and partition coefficient
advertisement

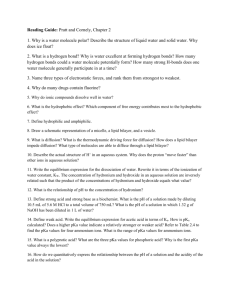
CH3 H3C CH3 + N N HO O Morphine OH HO O Inactive CH3 CH2CH=CH2 N OH AcO O N OAc Heroin (more potent) HO O OH Nalorphine(morphine antagonist) Physicochemical properties and Pharmacokinetics of the drug Some of the physicochemical properties that affect drug action are partition coefficient, dissociation constant, steric factors, solubility, polymorphism…etc. Storage sites Parentral route Site of action GIT Circulation Metabolism Excretion Physicochemical properties affect Absorption Distibution A D M E Metabolism Excretion Route of Administration Local activity only Intramuscular or Subcutaneous Injection Oral Gastrointestinal tract Tissue Depots DRUG DRUG DRUG DRUG Topical Administration Intravenous Injection DRUG Systemic circulation Drug Serum Albumin + First Pass Effect Lipid Membranes Drug Metabolites Drug Metabolites Enterohepatic Recirculation Primarily the Liver produces Drug Metabolites Route of Metabolism Bile Duct Intestinal Tract Kidney Feces Urine: Drug & Drug Metabolite Receptors for desired effects Receptors for undesired effects Pharmacology Route of Elimination •Routes of administration: 1- Parentral route: In case of IV, intra-arterial or intraspinal routes there are no absorption barriers; while in case of IM, SC, intradermal or intraperitoneal routes, the drug has to pass some membrane barriers till it reaches the circulation. 2- GIT route: The drug has first to come into solution before it can be absorbed from the GIT. This is affected by the pH of the part of GIT from which the drug is absorbed (stomach pH 1-3.5, duodenum pH 6-7, lower ileum pH 8), and the dissociation rate (pKa) of the drug at that pH. i) Particle size: The smaller the particle size of the drug powder, the greater will be the surface area exposed to the fluids of the GIT and the faster will be the dissolution. Spironolactone and griseofulvin are drugs that were reformulated in ‘micronized’ forms to improve their bioavailability. ii) The pH of the medium: Weakly acidic drugs are better dissolved in the alkaline regions of the GIT and the opposite holds true for weakly basic drugs. Drug absorption a) Active transport or carrier mediated transport where energy is required because transport of the drug occurs against concentration gradient. Also, there should be some structural similarity between the drug and the substrate normally carried across the membrane. b) Passive diffusion where the movement of the drug occurs following concentration gradient i.e. from high concentration to low concentration. The rate of diffusion is proportional to the drug concentration on the other side of the membrane. Where –dC/dt is the rate of diffusion and C1 is the concentration of the drug at the site of absorption and K is proportionality constant depending on the area and thickness of the membrane, and the partition coefficient of the drug. c) Convective absorption where small molecules of molecular radius less than 4Ǻ pass through water filled pores in the biological membrane. Conjugate Acid - Base For an acid (ex. R-COOH) HA Conjugate Acid R-COOH H+ + A- Conjugate base R-COO- For a base (ex. R-NH2) BH+ Conjugate Acid R-NH3+ H+ + B Conjugate base R-NH2 Effect of dissociation constant (pKa) and partition coefficient (logP) on drug absorption i) Dissociation constant (pKa): For acids: RCOOH = RCOO- + H+ If pKa > pH unionized acid has the greater concentration e.g. pKa=3; pH=1 i.e. unionized =99% and ionized =1% i.e. unionized =90% and ionized =10% If pKa < pH ionized acid will prevail. e.g. pKa=1; pH=7 i.e. unionized =0.0001% and ionized =99.9999% Drug Transfer – Acidic Drugs Acidic Drug "A" - Primary absorption in the stomach Blood HA pH = 7.4 H2O + A- Lipid Membrane pH = 1-2 HA Stomach H3O+ + A- Example: Aspirin - Acetylsalicylic acid CO2H CO2Water O O + H3O+ O CH3 O CH3 pKa = 3.5------The pH at which you have 50% unionized and 50% ionized forms of the molecule. Drug Transfer – Acidic Drugs Acidic Drug "A" - Little absorption in the small intestine Blood HA pH = 7.4 H 2O + A- Lipid Membrane pH = 8-9 HA Small intestine H 2O + A- Example: Aspirin - Acetylsalicylic acid CO2H CO2Water O O + H3O+ O CH3 O CH3 pKa = 3.5---------@ pH = 4.5 - 90.0% in ionized form @ pH = 5.5 - 99.0% in ionized form For bases: RNH3+ = RNH2 + H+ If pKa > pH ionized base will prevail. i.e. ionized=99% and unionized=1% If we know that the unionized form of the drug is the lipid soluble form and therefore is the absorbable form, then we can conclude that weak acids will exist in the stomach mostly in the unionized form so they are mainly absorbed from the stomach. So are weak bases which exist in the small intestine in unionized form they will be absorbed mainly from the intestine. In fact, there is always equilibrium between the unionized and ionized forms of the drug. When part of the unionized species is absorbed, some of the ionized forms get converted into the unionized forms to restore equilibrium. The latter will in turn be absorbed and the process continues. Drug Transfer – Basic Drugs Basic Drug "B" - Little absorption in the stomach Blood BH+ pH = 7.4 H2O + B Lipid Membrane pH = 1-2 BH+ Stomach H3O+ + B Example: Pseudoephedrine HCl HO Cl+ NH2CH3 H CH3 H HO Water H NHCH3 H + HCl CH3 Pseudoephedrine HCl pKa = 9.9------The pH at which you have 50% unionized and 50% ionized forms of the molecule. Drug Transfer – Basic Drugs Basic Drug "B" - Primary absorption in the small intestine Blood BH+ pH = 7.4 H 2O + B Lipid Membrane pH = 8-9 BH+ Small intestine H 2O + B Example: Pseudoephedrine HCl HO Cl+ NH2CH3 H CH3 H HO Water H NHCH3 H + HCl CH3 Pseudoephedrine HCl pKa = 9.9---------@ pH = 8.9 - 90.0% in ionized form @ pH = 7.9 - 99.0% in ionized form % Ionized vs. pH For HA acids: % ionization = 100/(1 + 10(pKa – pH)) For BH+ acids: % ionization = 100/(1 + 10(pH – pKa)) Example: Percentage ionized pseudoephedrine HCl (pKa 9.9) in the small intestine at pH 8.0? % ionization = 100/(1 + 10(8.0– 9.9)) % ionization = 100/(1 + 0.0126) % ionization = 100/1.0126 % ionization = 98.76% pH Effects on Absorption Acids 5-nitrosalicylic acid Salicylic acid Thiopental Bases Quinine Dextromethorphan pKa % absorbed at pH1 % absorbed at pH8 2.3 3.0 7.6 52 61 46 16 13 34 8.4 9.2 0 0 18 16 ii) Partition coefficient (logP): Where, Co is the concentration of drug in organic phase (n-octanol) , and Cw is its concentration in aqueous phase (water). The presence of the drug in the unionized form does not guarantee that it will be absorbed from the GIT. The lipid solubility of the unionized form is also a ruling factor. This is because of the composition of biological membranes which is mainly lipid in nature; therefore solubilization of the drug in the membrane is a must for absorption to occur. Barbital and secobarbital which have similar pKa values, 7.8 and 7.9, respectively have partition coefficients 0.7 and 23.3, respectively. So it can be expected that secobarbital is better absorbed than barbital although both drugs have the same percentage of unionized form under the same condition. Accordingly, one can modify a drug to improve its lipid solubility through the introduction of hydrophobic groups. The hydrophobicity constants (π) of various chemical groups are available in tables so that one can select the proper group according to its π value and estimate the partition coefficient of the modified drug. Ph C2H5 O HN NH O C2H5 O H13C6 O HN NH C2H5 O O HN NH O O S Phenobarbital Hexethal Thiopental On the contrary, it might be useful to decrease the lipophilicity of a drug so as to prevent its absorption from the GIT and therefore localize its effect in the GIT as in the case of intestinal sulfonamides (sulfaguanidine and succinyl sulfathiazole) NHCOCH2CH2COOH NH2 N NH SO2NH SO2NH NH2 Sulfaguanidine S Succinyl sulfathiazole •Sites of loss: 1- Protein binding: Binding of drugs to plasma protein depends mainly on the chemical structure of the drug. The bound drug is a large complex incapable of performing any biological process (no metabolism, no excretion, no interaction with receptors..etc.). So, the plasma protein binding can be regarded as storage site for the drug from which the drug is gradually released according to the equilibrium existing between the free and bound drug. This, in some cases, contributes to the long duration of action of some drugs. Also, protein binding protects the drug, to some extent, from rapid metabolism and excretion. 2- Neutral fat: Deposition of drugs into the adipose tissue depends largely on the partition coefficient and pKa of the drug, so that lipophylic unionized drugs are expected to partition rapidly into neutral fat. Drugs stored in the adipose tissue will eventually be released into the circulation to exert their action. 3- Excretion: Drugs of suitable size to pass the glomerular membranes and that are soluble enough in aqueous medium at the pH of urine are expected to be excreted in the urine. 4- Metabolism: this is discussed in a separate part. Quantitative Structure Activity Relationship (QSAR) The relation of one physicochemical parameter with biological activity can be quantified; and this holds true for other parameters so that a generalized equation can be developed to correlate activity to the physicochemical properties of a given drug. In QSAR, an additive mathematical model is developed in which it is assumed that a certain substituent in a specific position contributes additively to the biological activity of the molecule. Substituent hydrophobicity effect Substituent electronic effect Steric factors 1- Partition coefficient and Hansch substituent hydrophobicity constant (π): Increase in PC result in improvement in pharmacokinetics and distribution of the drug. log 1/C 12 log 1/C 12 10 10 8 8 6 6 X 4 2 √ 4 2 0 0 0 5 10 log P 0 10 20 log P The reasons for this behaviour are: a) The drug may be too hydrophobic to be soluble in aqueous body fluids. b) The drug may be trapped in the fat depot and not reach the site of action. c) Hydrophobic drugs are more susceptible to metabolism and loss. Hydrophobicity of a given molecule is a sum of the hydrophobicity constants (π) of the chemical groups that constitute the molecule. This quantitative approach helps to theoretically predict the PC of a given molecule and thereby chemical modifications by replacement of some functional groups will be selected on the basis of the (π) constants of the new chemical groups. substituent O O NH O N H O NH -1.35 O N H O Amobarbital 2.30 1.00 log P=sum of How to measure π constant of a given substituent? π constant of –COOH can be calculated by the difference between PC of benzene and benzoic acid. π Cl = log P chlorobenzene – log P benzene Positive π values increase PC and negative values decrease PC. 2- Electronic effects and Hammett sigma (σ) constant: The sigma σ constant is a measure of the electronic contribution of substituents relative to hydrogen. It affects the electron density on particular regions in the molecule and thereby affects drug-receptor interactions. How to measure the δ constant of a particular group? δ = pKa of benzoic acid- pKa of substituted benzoic acid σ is positive for electron withdrawing groups e.g. CN, Cl, COOH, NO2, CF3, and negative for electron donating groups e.g. OH, OCH3, NH2, CH3. Hammett’s equation: σ is electronic Hammett constant, ρ is characteristic of the reaction considered and its selectivity to the substitution in parent compounds, K and Ko refer to the rate constants for the derivative and the parent compound. In aromatic systems, the position of substituent whether meta, ortho or para to a given group (R) will affect its electronic effect on that group. In the meta position, the effect of the substituent on (R) will be only inductive; while in the para position it will be due to both inductive and resonance effects. O OH N O INDUCTIVE EFFECT R R O O N R R O O N OH OH R R R INDUCTIVE AND RESONANCE EFFECTS