorta: stomach (gastric), spleen (splenic), liver (hepatic)
Superior Mesenteric artery – small intestine, first half of colon
L. and R. Renal arteries – kidneys
L. and R. Gonadal arteries – gonads; ovaries or testes
Lumbar arteries – heavy muscles of abdomen and trunk walls
Inferior Mesenteric arteries – second half of colon
L. and R. Common iliac arteries – pelvic organs (internal iliac), thigh (external iliac to femoral ), leg, foot (anterior and posterior tibial)
Major arteries of systemic circulation.
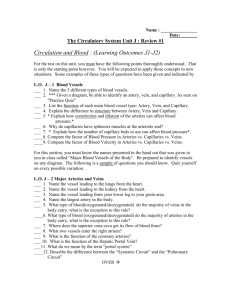
Major Veins of the Systemic Circulation:
Veins are more superficial and some are easily palpated on the body surface. Most deep veins follow the same course of the major arteries. Veins converge on the
venae cavae, which enter the right atrium of the heart. Veins draining the head and arms empty into the superior vena cava and those draining the lower body empty into the interior vena cava.
Veins draining into the superior vena cava: named in a distal to proximal direction.
Radial and ulnar veins – drain the forearm, are (brachial vain), and empty into axillary region
Cephalic vein – drains lateral aspect of the arm, empties into axillary vein
Basilic vein – drains medial aspect of arm, empties into brachial vein
Subclavian vein – blood from arm through axillary vein; skin, muscles of head through external jugular
Vertebral vein – drains posterior part of the head
Internal jugular vein – drains the dural sinuses of the brain
Brachiacephalic vein – receive venous blood from subclavian, vertebral, and internal jugular; all join to from the superior vena cava
Azygos vein – single vein that drains the thorax and enters the vena cava just before it enters the heart
Veins draining into the inferior vena cava: returns blood from below the diaphragm.
Anterior and posterior tibial and fibular
veins – drain the leg, (calf and foot); posterior tibial popliteal vein at the knee and femoral vein at the thigh, then external iliac at pelvis
Great saphenous veins – longest vein in the body; receive superficial drainage of the leg
Common iliac (R. and L. ) vein – formed from the union of external and internal iliac veins (drains pelvis); join to form inferior vena cava, ascends into abdominal cavity
R. Gonadal vein – drains right ovary and right testicle; L. gonadal vein empties into left renal vein
L. and R. Renal veins – drain the kidneys
Hepatic portal vein – single vein that drains the digestive tract organs, carries blood through the liver before systemic circulation
L. and R. Hepatic veins – drains the liver
Special Circulations
Arterial supply of the brain and Circle of Willis
A continuous blood supply to the brain is crucial.
A lack of blood for a few minutes, brain cells die.
The brain is supplied with two pairs of arteries –
internal carotid and vertebral arteries. Anterior and posterior blood supplies are united by small communicating arterial branches called the Circle
of Willis. This circle of vessels protects the brain by providing more than one route for blood to reach the brain tissue.
Hepatic portal circulation – veins drain the digestive organs and delivers the blood to the liver through the hepatic portal vein. The liver processes substances (nutrients – glucose, fat, protein) before they enter the systemic circulation.
Fetal circulation –
The lungs and digestive system of the fetus are not yet working.
All nutrients and excretory gas exchanges occur through the placenta. Nutrients and oxygen move from the mother’s blood into the fetal blood, and fetal wastes move in the opposite direction. The umbilical cord contains three blood vessels; a large umbilical vein and two smaller umbilical arteries. The vein carries nutrient and oxygen rich blood to the fetus. The arteries carry carbon dioxide and wastes from the fetus to the placenta.
Physiology of Circulation:
can be assessed by measuring arterial pressure and blood pressure
Arterial pulse – alternating expansion and recoil of an artery that occurs with each beat of the left ventricle. A pulse or pressure wave travels through the entire arterial system.
Normally the pulse rate (pressure surges per min.) equals the heart rate (beats per min.).
Pulse averages 70 to 76 beats per min. in a normal resting person. It is influenced by activity, postural changes, and emotions.
Vital signs – arterial pulse rate, blood pressure, respiratory rate, and temperature
The pulse can be felt in any artery lying close to the body surface by compressing the artery against firm tissue. Routinely detected where radial artery surfaces on the wrist.
Pressure points – used to measure pulse and are compressed to stop the flow blood during hemorrhage.
Blood Pressure the pressure blood exerts against the inner walls of blood vessels and is the force that keeps the blood circulating between heart beats.
Blood pressure gradient – pressure is highest in the large arteries, high pressure in the arteries forces blood to continually move into areas of lower pressure. Pressure continues to drop throughout the pathway, reaching zero at the vena cava. Blood flows into arterioles, then capillaries, venules, veins, and finally back to the vena cava. Blood flows along a pressure gradient from high to low pressure. Valves in the veins, skeletal activity, and pressure changes in the thorax, keep blood flowing.
Blood pressure in various areas of the cardiovascular system.
Measuring Blood Pressure -
Auscultatory Method of measuring blood pressure
The heart alternately contracts and relaxes causing an on/off flow of blood into the arteries.
This causes the blood pressure to rise and fall during each beat. There are two arterial measurements made:
Systolic pressure is the pressure in the arteries at the peak of ventricular contraction, and diastolic
pressure, the pressure when the ventricles are relaxing.
Blood pressure is reported in millimeters of mercury (mm
Hg).
Measuring the blood pressure in the brachial artery.
Effects of Various Factors on Blood Pressure -
Arterial blood pressure (BP) is directly related to cardiac output (CO) and peripheral resistance (PR): BP = CO X PR
Peripheral resistance - friction; viscosity, narrowing, atherosclerosis; age, weight, time of day, exercise, emotional state, drugs
Neural factors – sympathetic vasoconstriction; hemorrhage, exercise, frightened
Renal factors – osmoregulation; renin; aldosterone
Temperature –cold/ vasoconstriction, heat/ vasodilation
Chemicals – epinephrine, nicotine, alcohol, histamine
Diet – low sodium, low saturated fat, low cholesterol help prevent hypertension
Summary of factors causing and increase in arterial blood pressure.
Variations in Blood Pressure
Normal adults at rest, should have a systolic pressure that varies between 110 and 140 mm Hg, and a diastolic pressure between 75 and 80 mm Hg. Blood pressure varies from one person to another. Blood pressure varies with age, weight, race, mood, physical activity, and posture.
Hypotension - low blood pressure. Generally a systolic pressure below 100 mm Hg – individual differences and not usually cause for concern.
Hypertension – persistent high blood pressure; is pathological and defined as a condition of sustained elevated arterial pressure of 140/90 or higher.
Capillary Exchange of Gases and Nutrients
Capillaries form an intricate network among the body’s cells.
Diffusion takes place easily with the cells. Substances exchanged first diffuse through the interstitial fluid.
Four routes in the capillary walls:
• Substances can diffuse directly through if they are lipid soluble
(gases)
• Lipid soluble substances may enter or leave by endocytosis or exocytosis
• Limited passage allowed by
intercellular clefts – gaps or areas of the plasma membrane not joined by tight junctions
• Free passage of small solutes and fluids is allowed by fenestrated
capillaries – found where absorption is a priority or where filtration occurs.
Substances exchanged between blood and cells must diffuse through interstitial fluid.
Substances diffuse to and from the body cells according to their concentration gradients.