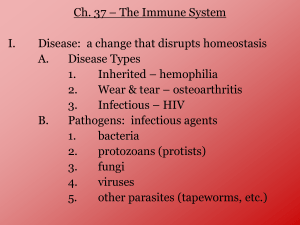
Immunity - Westford Academy Ap Bio
advertisement
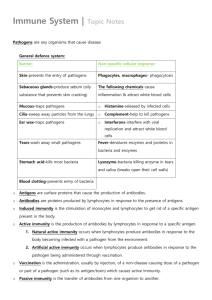
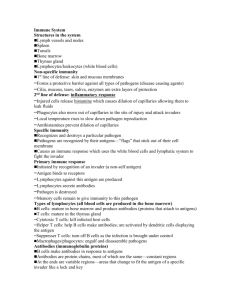
Immunity Human Immune Defenses • Protection against foreign invaders (bacteria, viruses, fungi, etc.) • Three levels of defense: – First line of defense = barrier to prevent entry (skin, mucous membranes) – Second line of defense = general reaction to minimize infection via intruder (inflammation, etc.) – Third line of defense = specific reaction to minimize infection via intruder (MHC, antibodies, T cells, etc.) • Supplementary developments: – Antibiotics, vaccines, and passive immunity First Line of Defense 1. Skin – physical barrier, covered with oily & acidic (pH 3-5) secretions from sweat glands 2. Antimicrobial proteins (e.g. lysozyme) – in saliva, tears, and other mucosal secretions 3. Cilia – line the lungs to sweep intruders up and out 4. Gastric juice – in stomach (pH ~2), kills most microbes 5. Symbiotic bacteria – in digestive tract and vagina, outcompete pathogenic organisms Second Line of Defense • Nonspecific mechanisms • Phagocytes – white blood cells (leukocytes) that phagocytose pathogens, circulate constantly • Complement – proteins (~20 different kinds) that attract phagocytes to foreign cells & promote lysis of pathogens, precursors circulate constantly • Interferons – secreted by cells infected with viruses, stimulate neighboring cells to produce proteins to defend against viral infection • Inflammation – swelling in response to tissue damage Phagocytes: Neutrophils • Neutrophils –Engulf pathogens via phagocytosis Travel to infection site via chemotaxis Neutrophils Remember this little guy from the Inner Life of a Cell? Phagocytes: Monocytes – Mature into large macrophages – Engulf pathogens via phagocytosis Phagocytes: Natural Killer Cells – Attack pathogen-infected body cells – Attack abnormal body cells (tumors) – Nonspecific attack on compromised cells – Action based on activation and inhibitory receptors Granules containing digestive enzymes Phagocytes: Natural Killer Cells Loss of “self” ID tag, no longer inhibits NK cell Complement Pathogen Detection Antibodies bind pathogens and trigger compliment-activating enzymes Pathogen surface receptors trigger complement-activating enzymes Complement Activation Inactive precursors in blood cleaved (by proteases) to become active compliment proteins Amplification of Immune Response Recruitment of Phagocytes Enhancement of Phagocytosis of Pathogens Perforation of Pathogen Cell Membrane (Lysis) Complement: Perforation of Pathogens Interferons Inflammatory Response • Occurs when skin is damaged (damage allows pathogens to enter body) • Histamine secretion by basophils & mast cells (WBC), stimulates vasodialation • Vasodialation – increases blood supply to damaged area, allows WBC and fluids (including complement) to move easier through blood vessel walls (increased permeability of blood vessels) • Phagocytes attracted to site of injury by complement, engulf pathogens • Complement helps phagocytes, stimulates basophil secretion of histamine, helps lyse pathogens Histamine Release • Basophils (WBC) normally circulate in blood (recruited into tissues when needed) • Mast cells (WBC) exist in tissues, particularly near interface with external environmental (skin, lungs, digestive, nose, mouth, eye) • Release histamines in response to pathogens or allergens Pathogen or Vasodialation • Dialation (widening) of blood vessels • Causes redness, increase in temperature, and swelling • Increases delivery of WBC & complement to site of damage • Increase in temperature may stimulate WBC and make environment inhospitable to pathogens Third Line of Defense • Targets specific antigens (on pathogens) • Major histocompatibility complex (MHC) self vs. nonself proteins at surface of all cells • Lymphocytes (WBC) – B cells (make antibodies) • respond to antigens on pathogens • produce plasma & memory cells – T cells • respond to nonself cells • produce cytotoxic/killer T cells & helper T cells Antigens • Antigen = any molecule (usually protein or polysaccharide) identified as foreign – Part of protein coat of virus – Unique molecule in plasma membrane of bacteria, protozoa, pollen, or other foreign cells – Toxin injected by insect sting Antigen Presenting Cells: Macrophages & Dendritic Cells Phagocytosis of pathogen Presentation of antigens to other immune cells Major histocompatibility complex (MHC) • Collection of glycoproteins (proteins with carbohydrate groups) on the membranes of all body cells (ID tag) • Each individual has unique MHC proteins • Self vs. Non-self recognition Carbohydrate groups Polypeptide chains MHC Class I & MHC Class II MHC Class I >Found in all nucleated cells >Function as “ID tag” >Present antigens when cell is infected or malignant MHC Class II >Found in antigen presenting cells >Activate other immune cells >Present antigens after phagocytosis of pathogen Antibodies • On surface of B cells (antigen receptors) • Specific to particular antigens • Y-shaped proteins with constant and variable regions (variable provides antigen specificity) • 5 classes (immunoglobulins): IgA, IgD, IgE, IgG, IgM (different particular activities) Antibodies • Inactivate antigens by binding to them (phagocyte) Agglutination and inactivation of pathogen Antibodies • Binding “flags” cells for death (macrophage phagocytosis, compliment protein lysis) Response to parasites Macrophage Flagged “foreign” cells Antibodies • Binding leads to B cell proliferation (by division): – Plasma cells – release antibodies to circulate through the body – Memory cells – long-lived, circulate & release antibodies with subsequent infection of same pathogen (immunity) T cell Lymphocytes • Work with MHC to identify/destroy non-self cells • Infected cell displays a combo of self and nonself markers (T cell interprets as non-self) • Cancer cells & transplant cells also interpreted as non-self T cell Cancer cell T cell Lyphocytes • T cells encounter non-self cells, divide & produce: – Cytotoxic/killer T cells – recognize & destroy nonself cells by puncturing them (lysis) and activating apoptosis, induced by antigen-presenting cells – Helper T cells – stimulate production of B cells and cytotoxic T cells by secreting interleukins Cytotoxic/Killer T cells Lysis Cytotoxic T cell Apoptosis Don’t confuse your KILLERS! Natural Killer Cells Killer (Cytotoxic) T Cells • • • • • • • • Second line of defense Non-specific response No APC activation Circulate constantly (INNATE immunity) Innate immunity is a non-specific and immediate response, responding in a general way that does not confer long-lasting immunity Third line of defense Specific response Require APC activation Proliferate in response to an infection (ADAPTIVE immunity) Adaptive immunity is a specific and acquired response, producing antibodies and conferring longlasting immunity through memory cells Helper T cells Immune Reactions Cell-mediated Response • Response to any non-self cells (including infected body cells and tumor cells) – Non-self cell binds to T cell – T cells produce cytotoxic T cells (destroy nonself cells) and helper T cells – Helper T cells bind to macrophages (that engulfed pathogens and are now presenting antigens) – Helper T cells produce interleukins (stimulate production of T cells and B cells) Humoral Response • Response to antigens or pathogens circulating in lymph/blood – B cells produce plasma cells and memory cells – Plasma cells release antibodies (bind to antigens) – Memory cells provide future immunity – Macrophage & helper T cells stimulate B cell production (helper T cells bind to macrophages that have engulfed pathogens, then secrete interleukins) Supplementation of Immunity • Antibiotics – derived from bacteria & fungi, harmful to pathogenic microorganisms • Vaccines – inactivated pathogens (or fragments of pathogens), stimulate production of memory cells (prevent disease if pathogen introduced) • Passive immunity – transferred antibodies from immune person to non-immune and infected person (ex: newborns get mom’s antibodies through placenta and via breastmilk) Antibiotics Vaccines Produces memory cells for subsequent antigen exposures Herd immunity reduces spread of infectious diseases Passive Immunity (placenta) pathogen, etc. Natural – placenta (IgG only), breast milk (IgA only) Artificial – serum infusion (used for infection, poisoning, immunodeficiency therapy)