lecture 7 (314)
advertisement

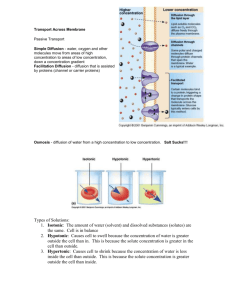
Lecture 7 PHARMACOKINETICS Drug at site of administration Absorption Drug in plasma Distribution Drug/metabolites in tissues Metabolism Drug/metabolites in urine, feces, bile Elimination Definition : The process of movement of unchanged drug from the site of administration to systemic circulation. The ultimate goal is to have the drug reach the site of action in a concentration which produces a pharmacological effect. No matter how the drug is given (other than IV) it must pass through a number of biological membranes before it reaches the site of action. KLECOP, Nipani 08/10/2010 6 Blood Flow To Absorptive Site: o Greater blood flow raises absorption Intestine has greater BF than stomach Total Surface Area of Absorptive Site: o Intestinal microvilli increases surface area to 1000fold that of the stomach favoring intestinal absorption Contact Time at Absorptive Site: Diarrhea reduces absorption Accelerated gastric emptying→ faster delivery to intestinal large surface → increased absorption Food: Presence of food in the gut reduces/delays drug absorption from GIT Increased splanchnic blood flow during eating increases drug absorption Ionized drugs as tetracycline can form insoluble complexes with Ca2+ in food/milk. Formulation Factors: Solid dosage forms dissolution & solubility are essential Aqueous solutions are absorbed more quickly than tablets or suspensions 8 Drug transported by passive diffusion depend upon: dissociation constant, pKa of the drug pH at absorption site. lipid solubility, K o/w. Polarity estimates partition coefficient. The greater the lipid solubility – the faster the rate of diffusion Most drugs are either weak acids or weak bases whose degree of ionization is depend upon pH of biological fluid. For a drug to be absorbed, it should be unionized and the unionized portion should be lipid soluble. Only non-ionized fraction of drugs (acids or bases is absorbed The fraction of drug remaining unionized is a function of both Dissociation constant (pKa) and pH of solution. HENDERSON HASSELBATCH EQUATION For acid, For base, pKa - pH = log[ Cu/Ci ] pKa – pH = log[ Ci/Cu ] Eg. Weak acid aspirin (pKa=3.5) in stomach (pH=1) will have > 99%of unionized form so gets absorbed in stomach Weak base quinine (pKa=8.5) will have very negligible unionization in gastric pH so negligible absorption Several prodrugs have been developed which are lipid soluble to overcome poor oral absorption of their parent compounds. 11 ◦ Absorption facts: Smaller molecules penetrate more rapidly. The membrane is Highly permeable to O2, CO2, NO and H2O . Large polar molecules – sugar, amino acids, phosphorylated intermediates – poor permeability. These are essential for cell function, and thus must be actively transported 12 KLECOP, Niani 13 1) Passive diffusion 2) Carrier- mediated transport a) Facilitated diffusion b) Active transport 3) PINOCYTOSIS KLECOP, Nipani 08/10/2010 14 Also known as nonionic diffusion. It depends on the difference in the drug concentration on either side of the membrane. Absorption of 90% of drugs. The driving force for this process is the concentration or electrochemical gradient. 15 Involves a carrier (a component of the membrane) which binds reversibly with the solute molecules to be transported to yield the carrier solute complex which transverses across the membrane to the other side where it dissociates to yield the solute molecule The carrier then returns to its original site to accept a fresh molecule of solute. There are two types of carrier mediated transport system: a) facilitated diffusion b) active transport 16 This mechanism driving force is concentration gradient. In this system, no use of energy is involved (down-hill transport), therefore the process is not inhibited by metabolic poisons that interfere with energy production. 17 More important process than facilitated diffusion. The driving force is against the concentration gradient or uphill transport. Since the process is uphill, energy is required in the work done by the barrier. As the process requires energy, it can be inhibited by metabolic poisons that interfere with energy production. 18 Active transport: • Carrier-mediated • Energy-dependent • Against conc gradient • Shows carrier saturation kinetics Passive transport • Energy-independent • No carrier involved • Along conc gradient • No saturation kinetics ATP ADP + Pi AH B ABH+ Carrier-mediated energy-dependent active transport Passive diffusion of a water-sol drug via aqueous channel Passive diffusion of a lipid-sol drug This process is important in the absorption of oil soluble vitamins & in the uptake of nutrients. 20 the proportion of the drug in a dosage form available to the body Fraction of a drug reaching systemic circulation in chemically unchanged form after a particular route First pass metabolism, i.e., rapid hepatic metabolism, reduces bioav. (lidocaine, propranolol, nitrates) Drug solubility Chemical instability in gastric pH (penicillin G, insulin) Drug formulation: Standard & SR formulations Serum Concentration Bio = AUC oral/AUC IV x 100 Injected Dose Oral Dose Time 22 Therapeutic success of a rapidly & completely absorbed drug. Plasm a Minimum effective conc. Therapeutic failure of a slowly absorbed drug. Drug Conc. Not only the magnitude of drug that comes into the systemic circulation but also the rate at which it is absorbed is important this is clear from the figure. Subtherapeutic level Time 23