VII Nerve Palsy
advertisement

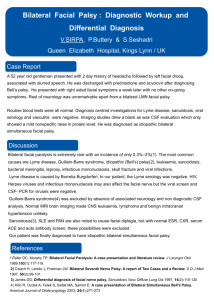
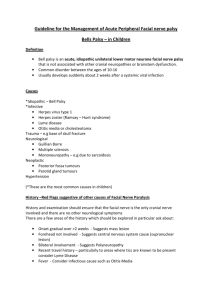
VII Nerve Palsy Examination Upon noticing facial asymmetry, proceed to tests VII nerve functions Look up (frontalis) and attempt to push the folds down, close your eyes (orbicularis oculi) and attempt to force them open, and frown (corrugator superficialis) Look for exposure keratitis, tarsorraphy Nasolabial fold, show your teeth and and blow against closed lips Look for drooling of saliva Determine UMN or LMN, unilateral or bilateral UMN unilateral Examine UL and look for hemiparesis on the same side of the facial weakness Check for xanthelesma, DM signs and BP LMN unilateral Examine other CN VI nerve and contralateral weakness in brainstem lesions CPA lesion (V, VI, VII and VIII with cerebellar) Other CN nerves involvement non-conforming type Basal meningitis lesions Mononeuritis multiplex, MG Therefore proceed to examine the neck Look at the Palate for vesicles Examine the parotids and for surgical scars Mastoid tenderness Examine the neck for cervical LNs Upper limbs Contralateral hemiparesis Ipsilateral cerebellar Ask to examine Otoscopy for vesicles in EC and otitis media For hyperacusis (sensitive to high-pitched or loud sounds) For loss of taste in the anterior two-thirds of the tongue Urine dipstick for glucose and BP Upon noticing facial diplegia, proceed with Rule out MG (Bilateral ptosis) Rule out Dystrophia myotonica or fascio-scapular-humeral dystrophy Bilateral LMN VII Test for frontalis, corrugator and orbicularis oculi Ask patient to show teeth and blow against closed lips Look for V, VI, VIII Examine parotids (Sarcoidosis, amyloidosis) Examine tongue (scrotal tongue for MR syndrome) Examine the upper limbs for GBS, MND, leprosy, Lyme’s (radiculopathy) and bilateral cerebellar signs if suggestive of bilateral CPA tumors Think of rare: Melkersson-Rosenthal syndrome, Mobius syndrome Presentation Sir, this patient has got a right sided lower motor neurone facial nerve palsy as evidenced by: Paralysis of both the upper and lower facial muscles on the right Loss of wrinkling of the right side of the forehead, inability to fully close his right eye shut with Bell’s phenemenon Associated with loss of the right nasolabial fold and drooping of the right angle of the mouth There are no complications of exposure keratitis and there is no drooling of saliva. I also did not notice any evidence of a right sided tarsorraphy There is no associated VI nerve palsy to suggest a brainstem lesion. There are also no features of Cerebellopontine angle lesion with no involvement of the V, VI, VIII or cerebellar signs on the right. I did not find any evidence of a parotid swelling or a surgical scar and there are no vesicles on the palate. There was no right sided facial oedema or plication of the tongue to suggest the rare syndrome of MR syndrome. There is no mastoid tenderness and no enlarged cervical LNs. I did not detect any contralateral hemiparesis or cerebellar signs. I would like to complete my examination by Otoscopy for vesicles in EC and otitis media Ask about hyperacusis (sensitive to high-pitched or loud sounds) Ask for loss of taste in the anterior two-thirds of the tongue Urine dipstick for glucose and BP (mononeuritis multiplex) The most likely cause for this patient would be a right sided Bell’s palsy. Questions What is the course of the facial nerve? VII nerve nucleus lies in the pons in close proximity with VI nerve nuclei VII leave the pons with VIII via the cerebellopontine angle It enters the facial canal and enlarges to become the geniculate ganglion A branch is given off to the stapedius muscle and the greater superficial petrosal branch goes to the lacrimal glands The chorda tympani which supplies taste sensation to the anterior two thirds of the tongue joins the VII nerve in the facial canal VII nerve exits the skull via the stylomastoid foramen, through the parotids with the following branches Temporalis Zygomatic Buccal Mandibular Cervical What are the causes of a unilateral LMN VII nerve palsy? Brainstem (Infarct/haemorrhage, MS, abscess and tumour, syringobulbia) Base of skull lesions (infective, tumour, infiltrative) CPA lesions (acoustic neuroma, meningioma, neurofibroma) Petrous temporal bone (Bell’s palsy, Ramsay Hunt, OM) Parotid (tumour, sarcoidosis, surgery) Mononeuritis multiplex NB: Most common is Bell’s palsy What are the causes of bilateral LMN VII nerve palsies? After ruling out MG and myopathies Bilateral CPA tumor as in NF type 2 Bilateral Bell’s palsy Bilateral Parotid enlargement (Sarcoidosis – Uvoeoparotid fever or Heerfordt’s fever) GBS, MND and leprosy, Lyme disease Rare: Rosenthal Melkersson syndrome (triad of VII palsy with facial edema and plication of the tongue, Mobius syndrome (congenital facial diplegia, oculoparalysis from III and VI and infantile nuclear hypoplasia) What is Bell’s phenemenon? It refers to the upward movement of the right eyeball with incomplete closure of the right eyelid in an attempt to close the right eye. Why are the muscles of the upper face spared in a upper motor neurone lesion? The upper facial muscles are preserved in an UMN lesion as there are bilateral cortical representations of these muscles. What is Bell’s palsy? An idiopathic facial paralysis, believed to be due to viral-mediated cranial neuritis from HSV Typically presents with abrupt onset of weakness with worsening the following day, associated with facial or retroauricular pain, hyperacusis and excessive tearing What is Ramsay Hunt syndrome? Herpes zoster infection of the geniculate ganglion Presents with vertigo, hearing loss, facial weakness, pain in the ear with vesicles seen on the external auditory meatus and palate What is facial synkinesis? Attempt to move one group of facial muscles results in movement of another group Occurs as a result of anomalous regeneration of the facial nerve Egs if nerve fibres which innervate the facial muscles later innervate the lacrmial glands, then patient shed tears on mastication (crocodile tears) How would you investigate? Targeted Ix according to history and physical examination Blood Ix eg Lyme’s disease Imaging How would you manage (Bell’s palsy)? Educate Lubricating eye drops, eye patch, physiotherapy PO Pred 1mg/kg/d for 7-10 days and PO acyclovir 400mg 5X/d for 7 days (within first 72hrs) Regular follow up to look for resolution and exclude new developing signs suggestive of other conditions Surgical (tarsorraphy) for chronic non-resolving cases How would you educate or counsel patient with Bell’s palsy? Common condition Course Improvement onset: 10 days to 2 months Plateau: 6 weeks to 9 months Residual signs Synkinesis Frequency: ~50%; May be reduced by corticosteroid treatment May be treated with botulinum Probably due to anomalous regeneration of nerve Crocodile tears: 6% Face weakness: 30% Contracture: 20% Blepharospasm: May occur years after paralysis Prognosis better Incomplete paralysis Early improvement Slow progression Younger age Normal salivary flow Normal taste Electrodiagnostic tests normal Nerve excitability Electrogustometry