Facial Nerve Palsy
advertisement

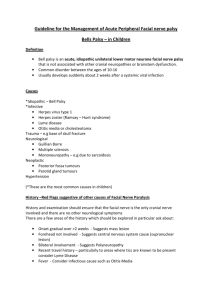
Facial Nerve Palsy Dr. Saud ALROMAIH Anatomy Facial nerve is a mixed nerve, having a motor root and a sensory root. Motor root supplies all the mimetic muscles of the face which develop from the 2nd brachial arch. Anatomy Sensory root “nerve of Wrisberg” carries taste fibers from the anterior 2/3 of the tongue and general sensation from the concha and retroauricular skin. Anatomy Also it carries secretomotor fibers to the lacrimal, submandibular and sublingual glands as well as those in the nose and palate. Anatomy: Nucleus Pons. precentral gyrus. Upper part of the nucleus: – Upper face – Involuntary emotional movements Anatomy: Course Motor fibers originate… Hooks around… Joined by… Facial n. leaves the brainstem… Travels through… Enters the IAC. Then traverse the temporal bone through facial n. canal Leaves the temporal bone through Finally divides into terminal branches. Anatomy: Parts Intracranial part Intratemporal part Extracranial part Anatomy: Intratemporal segments Meatal Labyrinthine Tympanic, horizontal Mastoid, vertical Anatomy: Branches Greater superficial petrosal nerve: Nerve to stapedius: Chorda tympani: Comunicating branch: Posterior auricular nerve: Muscular branches: Peripheral branches: “Pes anserinus” Anatomy: Surgical landmarks Middle Ear and Mastoid Surgery: – Processus chocleariformis – Oval window and horizontal canal – Short process of the incus – Pyramid Anatomy: Surgical landmarks Parotid Surgery: – Cartilaginous pointer: – Styloid process – Posterior belly pf digastric muscle Anatomy: Structure of the nerve From inside outward: – Axon – Myelin sheath – Neurolimma – Endoneurium – Perineurium – Epineurium Anatomy: Severity of injury Saunderland classification: – 1°: Partial block: Neuropraxia – 2°: Loss of axons: axonotemesis – 3°: Injury to the endoneurium: neurotemesis – 4°: Injury to the perineurium: partial transection – 5°: Injury to the epineurium: complete transection History: Onset: Sudden vs. Gradual Duration: Rate of progression: Recuurent or familial Associated symptoms Medical history Previous surgeries Physical exam: Complete vs. incomplete Segmental vs. uniform involvement Unilateral vs. bilateral Cranial nerves assessment Neurologic evaluation Cerebellar signs Physical exam: Microscopic otoscopy Complete head and neck exam Physical exam: Localization of facial nerve lesion: Central vs. Peripheral. Physical exam: Localization of facial nerve lesion: Peripheral: – Level of nucleus – CPA level: – Bony canal level: Topodiagnostics – Outside the Temporal bone Physical exam: Topodiagnostics: – Schirmer’s test: – Stapedial reflex: – Taste test: – Submandibular salivery flow test: Warton’s ducts Causes: Central: Intacranial part: Intratemporal part: Extracranial part: Systemic: Causes: Central: – Brain abscess – Pontine glioma – Poliomyelitis – Multiple sclerosis Causes: Intacranial part: – Acoustic neuroma – Meningioma – Metastatic CA – Meningitis Causes: Intratemporal part: – Idiopathic: Bell’s palsy Melkersson’s syndrome Causes: Intratemporal part: – Infections: ASOM CSOM Herpes Zoster Oticus Causes: Intratemporal part: – Trauma: Surgical: Mastoidectomy, Stapedectomy Accidental:# temporal bone Causes: Intratemporal part: – Neoplasms: Glomus jugulare tumour Facial nerve neuroma Metastatic CA Causes: Extracranial part: – Parotid gland CA – Parotid gland surgery – Parotid gland injury – Neonatal facial nerve injury Causes: Systemic: – DM – Hypothyroidism – Uremia – PAN – Wegener’s granulomatosis – Sarcoidosis – Leprosy – Leukemia Labs: Pure-tune audiometry Electrophysiologic tests Imaging tests Others Labs: Electrophysiologic tests: – Nerve Excitability Test: NET – Maximum stimulation Test: MST – Electroneurography: ENoG – Electromyography: EMG Complications: Incomplete recovery Exposure keratitis Synkinesis Tics and spasms Contractures Crocodile tears Frey’s syndrome “gustatory sweating” Psychological and social problems Bell’s Palsy Dr. Saud ALROMAIH Background: one of the most common neurologic disorders affecting the cranial nerves. abrupt, unilateral, peripheral facial paresis or paralysis without a detectable cause. Background: first described more than a century ago by Sir Charles Bell, yet much controversy still surrounds its etiology and management. Bell palsy is certainly the most common cause of facial paralysis worldwide. Incidence: United States Internationally Incidence: The incidence of Bell palsy in the United States is approximately 23 cases per 100,000 persons. Internationally: The incidence is the same as in the United States. Demographics: Race: Sex: Age: Demographics: Race: slightly higher in persons of Japanese descent. Sex: No difference exists Age: highest in persons aged 15-45 years. Bell palsy is less common in those younger than 15 years and in those older than 60 years. Pathophysiology: Main cause of Bell's palsy is latent herpes viruses (herpes simplex virus type 1 and herpes zoster virus), which are reactivated from cranial nerve ganglia. Polymerase chain reaction techniques have isolated herpes virus DNA from the facial nerve during acute palsy. Pathophysiology: Inflammation of the nerve initially results in a reversible neurapraxia, Herpes zoster virus shows more aggressive biological behaviour than herpes simplex virus type 1 History: The most alarming symptom of Bell's palsy is paresis Up to three quarters of affected patients think they have had a stroke or have an intracranial tumour. History: The palsy is often sudden in onset and evolves rapidly, with maximal facial weakness developing within two days. Associated symptoms may be hyperacusis, decreased production of tears, and altered taste. History: Patients may also mention otalgia or aural fullness and facial or retroauricular pain, which is typically mild and may precede the palsy. A slow onset progressive palsy with other cranial nerve deficits or headache raises the possibility of a neoplasm Physical exam: Bell's palsy causes a peripheral lower motor neurone palsy, which manifests as the unilateral impairment of movement in the facial and platysma muscles, drooping of the brow and corner of the mouth, and impaired closure of the eye and mouth. Physical exam: Bell's phenomenon—upward diversion of the eye on attempted closure of the lid—is seen when eye closure is incomplete. Physical exam: Polyposis or granulations in the ear canal may suggest cholesteatoma or malignant otitis externa. Vesicles in the conchal bowl, soft palate, or tongue suggest Ramsay Hunt syndrome Physical exam: The examination should exclude masses in the head and neck. A deep lobe parotid tumour may only be identified clinically by careful examination of the oropharynx and ipsilateral tonsil to rule out asymmetry. Investigations: Serum testing for rising antibody titres to herpes virus is not a reliable diagnostic tool for Bell's palsy. Salivary PCR for herpes simplex virus type 1 or herpes zoster virus is more likely to confirm virus during the replicating phase, but these tests remain research tools. Investigations: MRI has revolutionised the detection of tumours. Investigations: Topognostic tests and electroneurography may give useful prognostic information but remain research tools. Diagnosis: Bell palsy is a diagnosis of exclusion. Other disease states or conditions that present with facial palsies are often misdiagnosed as idiopathic. Management: The main aims of treatment in the acute phase of Bell's palsy are to speed recovery and to prevent corneal complications. Treatment should begin immediately to inhibit viral replication and the effect on subsequent pathophysiological processes that affect the facial nerve. Psychological support is also essential, and for this reason patients may require regular follow up. Management, Eye care Management, Eye care It focuses on protecting the cornea from drying and abrasion due to problems with lid closure and the tearing mechanism. The patient is educated to report new findings such as pain, discharge, or change in vision. Lubricating drops should be applied hourly during the day and a simple eye ointment should be used at night. Management, Steroid Management, Steroid Two systematic reviews concluded that Bell's palsy could be effectively treated with corticosteroids in the first seven days, providing up to a further 17% of patients with a good outcome in addition to the 80% that spontaneously improve. Management, Steroid Usual regimen is 1mg/kg/day for 1 week. To be tapered in the 2nd week. Management, Steroid Cochrane review*: “There is insufficient evidence about the effects of corticosteroids for people with Bell's palsy, although their anti-inflammatory effect might prevent nerve damage.” *Salinas RA, Alvarez G, Ferreira J. Corticosteroids for Bell's palsy (idiopathic facial paralysis). Cochrane Database of Systematic Reviews 2004, Issue 4. Art. No.: CD001942. Management, Antivirals It seems logical in Bell's palsy because of the probable involvement of herpes viruses. Aciclovir, a nucleotide analogue, interferes with herpes virus DNA polymerase and inhibits DNA replication. Management, Antivirals Usual regimen is 4000mg/24hrs divided into 5 doses for 7 to 10 days Bell’s palsy: Antivirals: Cochrane review*: “More evidence is needed to show whether the antiviral drugs acyclovir or valacyclovir are effective in aiding recovery from Bell's palsy.” * Allen D, Dunn L. Acyclovir or valaciclovir for Bell's palsy (idiopathic facial paralysis). Cochrane Database of Systematic Reviews 2004, Issue 3. Art. No.: CD001869. Outcomes: It has a fair prognosis without treatment, with almost three quarters of patients recovering normal mimetical function and just over a tenth having minor sequelae. A sixth of patients are left with either moderate to severe weakness, contracture, hemifacial spasm, or synkinesis. Outcomes: Patients with a partial palsy fair better, with 94% making a full recovery. The outcome is worse when herpes zoster virus infection is involved in partial palsy. Outcomes: In patients who recover without treatment, major improvement occurs within three weeks in most. If recovery does not occur within this time, then it is unlikely to be seen until four to six months, when nerve regrowth and reinnervation have occurred. Bad Prognostic Factor: Complete facial palsy No recovery by three weeks Age over 60 years Severe pain Ramsay Hunt syndrome (herpes zoster virus) Associated conditions—hypertension, diabetes, pregnancy Severe degeneration of the facial nerve shown by electrophysiological testing Thanks Labs: Nerve Excitability Test: NET : – Indication: complete paralysis<3wks – Interpretation: < or = 3.5 mA threshold: Prognosis Good – Limitation: Not useful in the 1st 3 days or during recovery. Labs: Maximum stimulation Test: MST: – Indication: complete paralysis<3wks – Interpretation: Marked weakness or no muscle contraction: advanced degeneration with guarded prognosis – Limitation: Not Objective. Labs: Electroneurography: ENoG : – Indication: complete paralysis<3wks – Interpretation: < 90% degeneration: prognosis is good; > or = 90%: prognosis is question – Limitation: False-positive results in deblocking phase. Labs: Electromyography: EMG – Indication: Acute paralysis less than 1 week or chronic paralysis longer than 2 weeks – Interpretation: Active mu: intact motor axons Mu + fibrillation potentials: partial degeneration Polyphasic mu: regenerating nerve – Limitation: cannot assess degree of degeneration or prognosis for recovery.